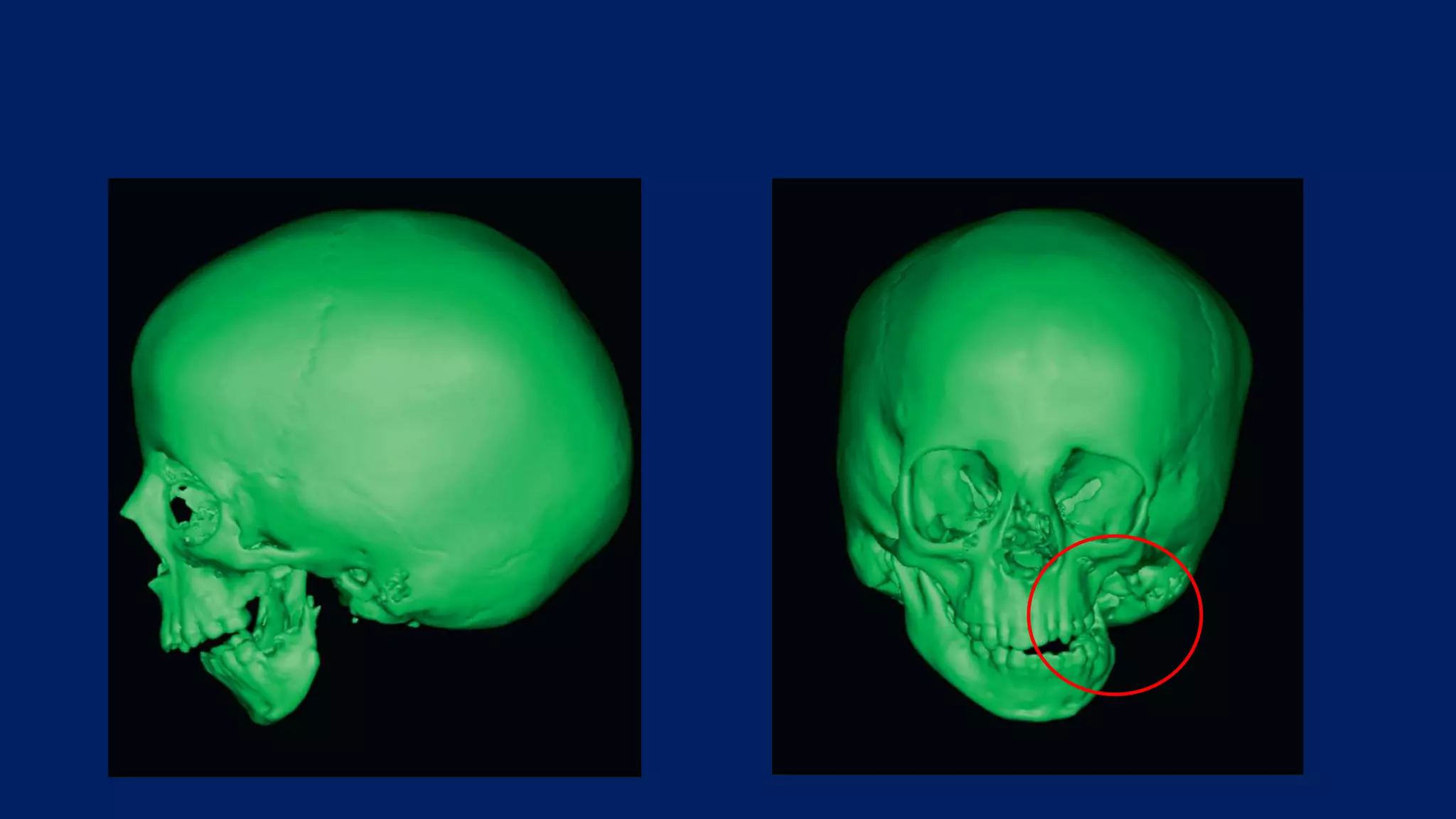
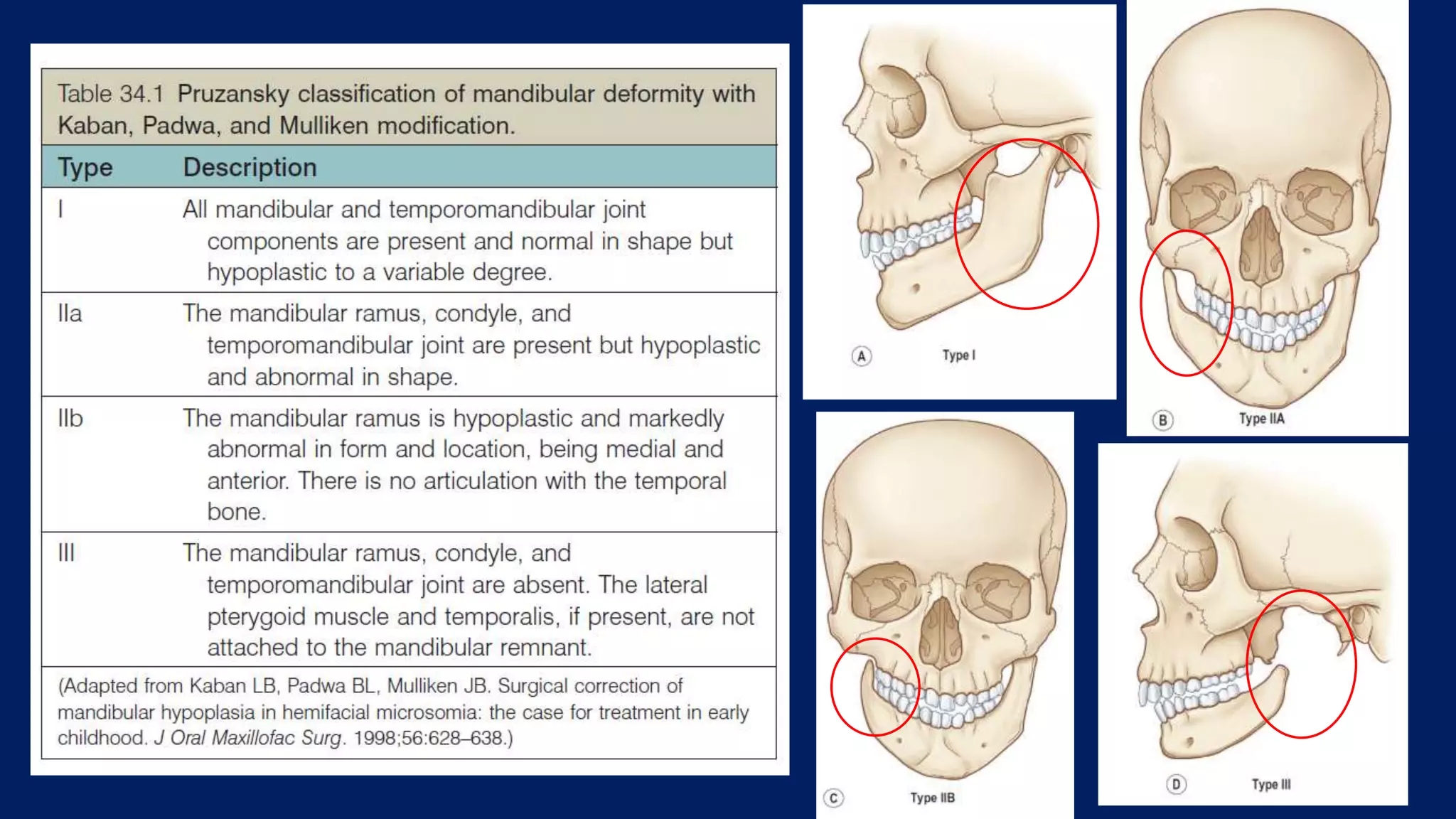
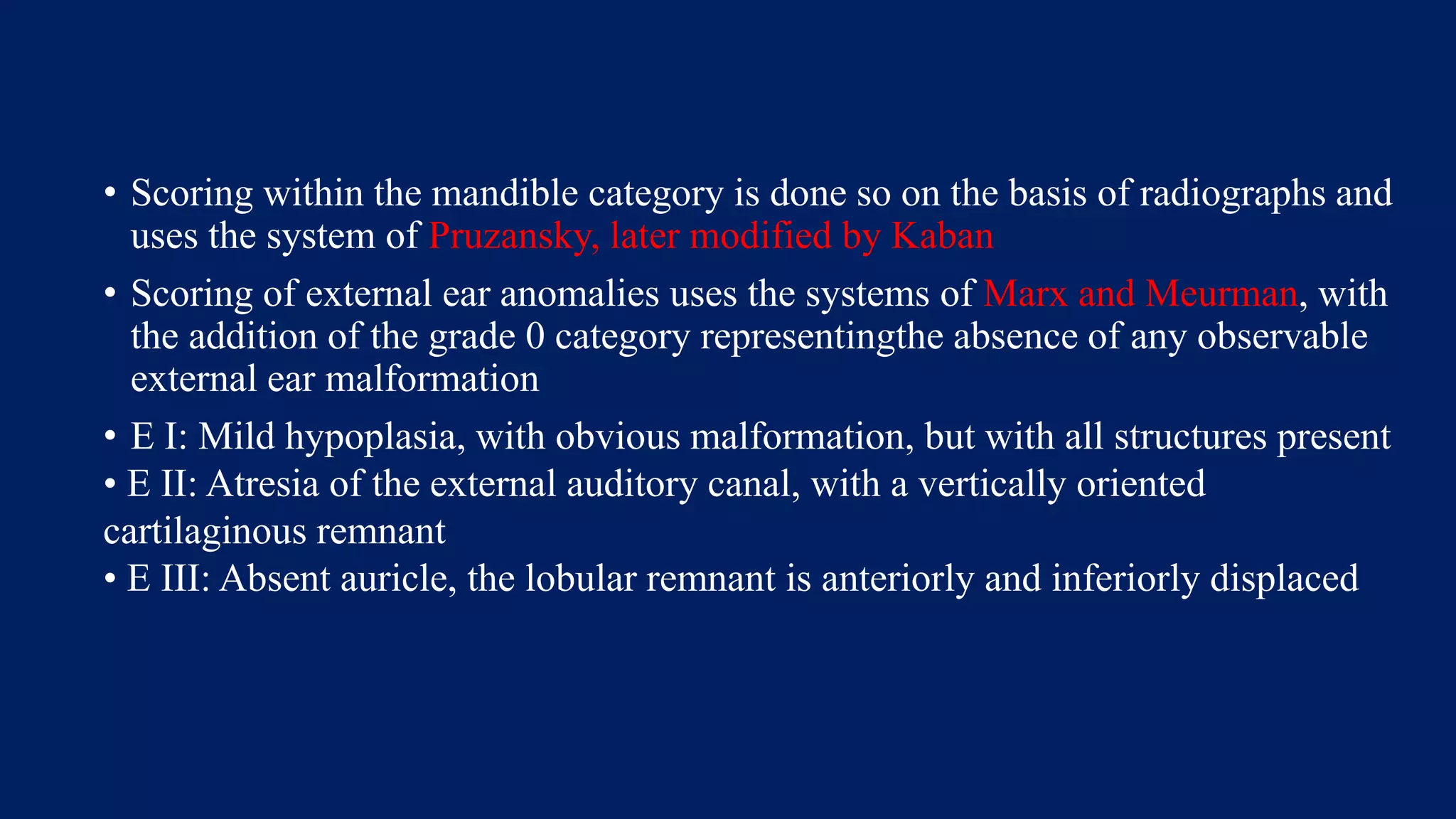
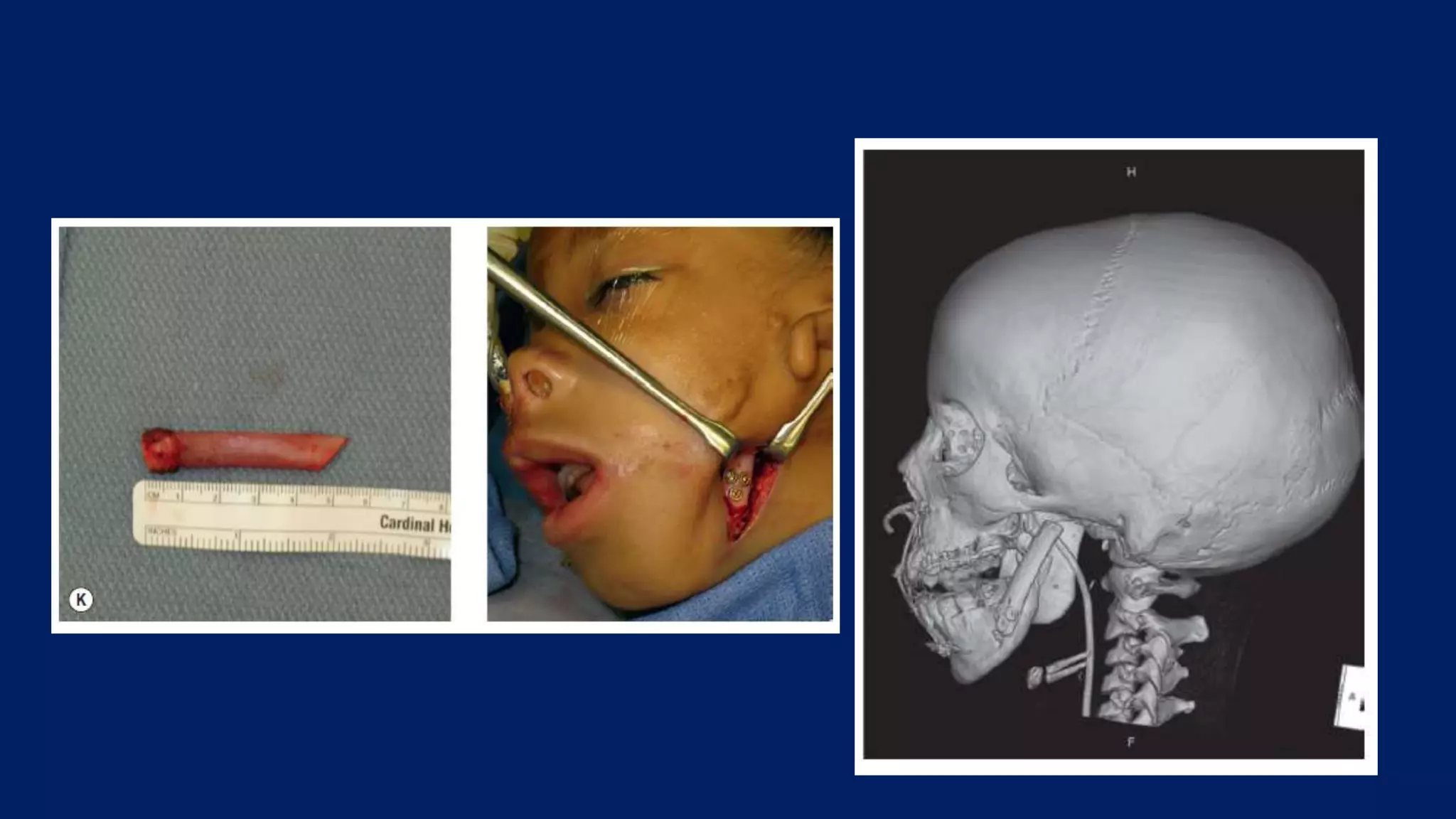
Craniofacial microsomia involves congenital malformations of structures arising from the first and second branchial arches. It can cause deformities of the orbit, mandible, ear, nerves and soft tissues that range from mild to severe. The etiology is unclear but may involve vascular perturbations, teratogen exposure or neural crest pathology. Treatment involves surgery to correct deformities such as mandibular distraction, commissuroplasty or facial reanimation procedures.