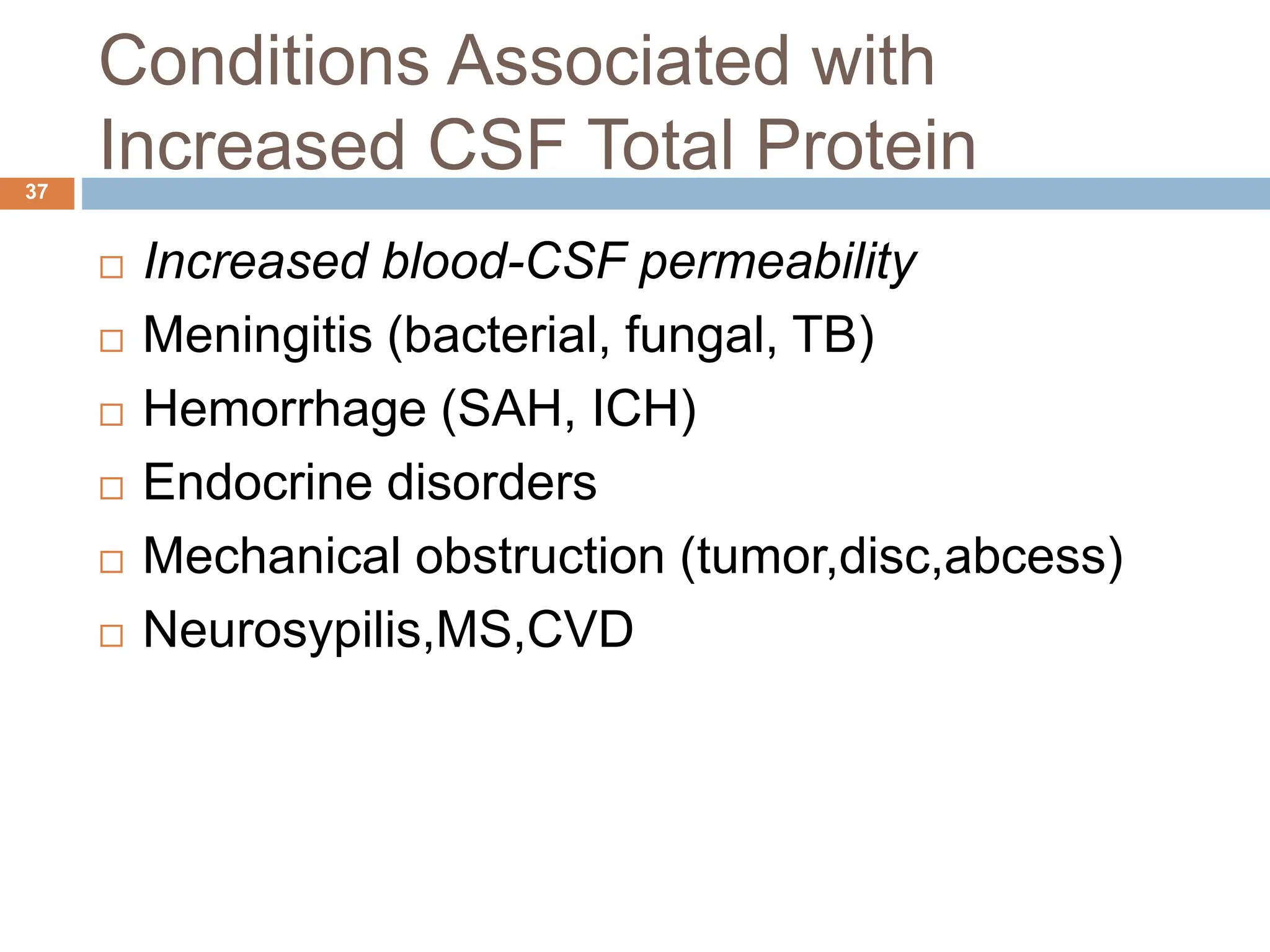
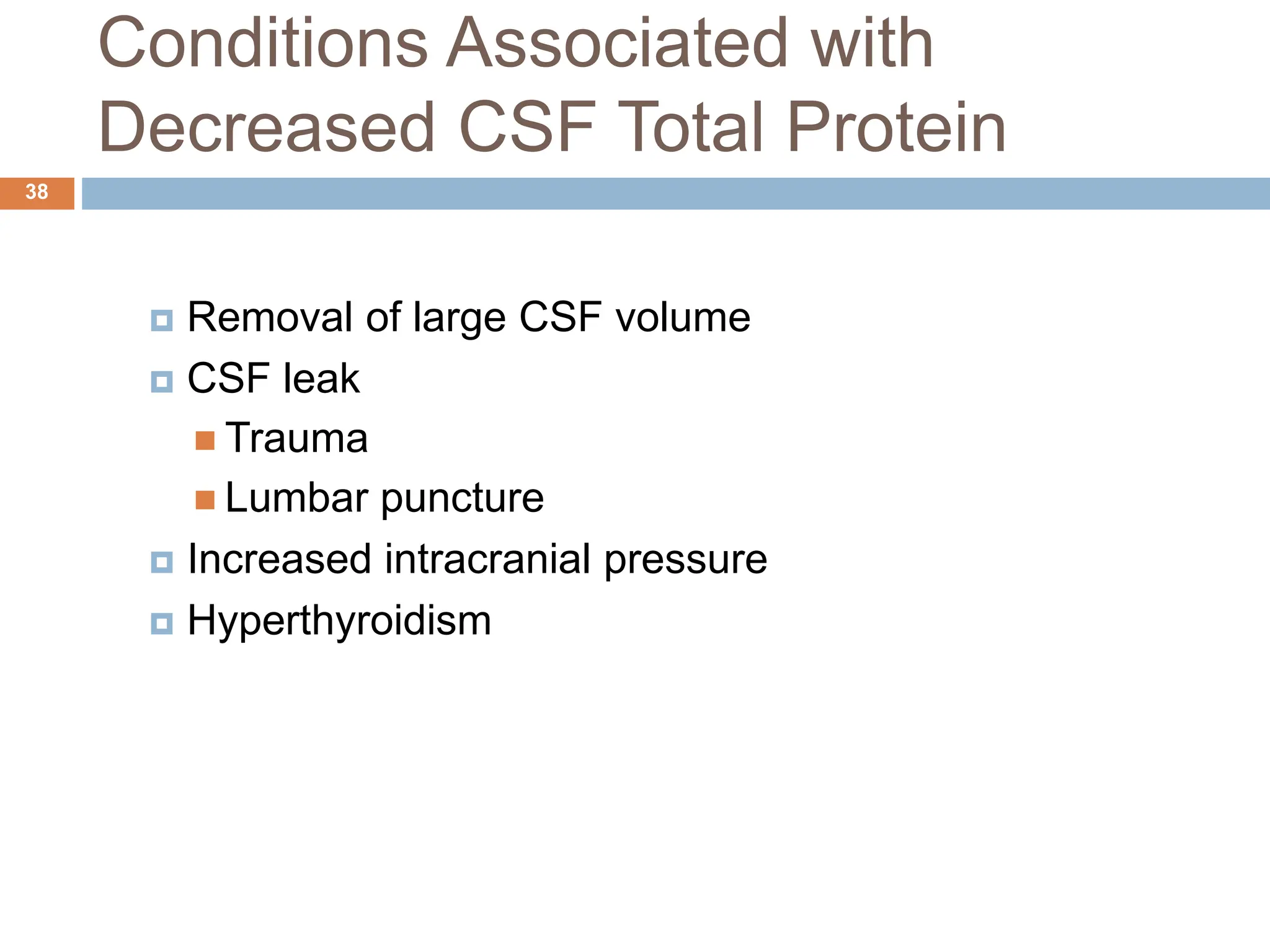
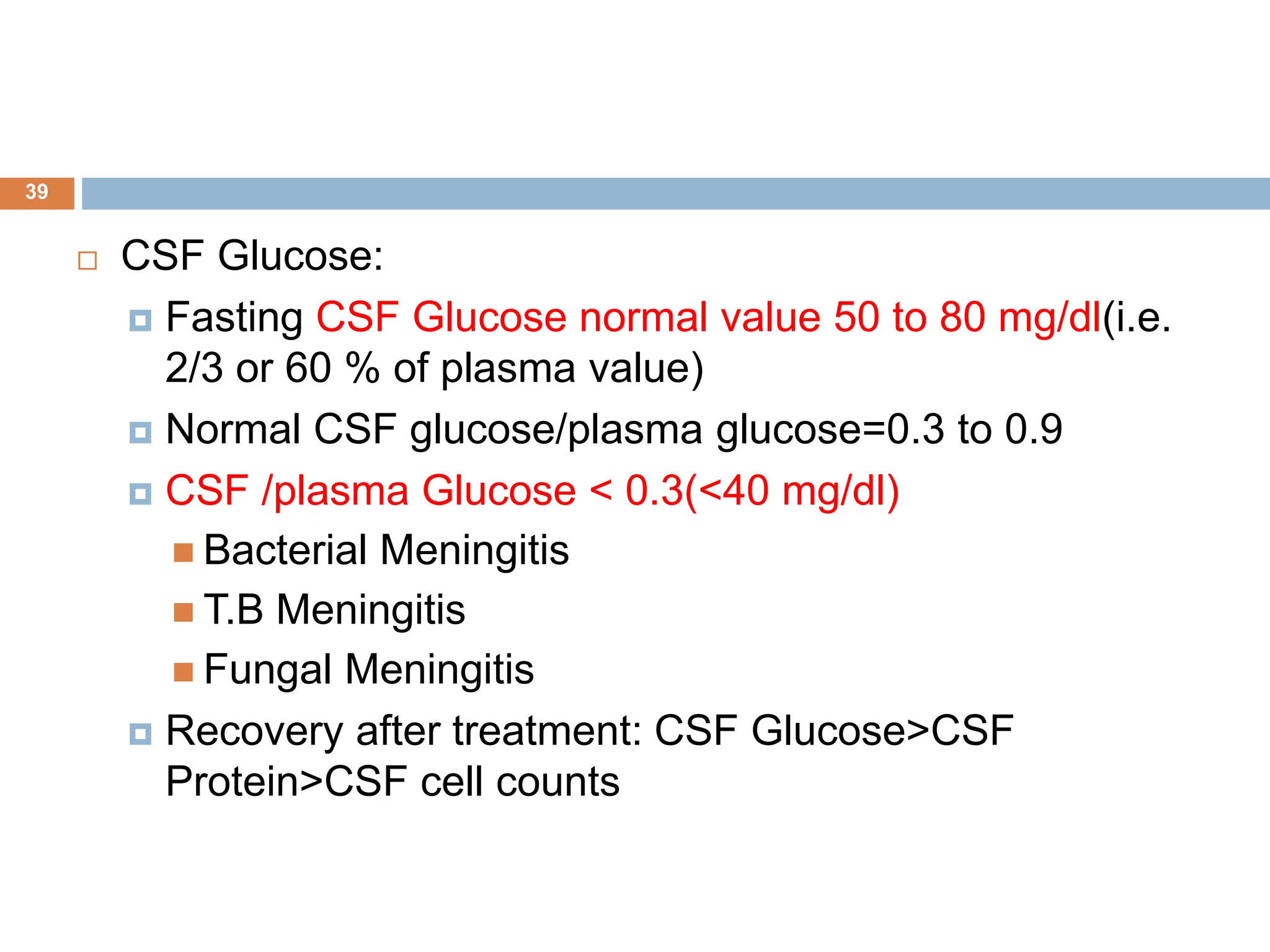
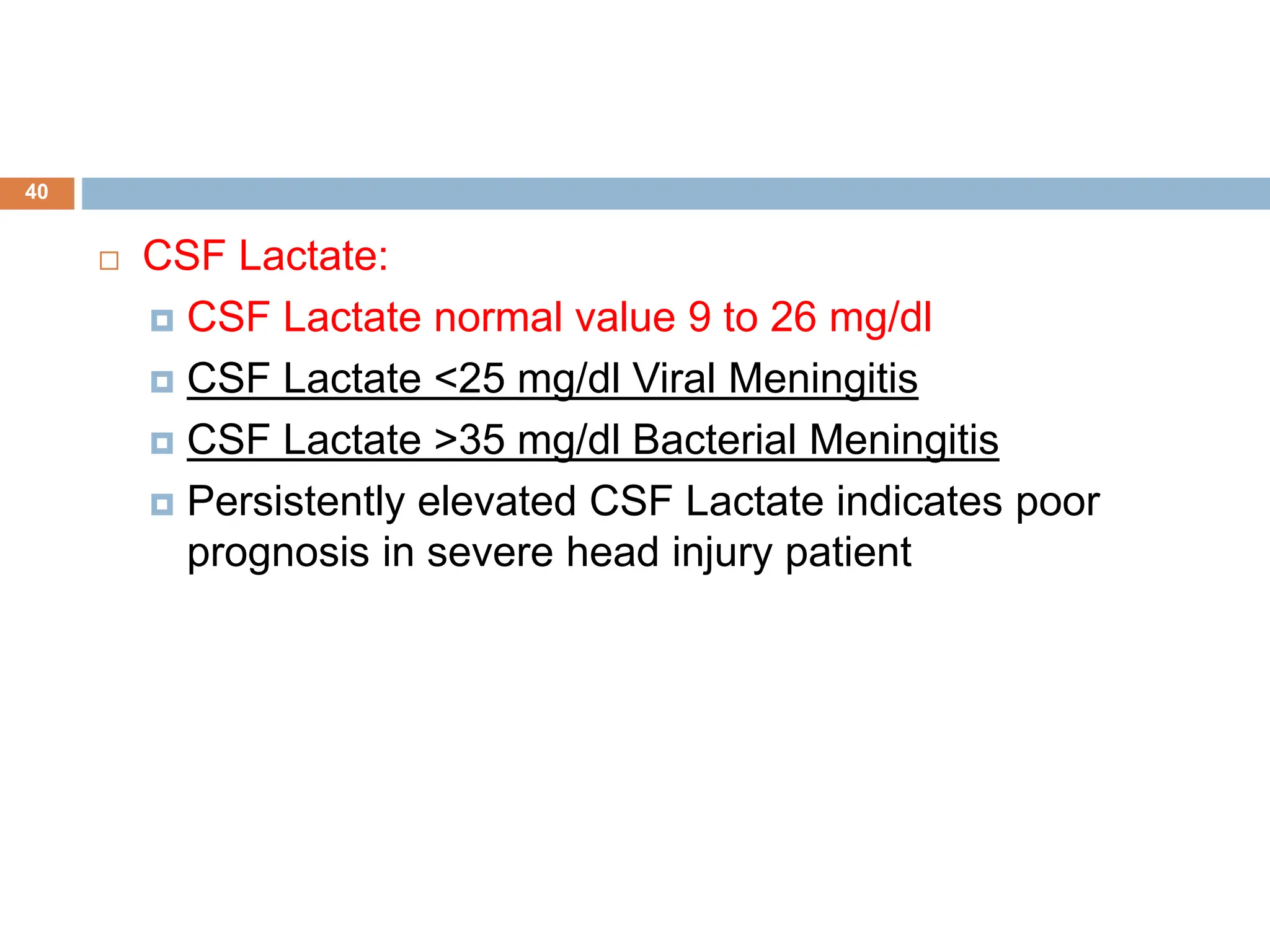
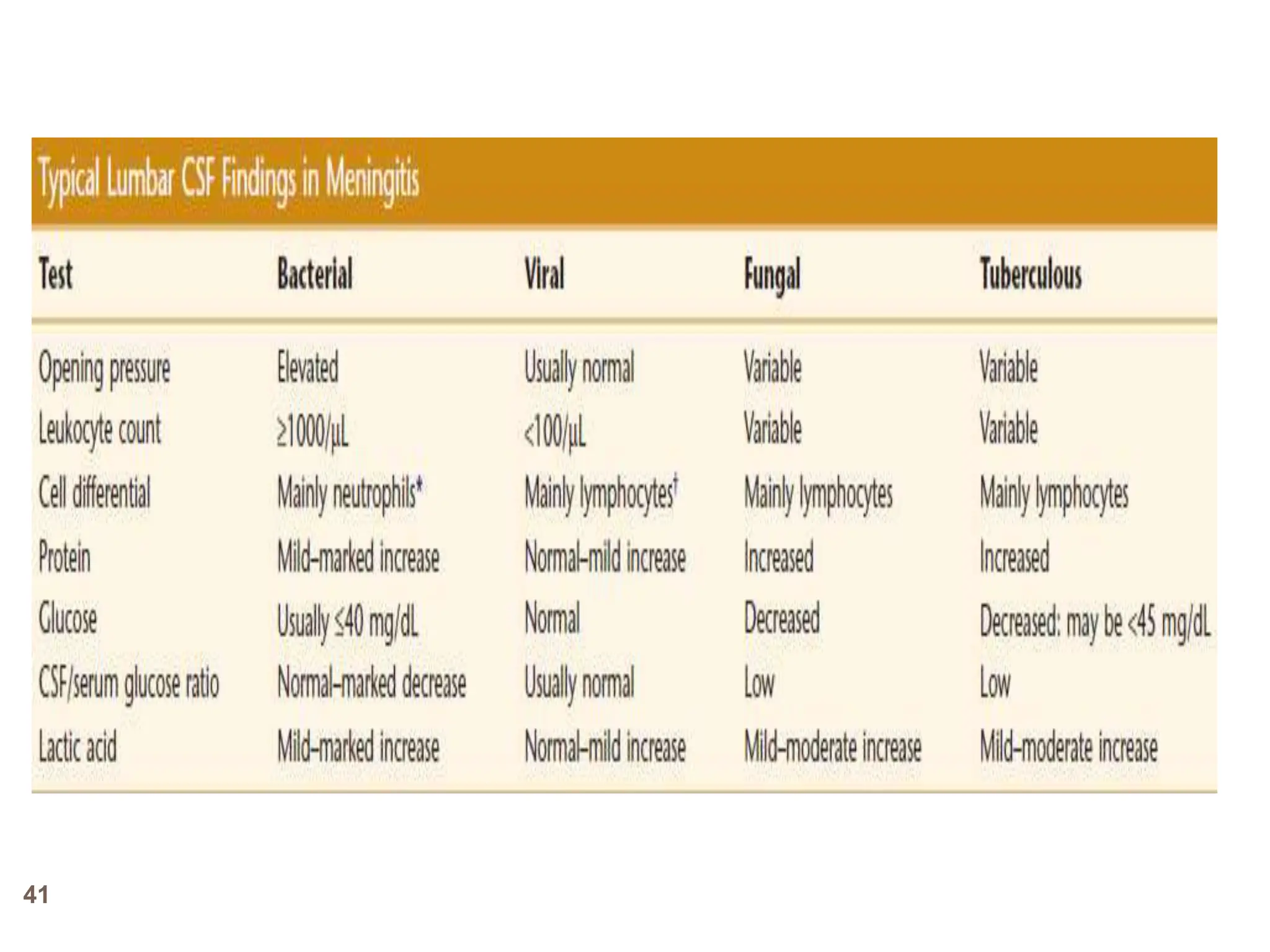
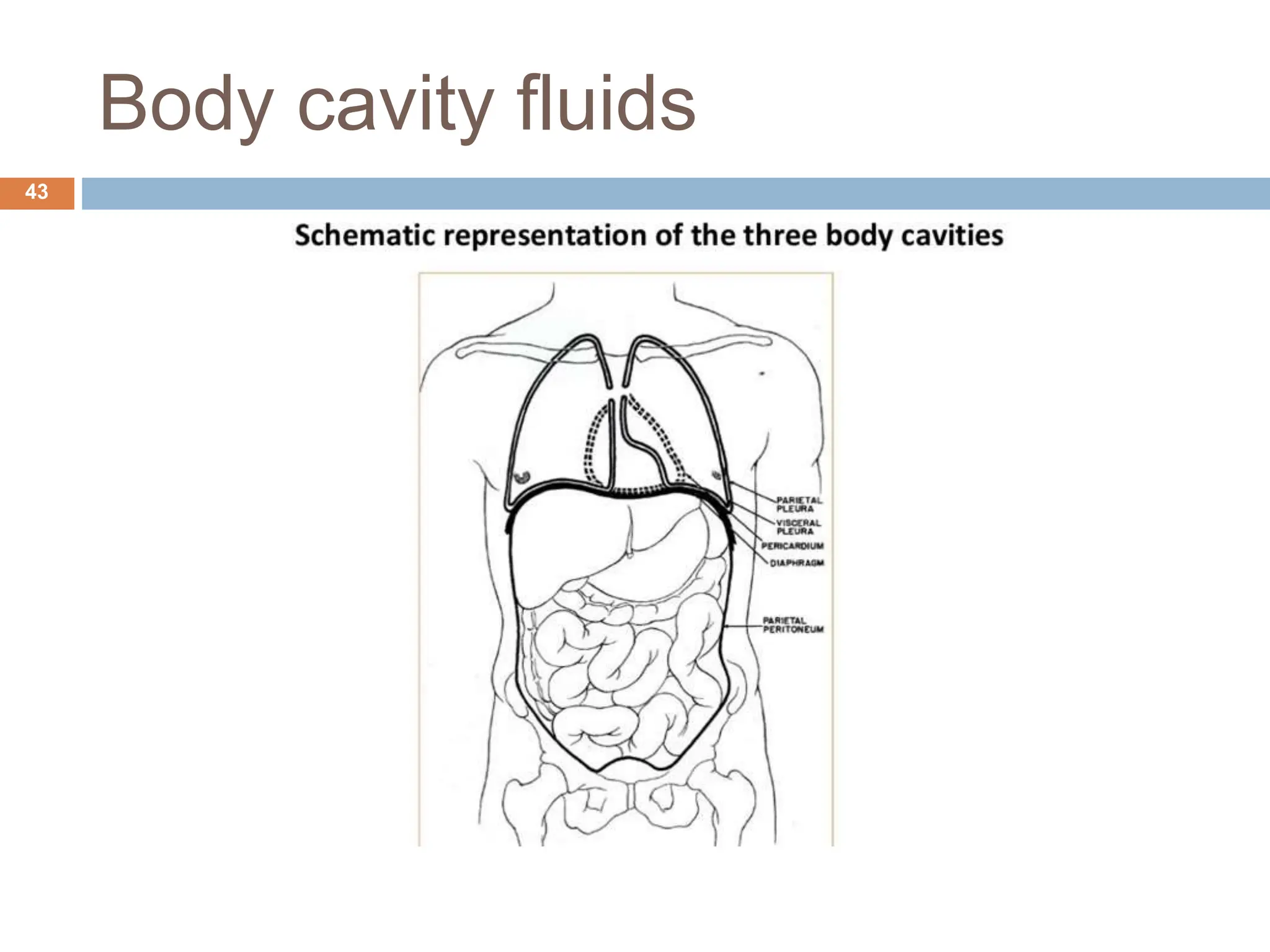
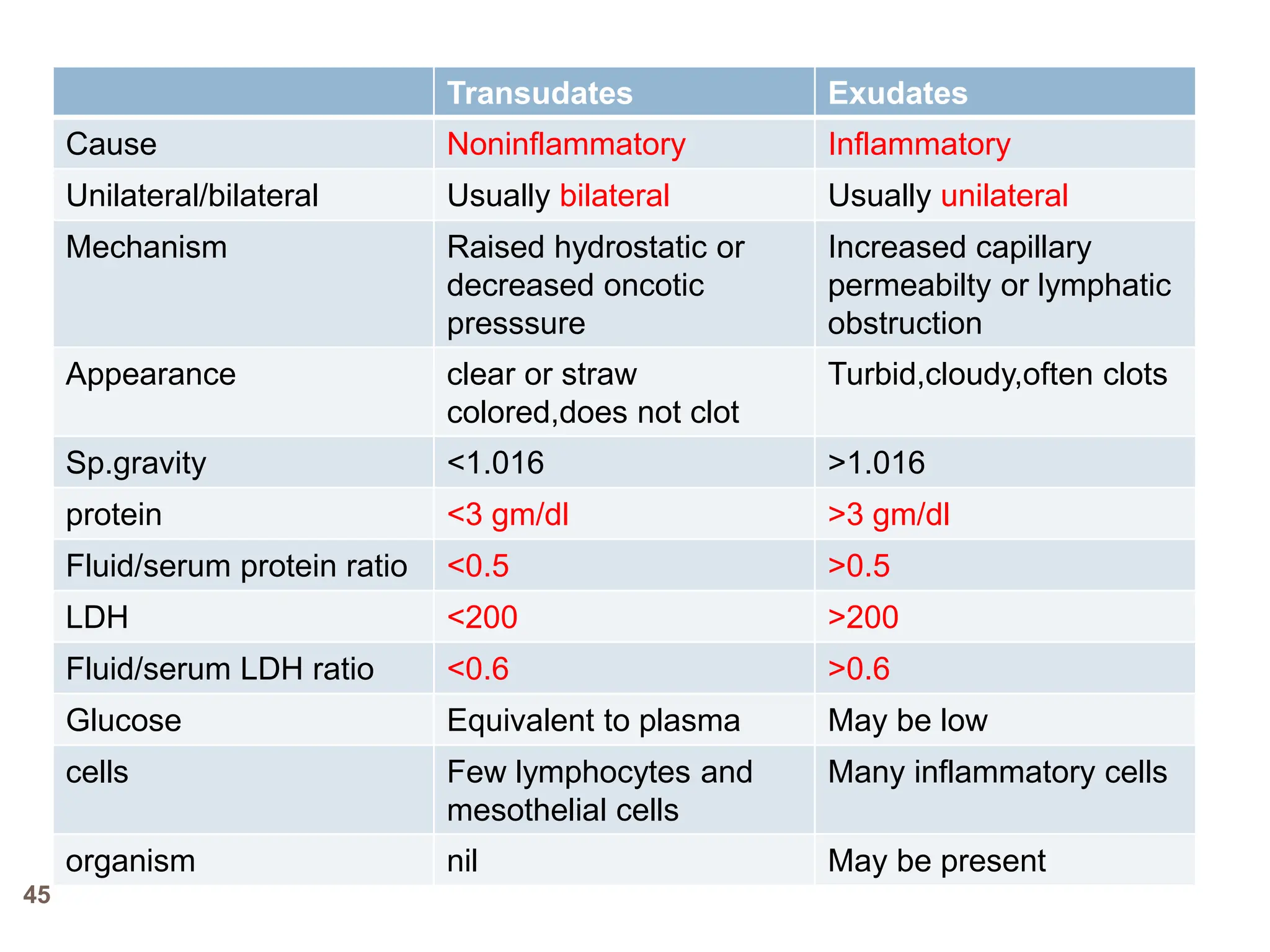
