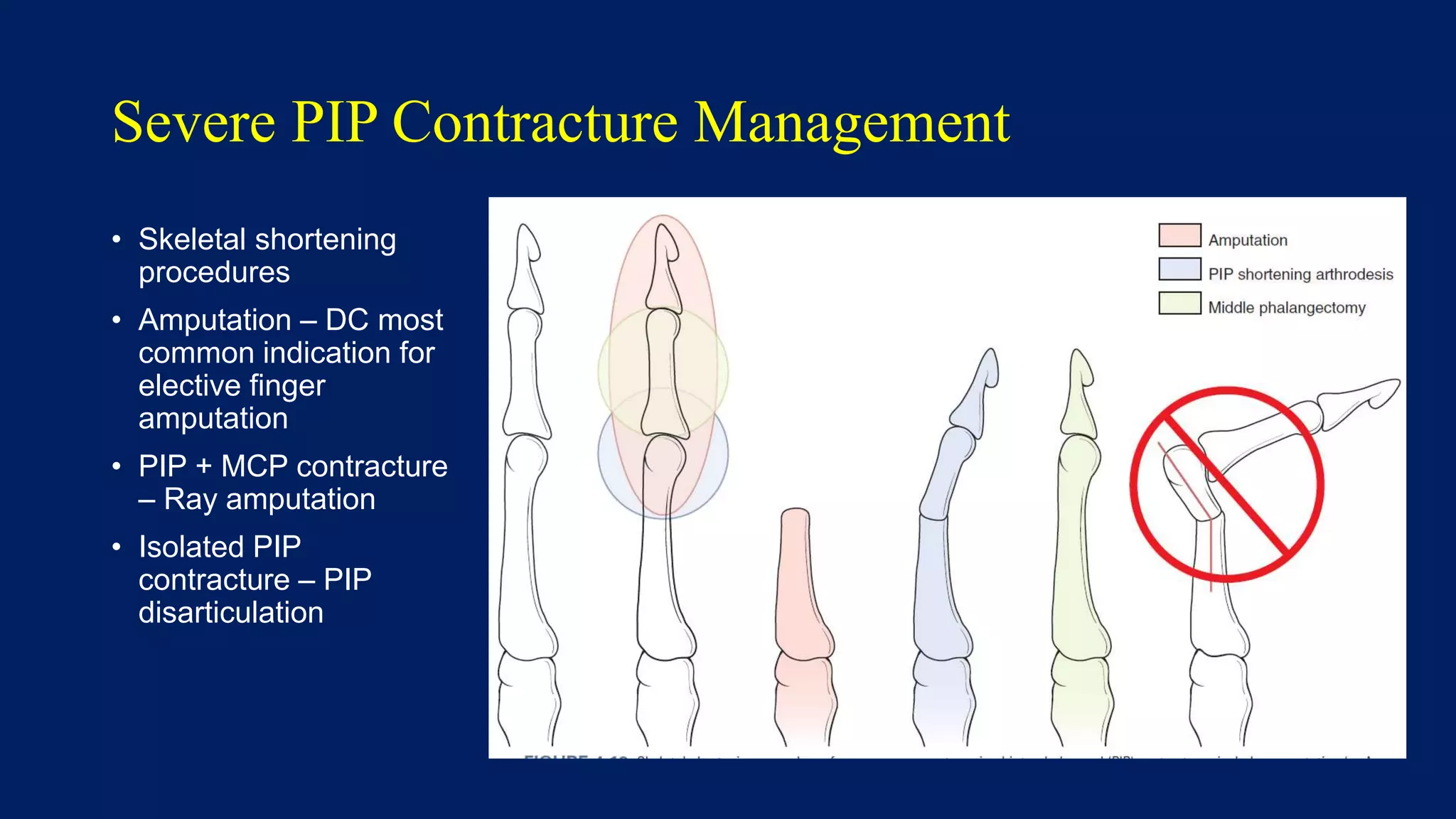
Dupuytren's contracture is a progressive fibroproliferative disease affecting the palmar fascia that can cause fingers to bend into the palm. It typically affects middle-aged Caucasian men and has genetic and environmental risk factors. Physical exam reveals nodules and cords in the palm which can cause finger contractures over time. Treatment options range from minimally invasive needle fasciotomy or collagenase injections to more extensive fasciectomy surgery to remove diseased fascia. Recurrence is common, especially in patients with more severe disease.