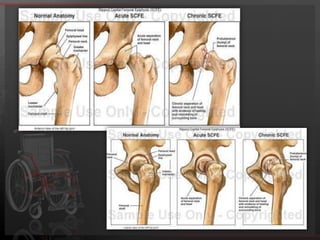
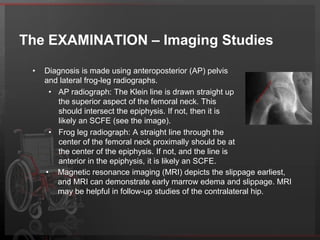
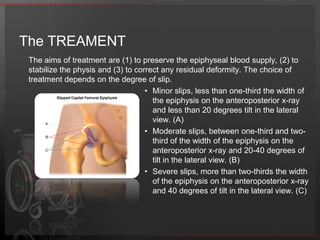
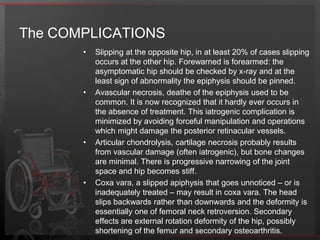
Slipped capital femoral epiphysis (SCFE) is a common hip disorder in adolescents where the femoral head slips out of position in the femoral neck. It is caused by weakness in the growth plate and can be influenced by both mechanical and biochemical factors like obesity. Patients present with hip, thigh, or knee pain and decreased range of motion. Diagnosis is made through x-rays showing displacement of the femoral head. Treatment depends on the degree of slippage and aims to stabilize the growth plate to prevent further slipping and complications like avascular necrosis.