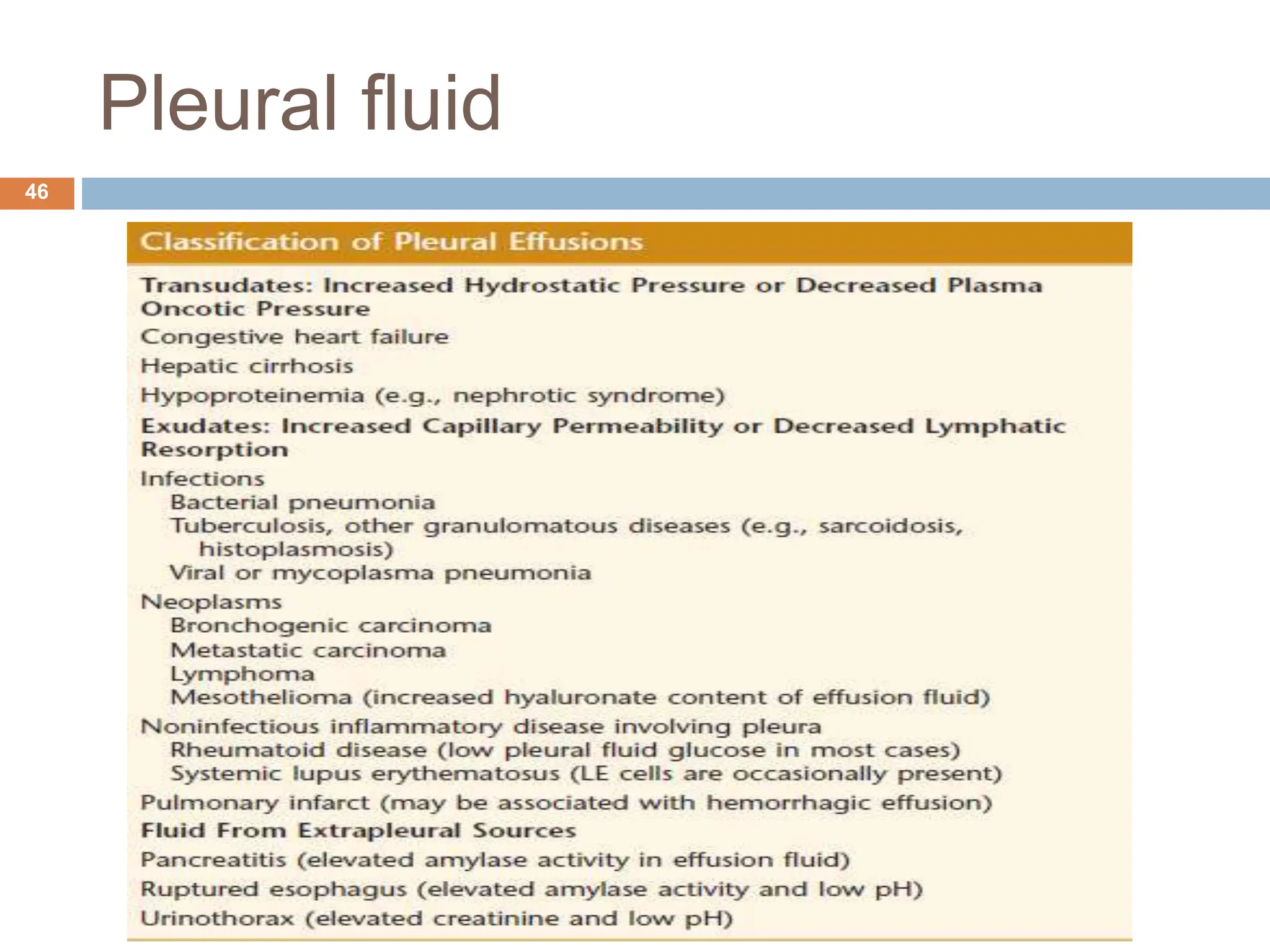
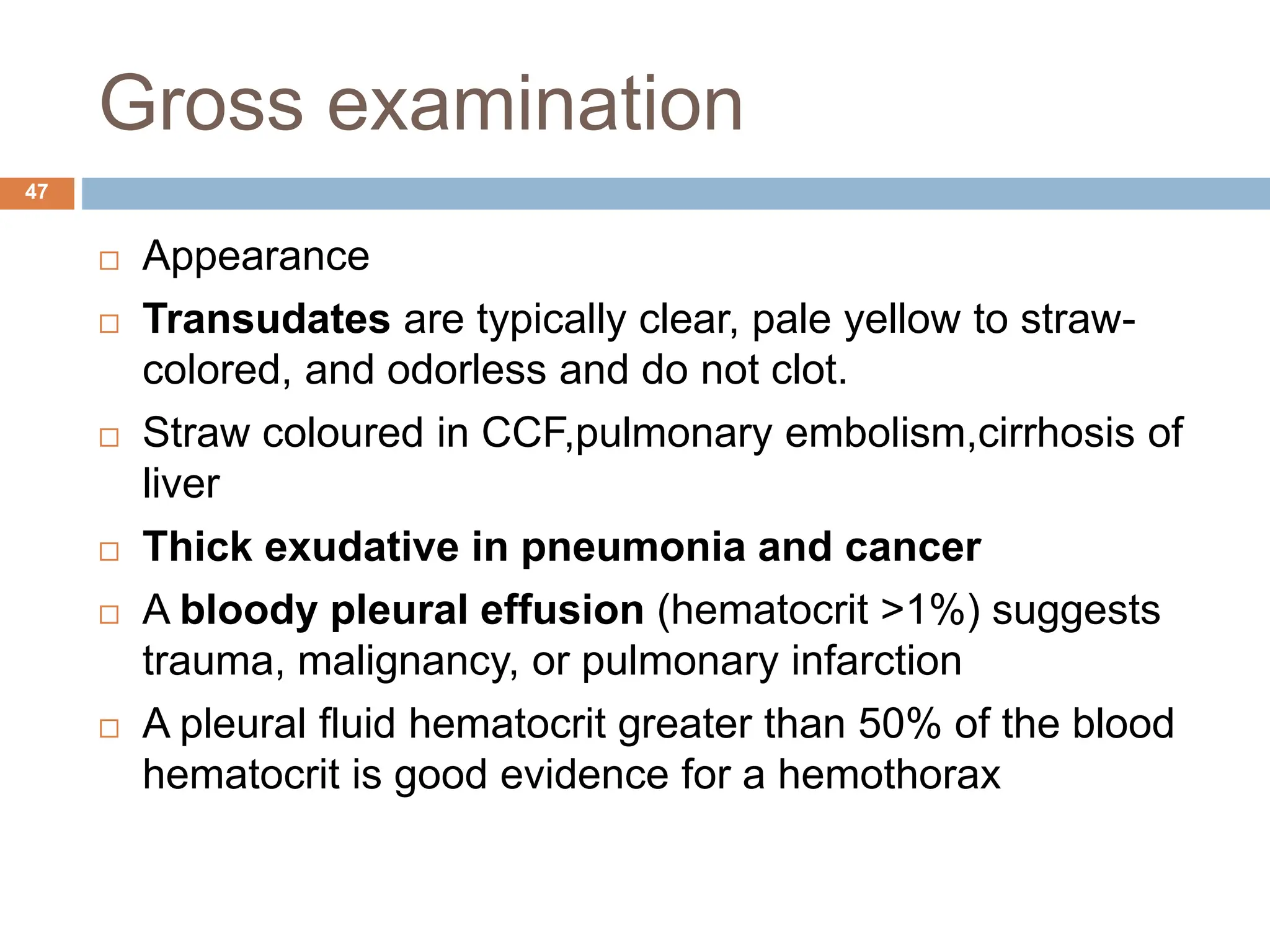
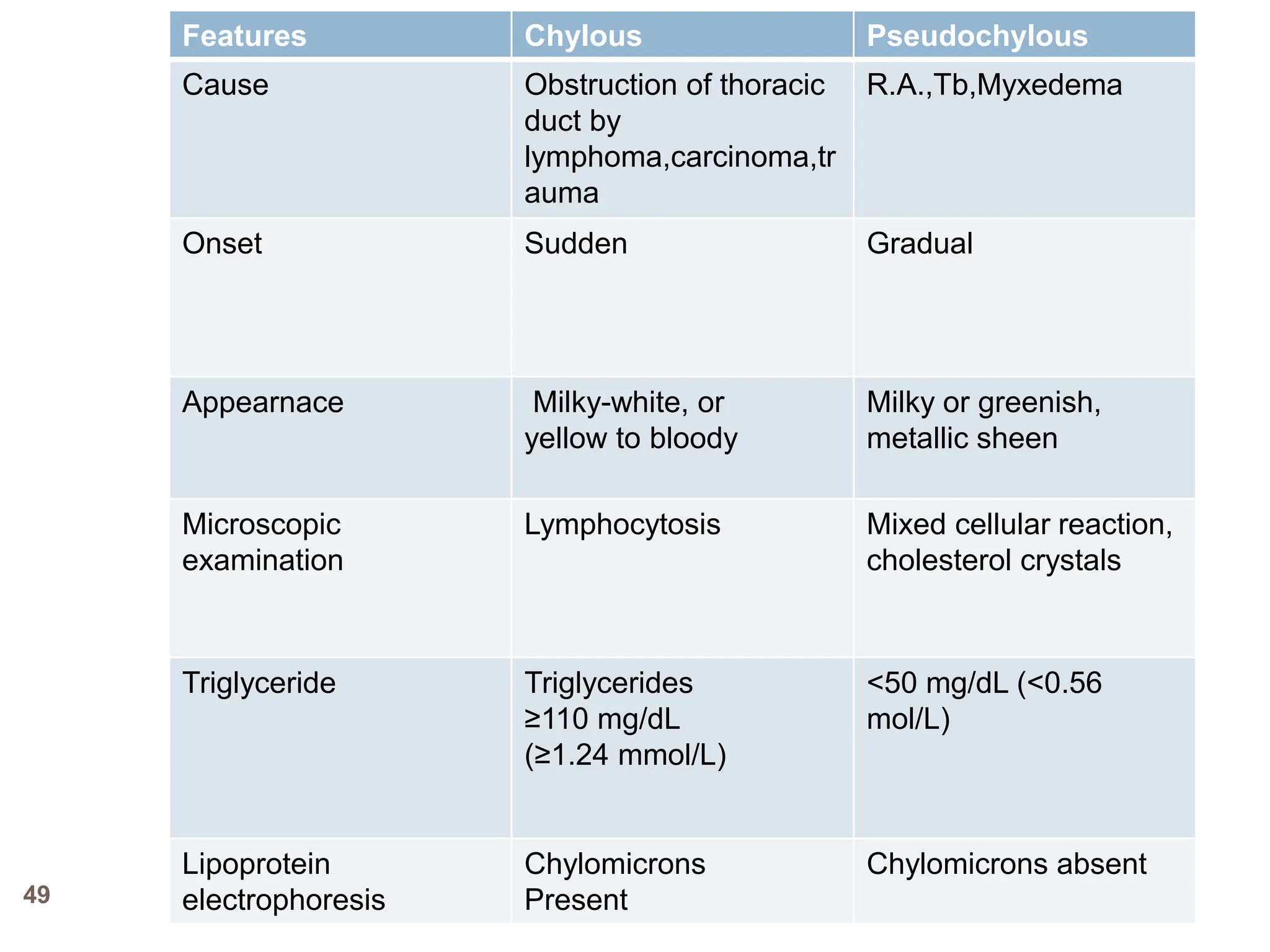
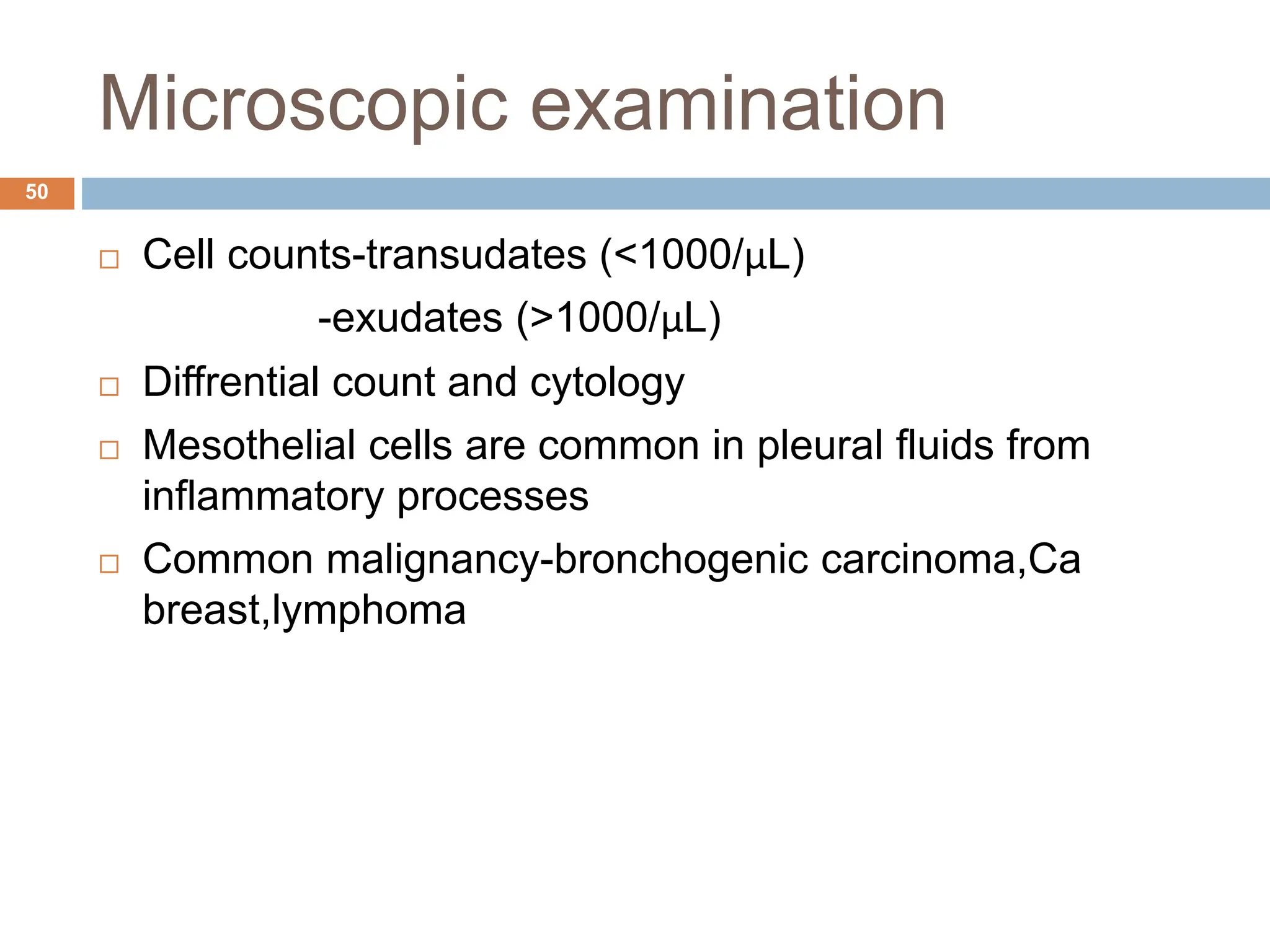
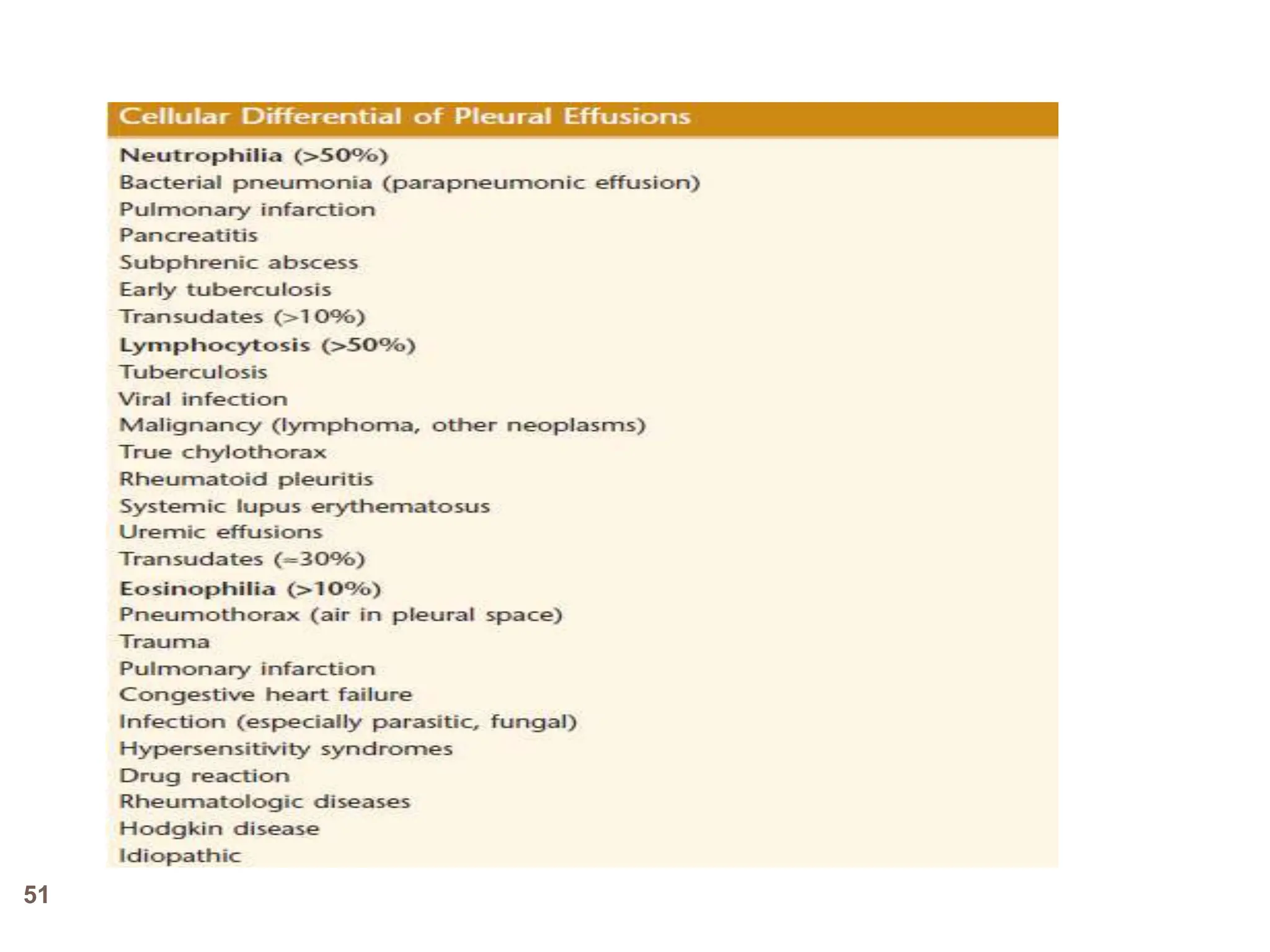
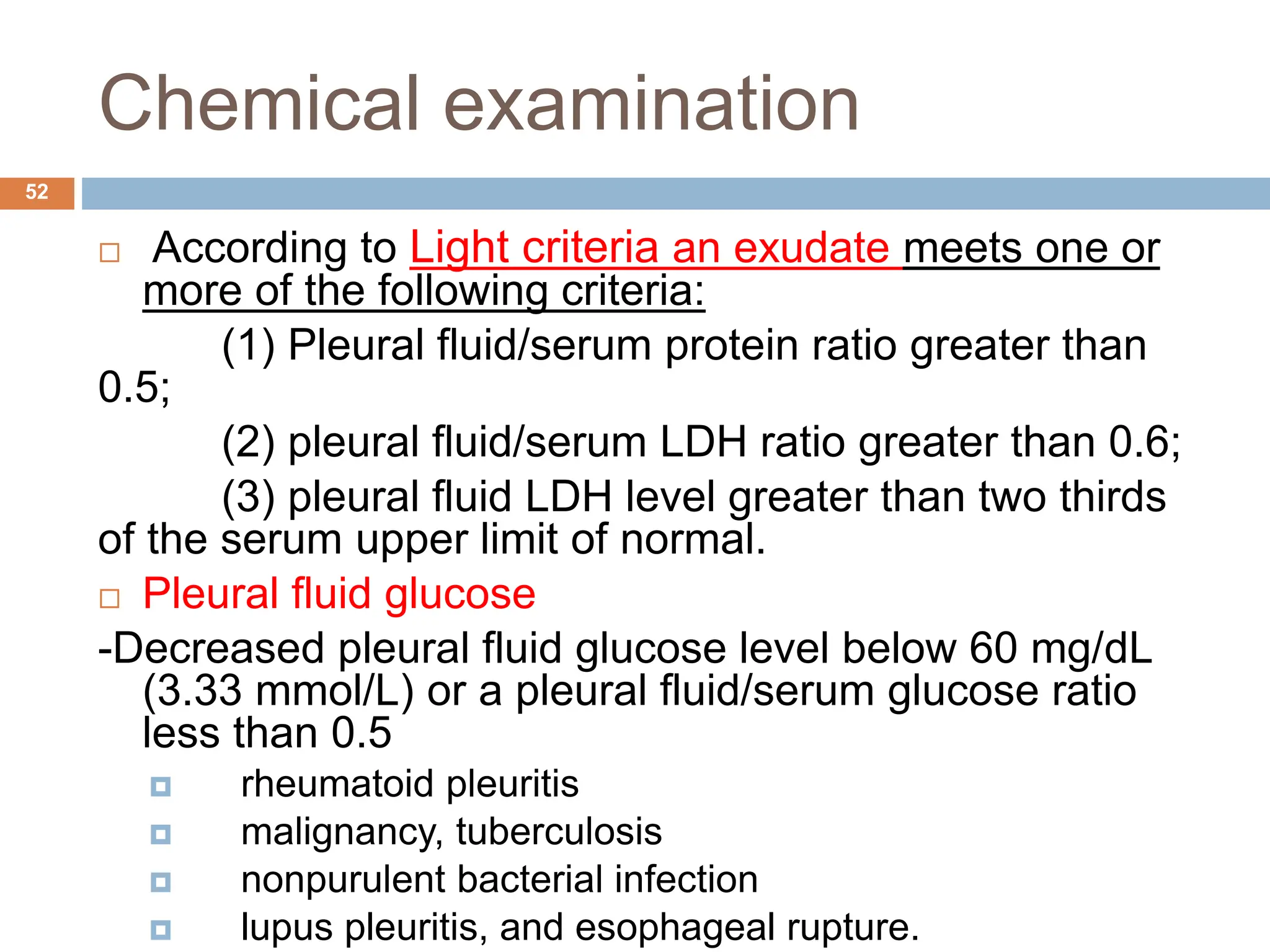
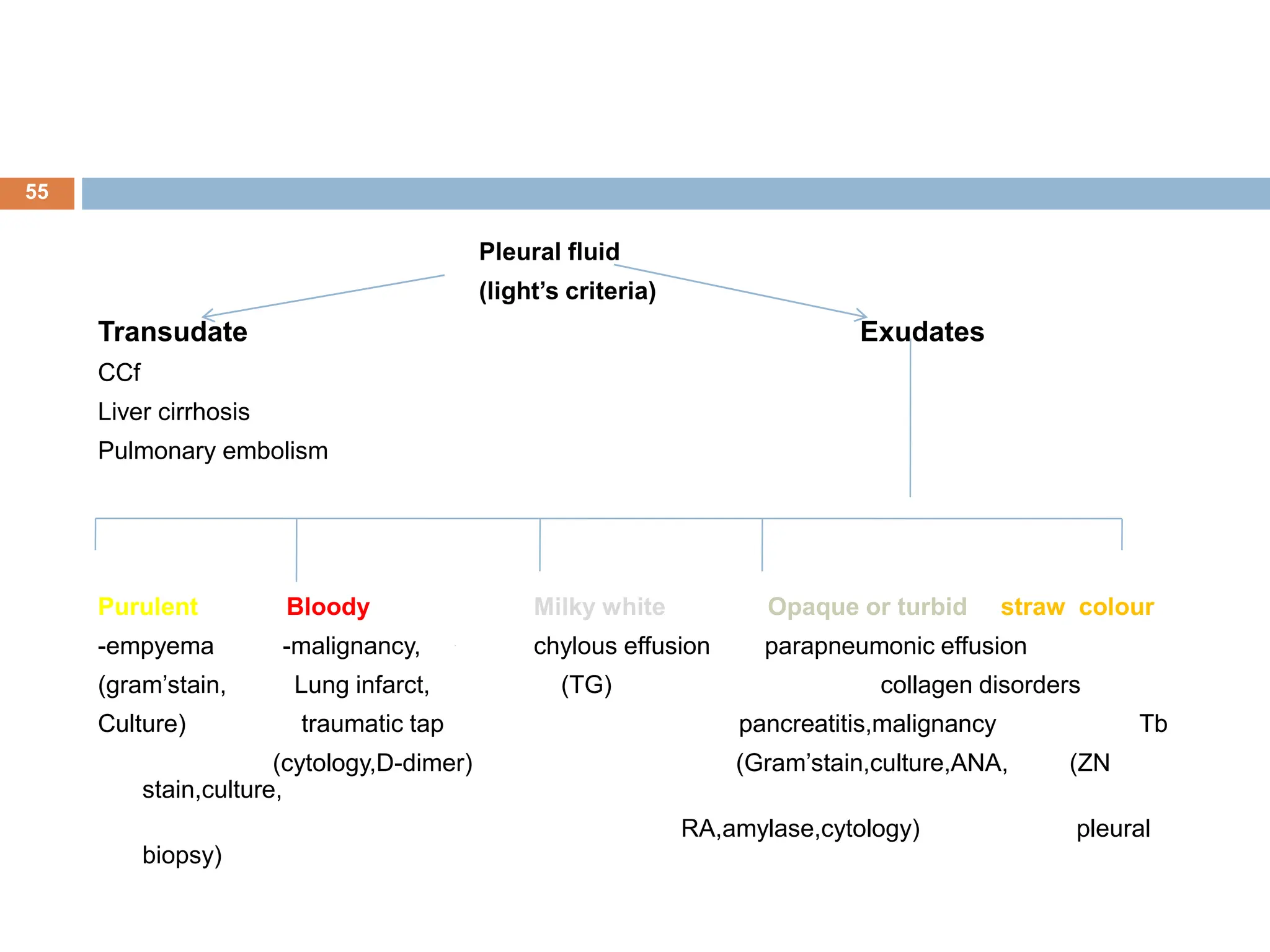
