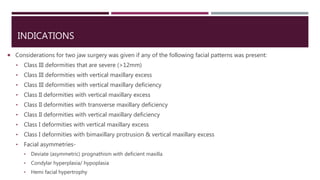
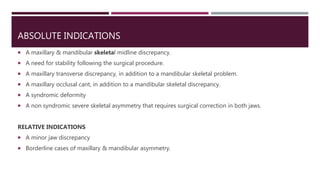
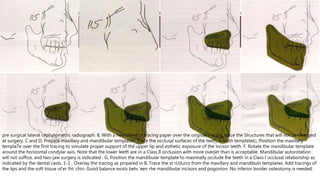
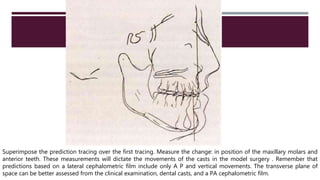
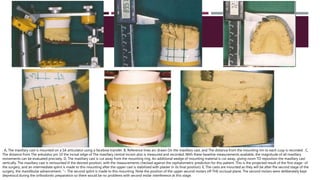
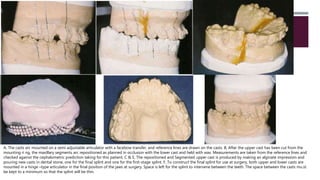
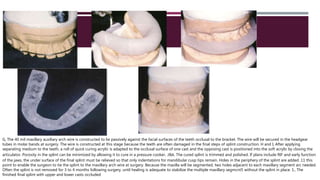
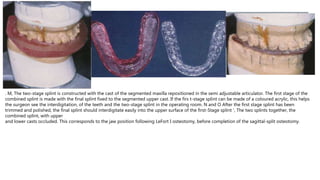
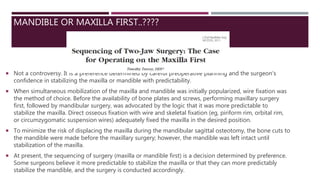
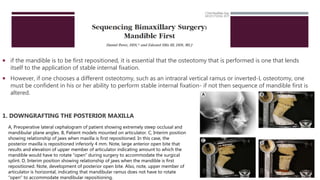
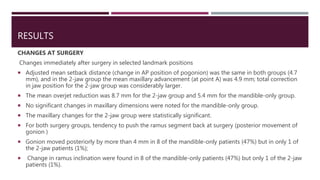
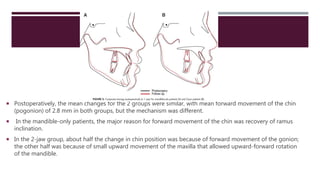
This document discusses bi-maxillary surgery, which involves surgical correction of skeletal deformities in both the upper and lower jaw. It covers indications for bi-maxillary surgery such as severe class III deformities or facial asymmetries. Careful pre-operative planning is required, including cephalometric prediction tracings and model surgery to plan the movements. The sequence of surgery typically involves a Lefort I osteotomy of the maxilla followed by bilateral sagittal split osteotomies of the mandible while holding the repositioned maxilla in place. Splints are used to guide jaw positioning during the procedure.