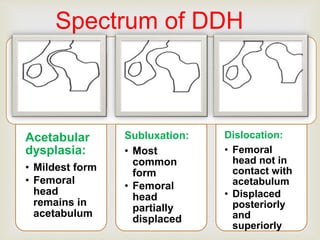
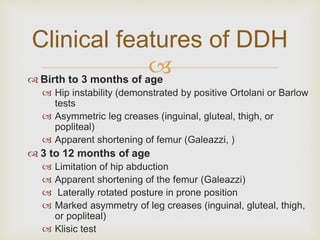
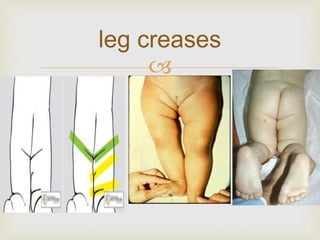
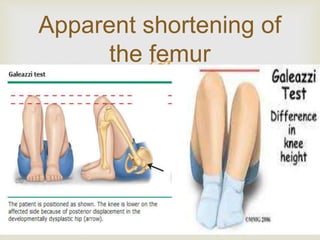
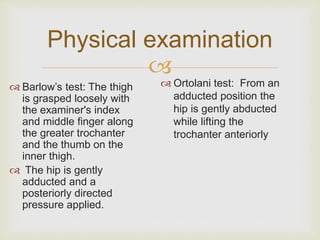
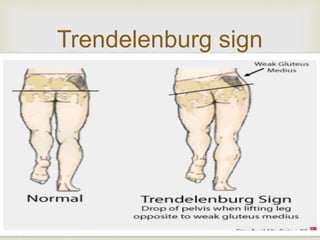
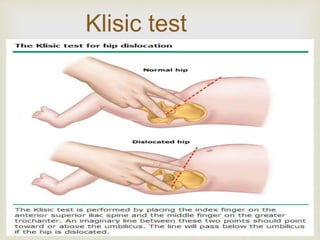
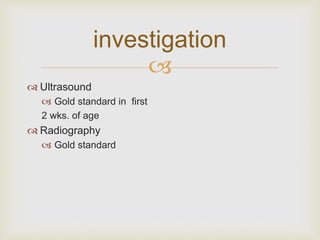
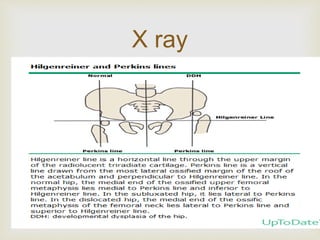
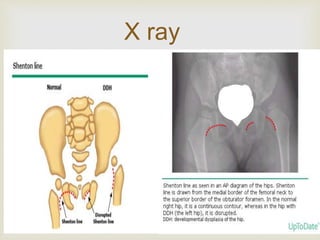
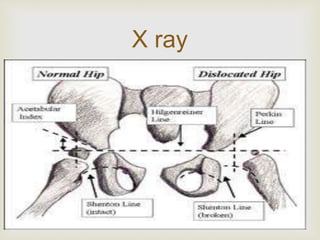
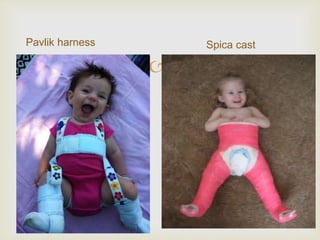
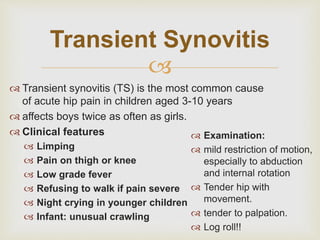
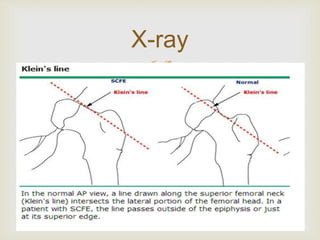
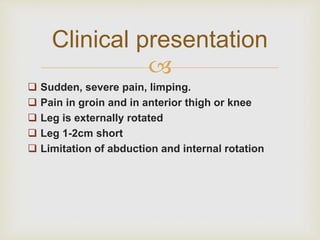
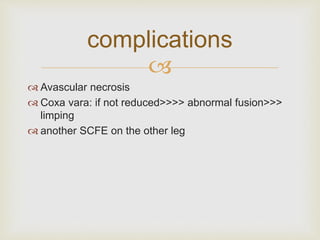
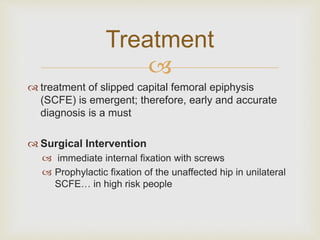
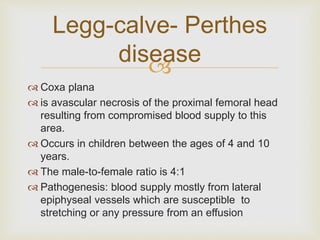
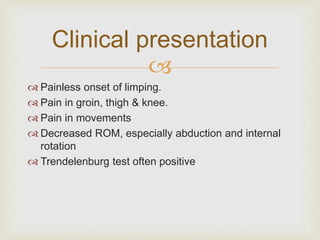
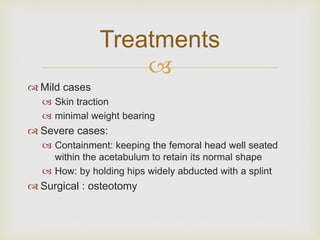
This document discusses several common pediatric hip conditions: developmental dysplasia of the hip (DDH), transient synovitis, slipped capital femoral epiphysis (SCFE), and Legg-Calvé-Perthes disease. It provides details on the epidemiology, clinical presentation, investigations, and management for each condition. DDH is a hip joint abnormality more common in girls, while transient synovitis causes acute hip pain in children aged 3-10 years. SCFE occurs during puberty and is associated with obesity and endocrine disorders. Legg-Calvé-Perthes disease results from impaired blood supply to the femoral head between ages 4-10 years. Management depends on the specific condition but