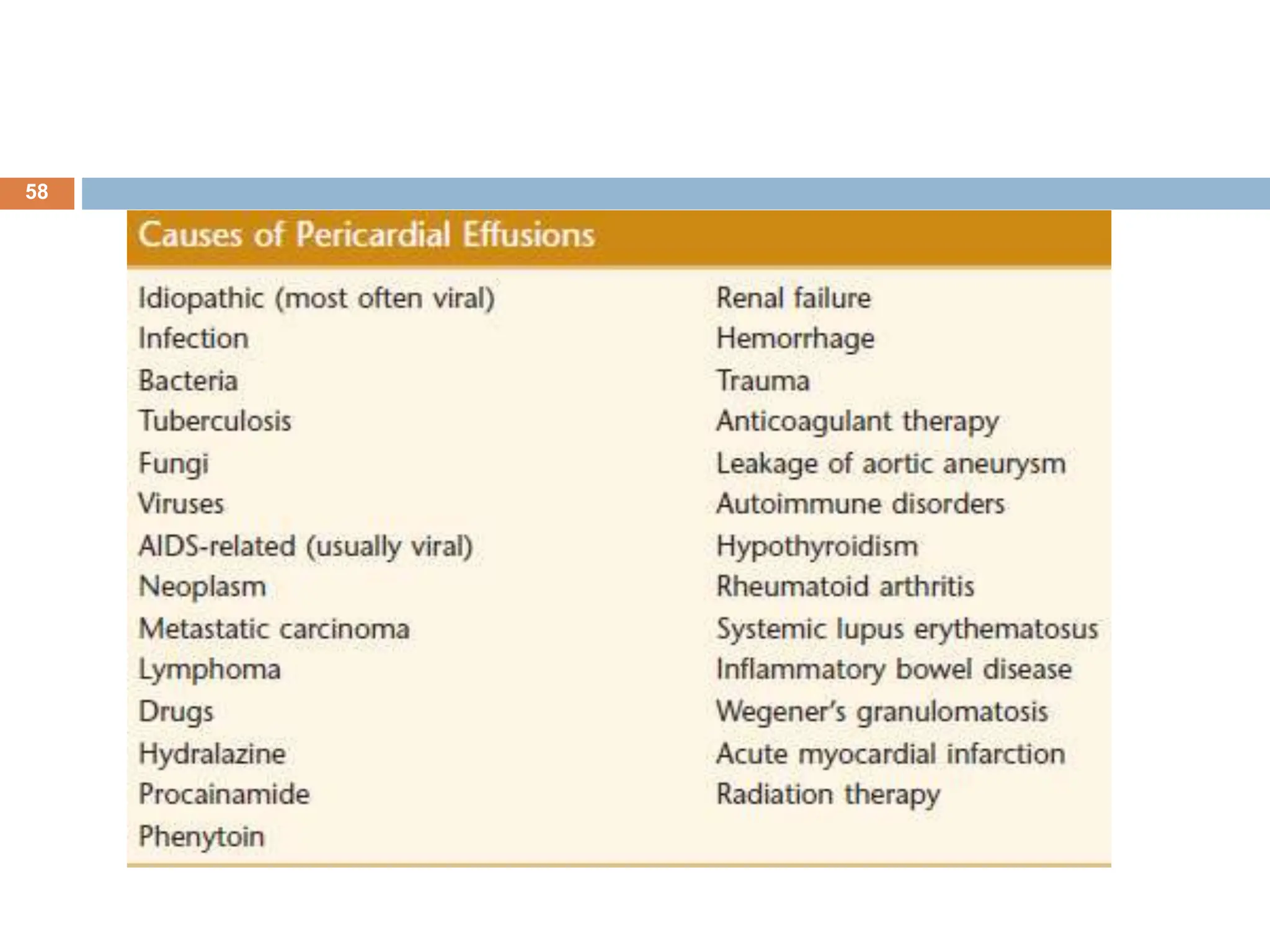
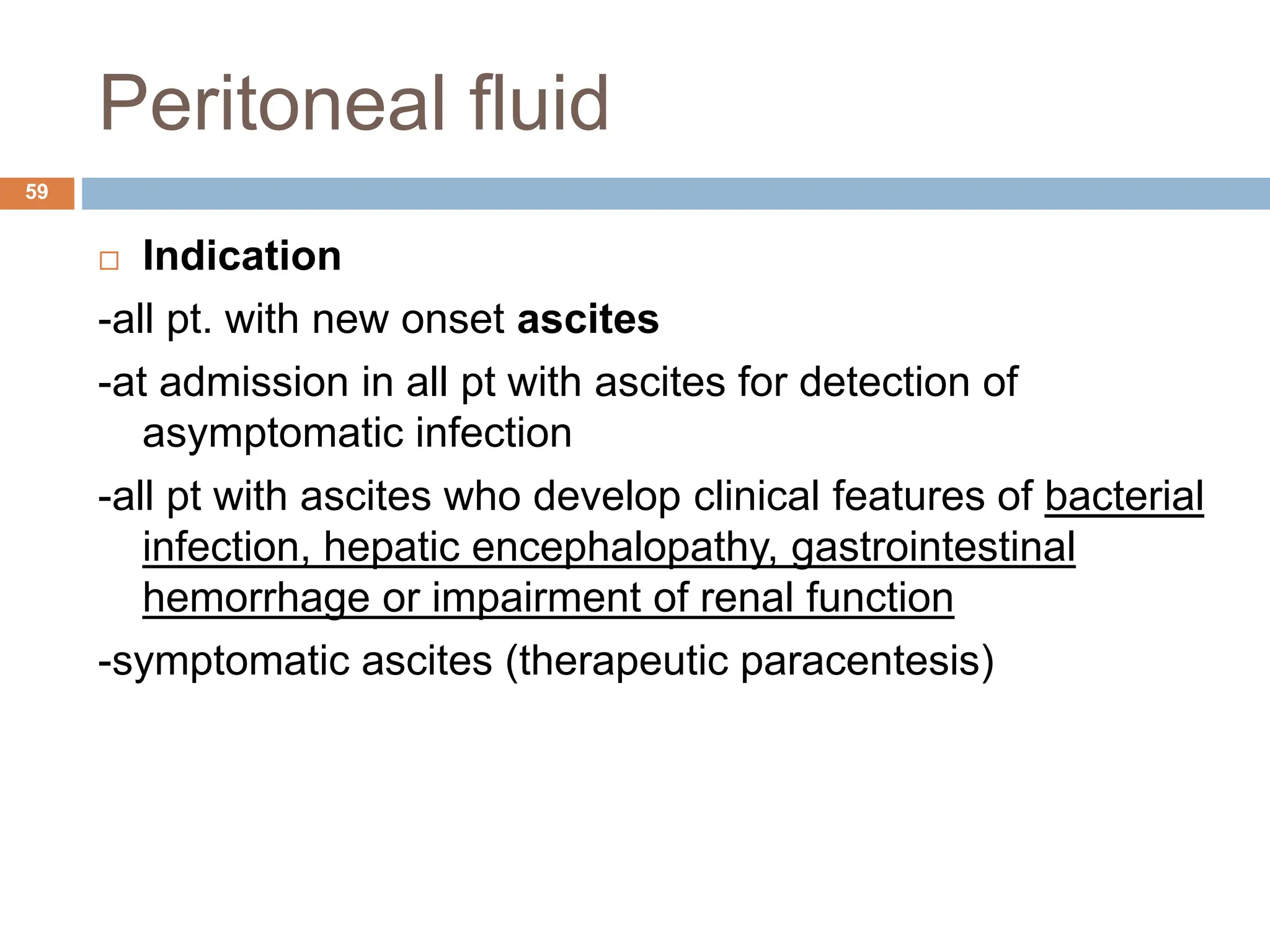
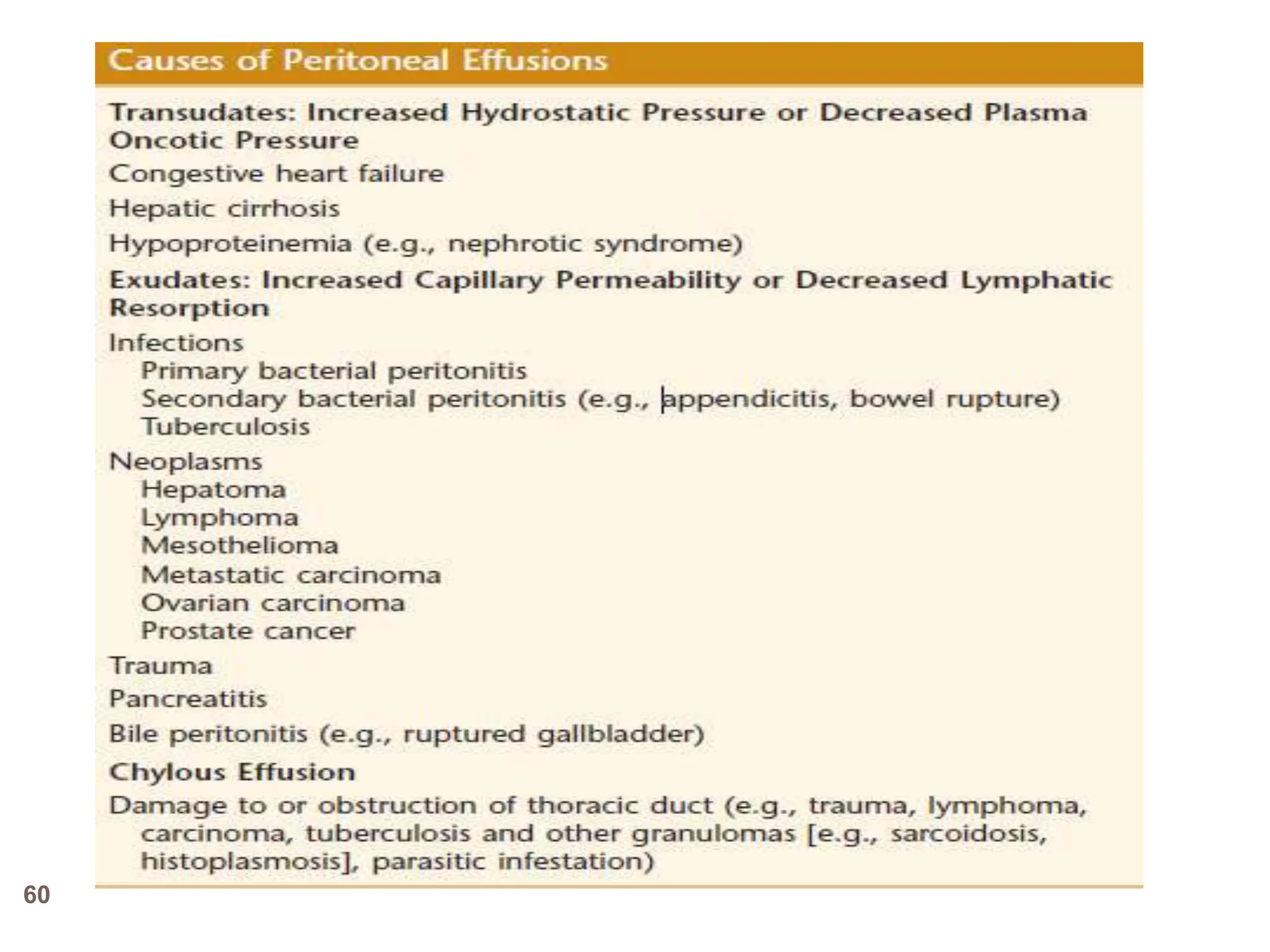
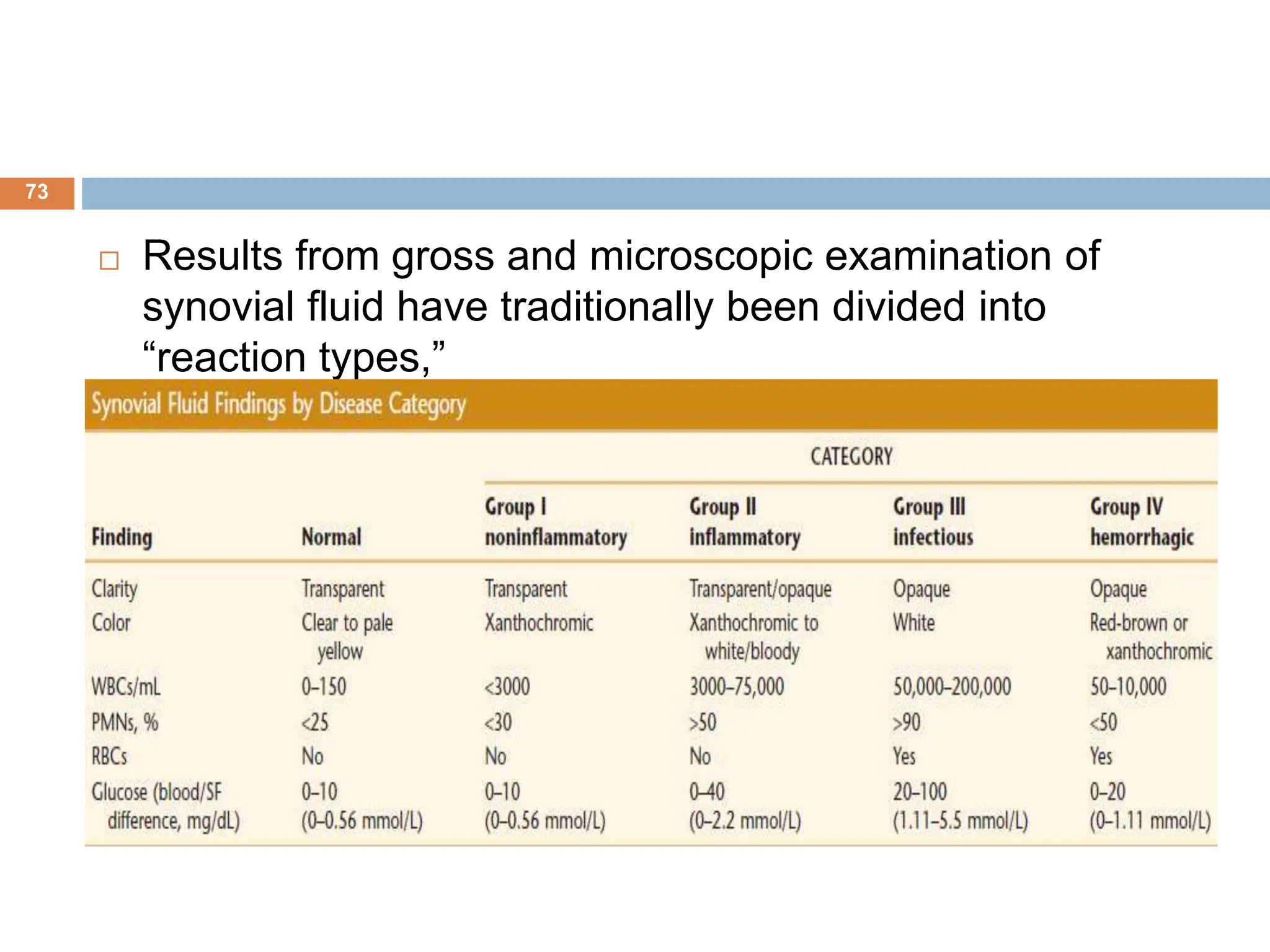
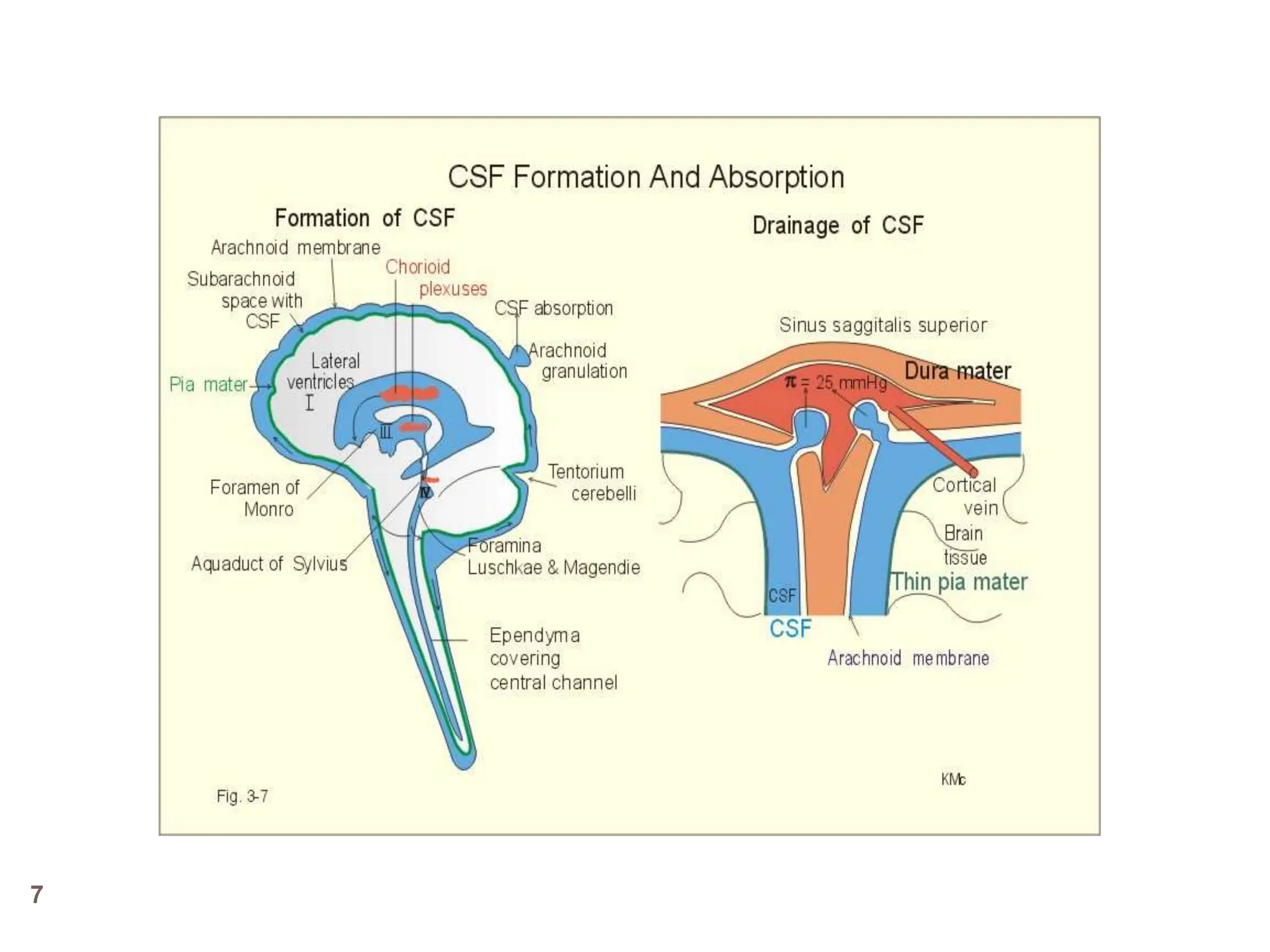
The document outlines the examination of body cavity fluids, including cerebrospinal fluid (CSF), pleural fluid, pericardial fluid, and peritoneal fluid. It emphasizes the importance of analyzing these fluids to diagnose a variety of medical conditions such as infections and malignancies, detailing procedures for specimen collection, gross and microscopic examination, as well as chemical and microbiological analysis. Key indicators for various pathologies are provided, alongside diagnostic criteria and normal values for laboratory tests.

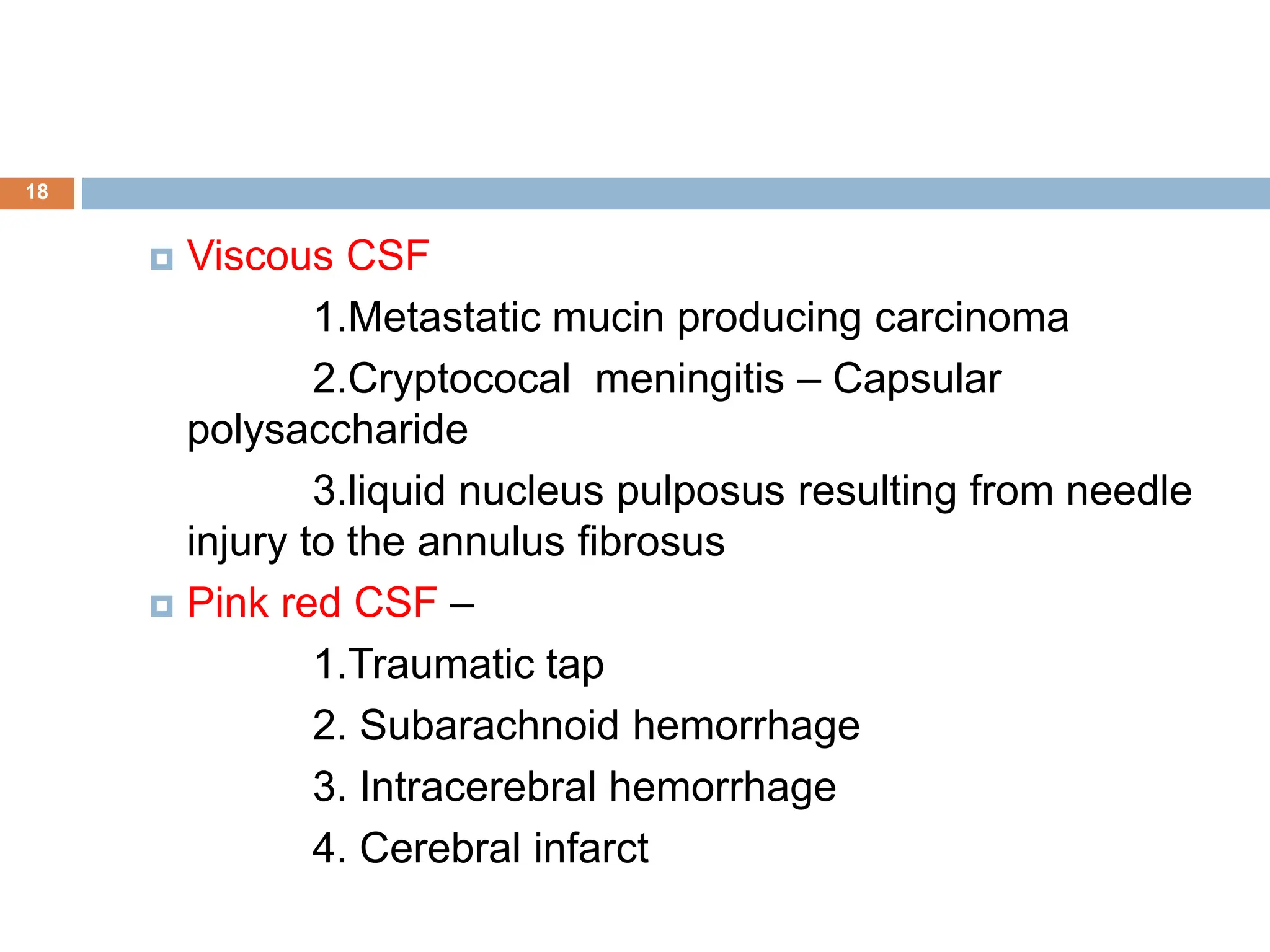
![Calculation:
23
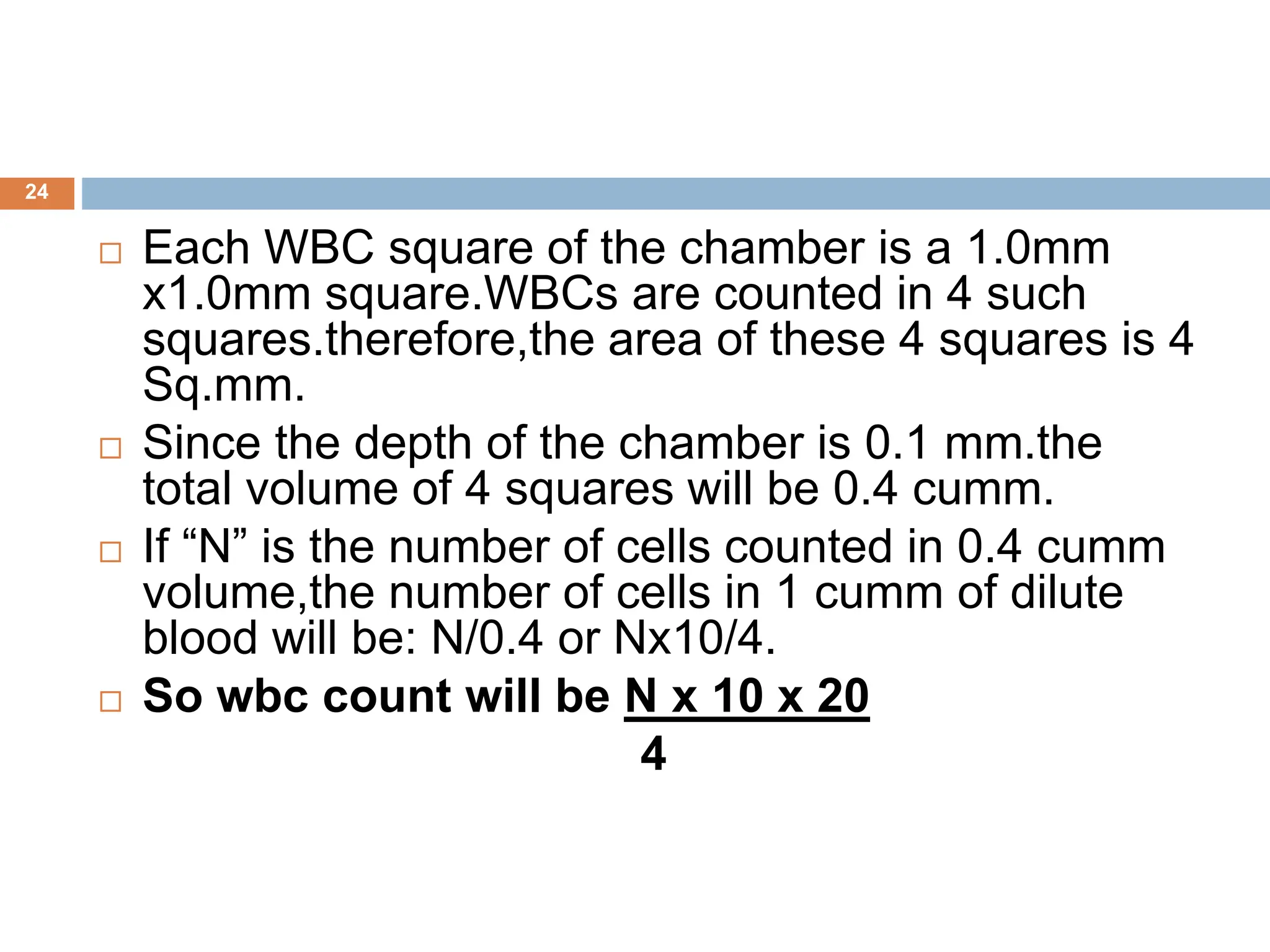
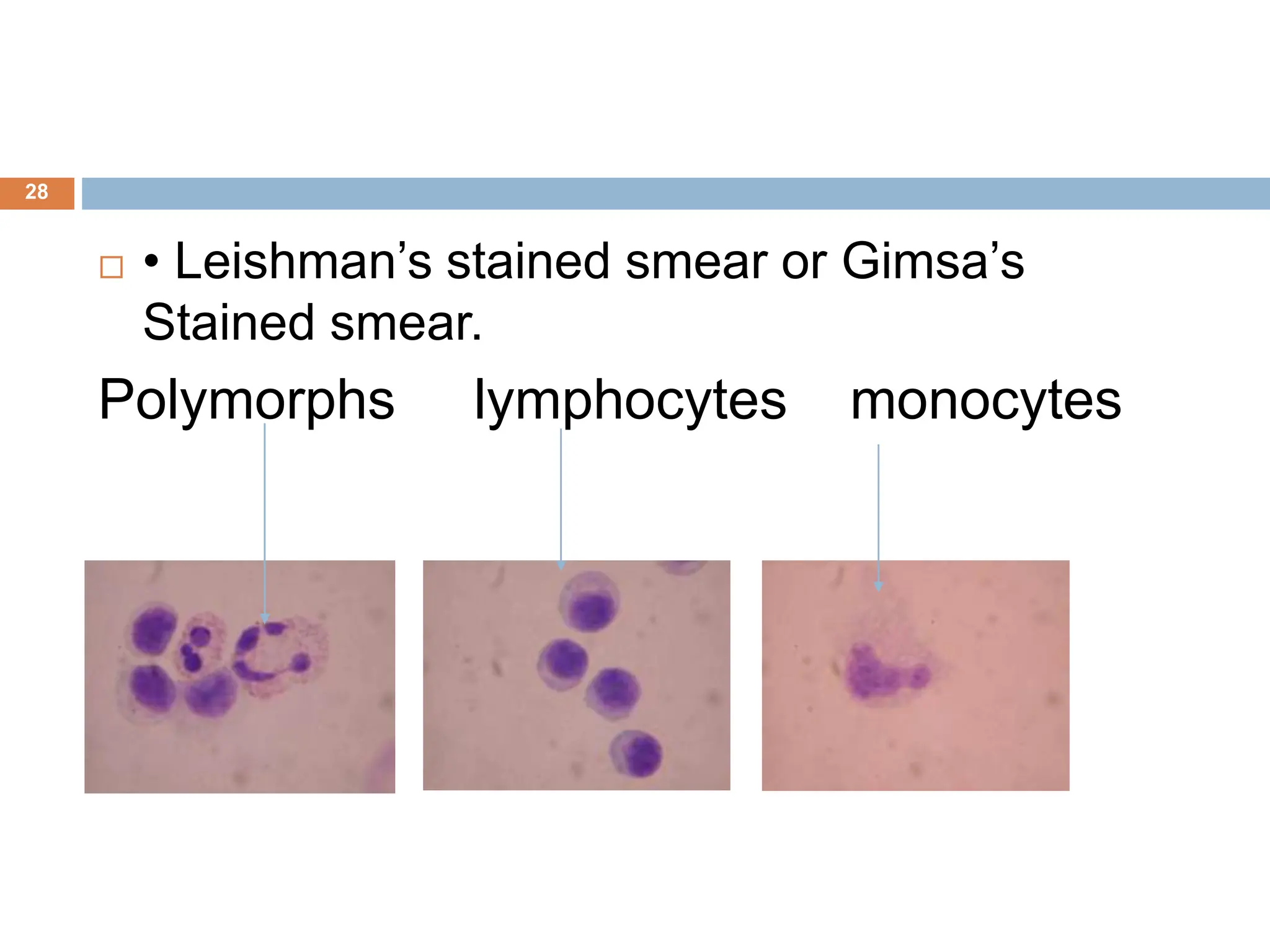
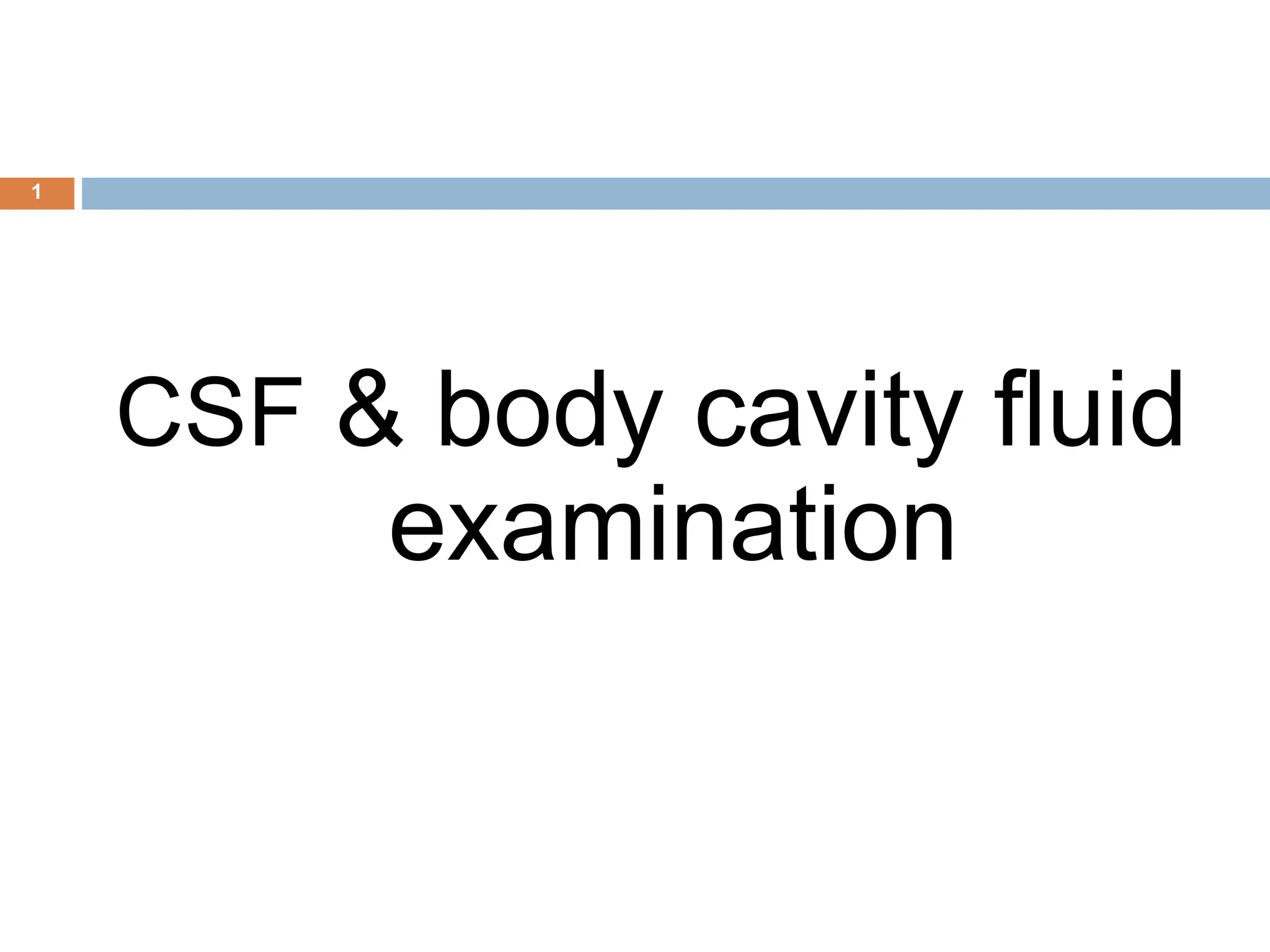
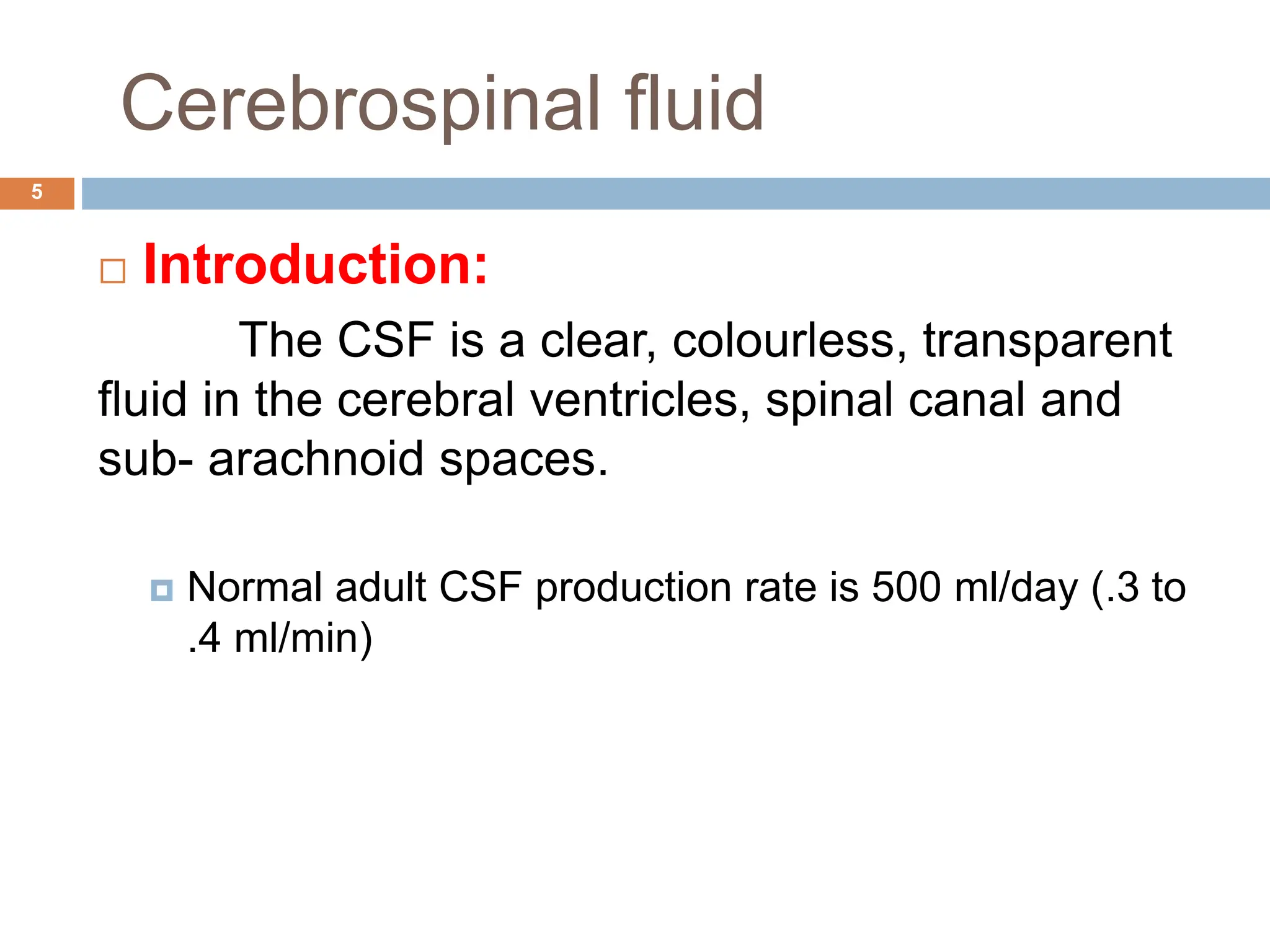
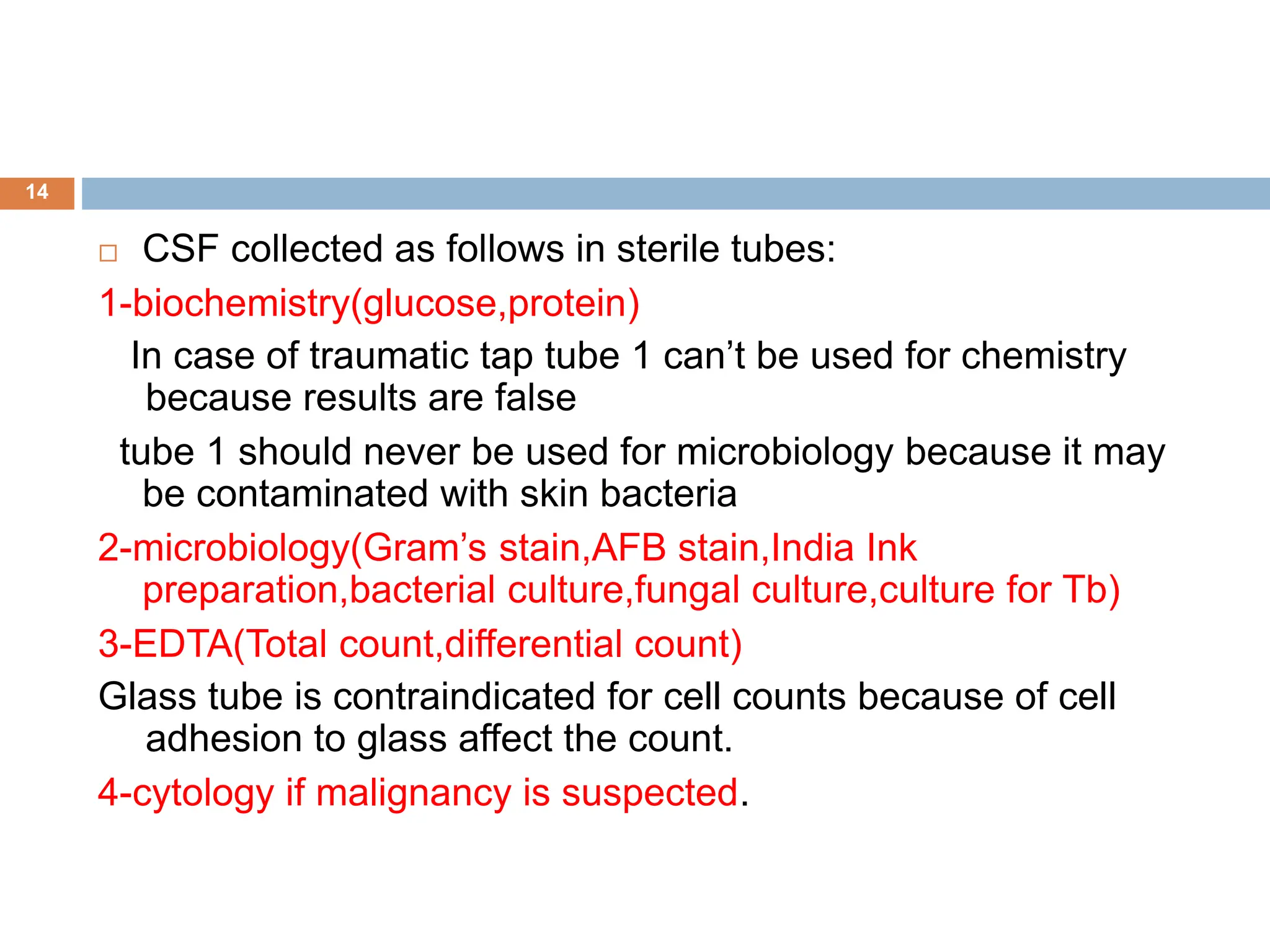
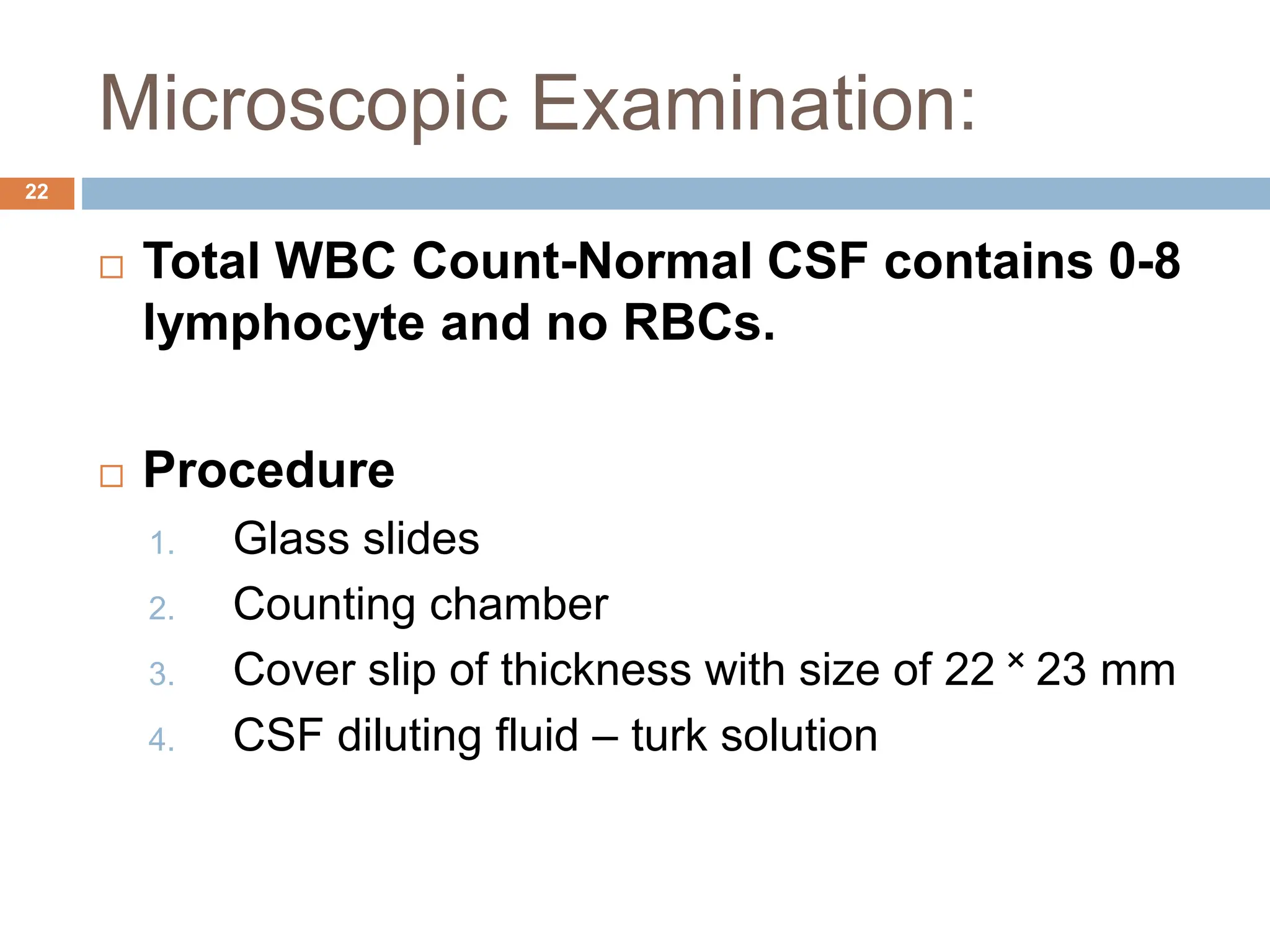
If CSF is cloudy then make a dilution of 1:10 or 1:20 [is
made using 0.05 ml of CSF and 0.95 ml of turk solution]
Charge the counting chamber properly without any air
bubbles.
• Wait for 5 minutes before counting, to allow the cells in CSF
to settle down.
• Count the cells in all 4 squares by using low power
objective.
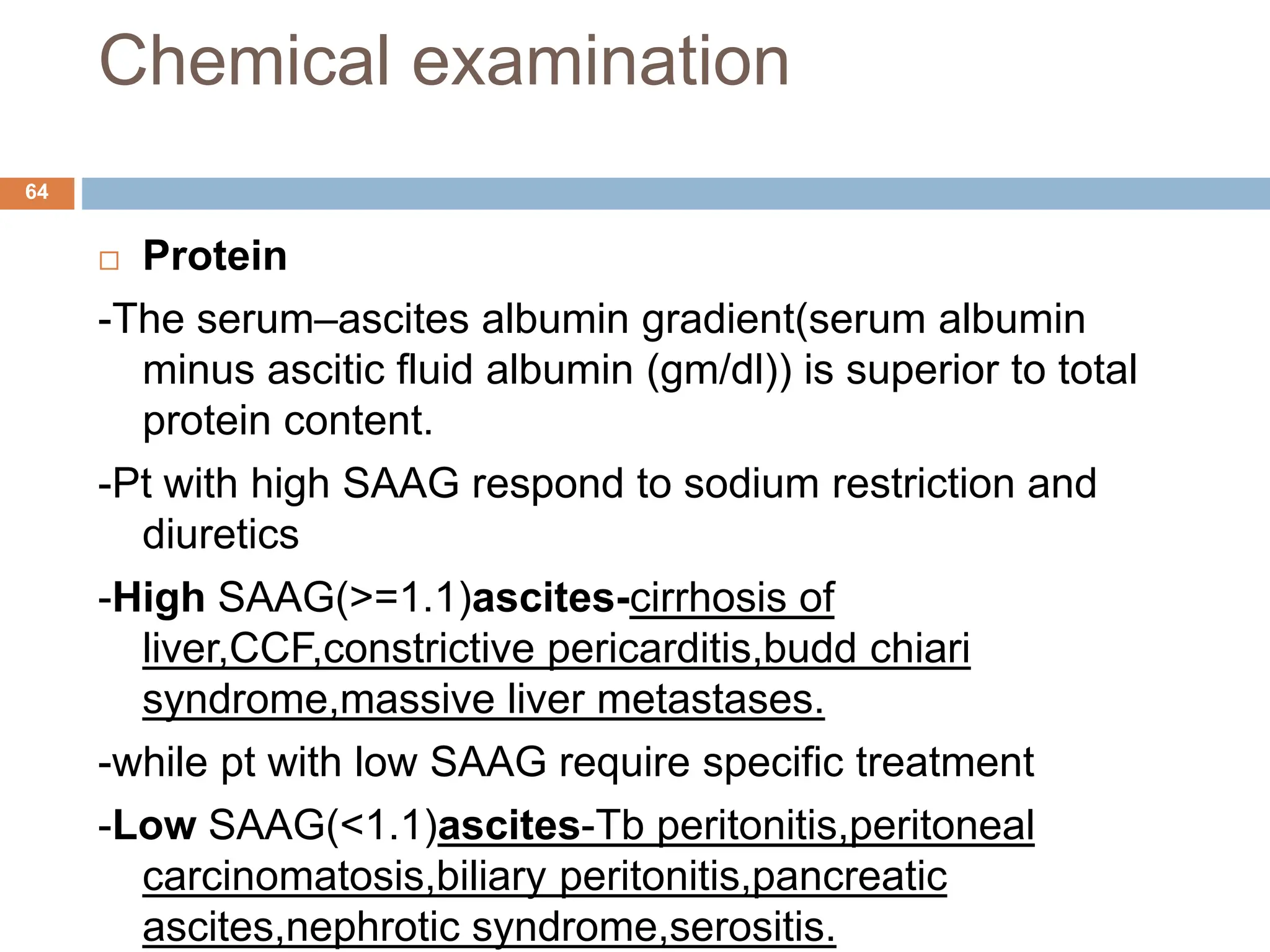
Calculation
WBC in CSF/cumm (μL)=
No.of cell x dilution factor
total volume
=counted cells x10 x20
4](https://image.slidesharecdn.com/csfbodycavityfluidexamination-240628040833-00c11af1/75/CSF-Body-Cavity-Fluid-Examination-ppt-23-2048.jpg)