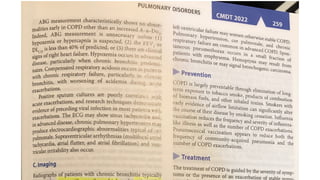
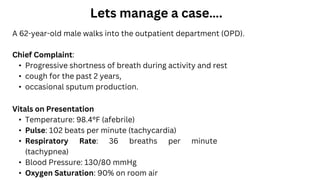
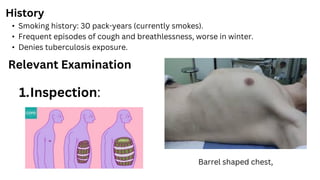
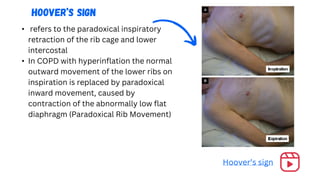
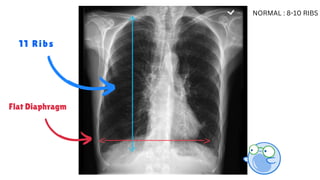
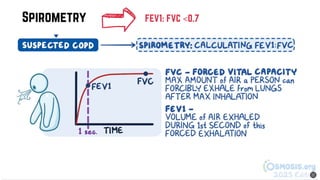
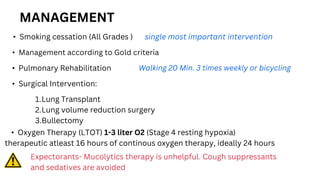
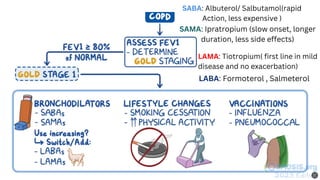
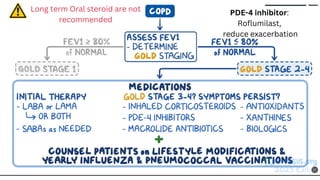
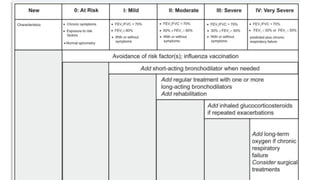
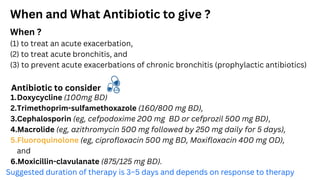
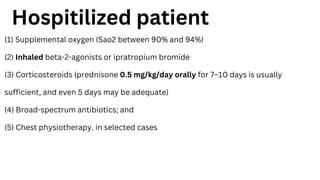
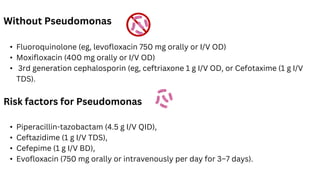
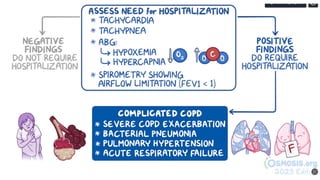
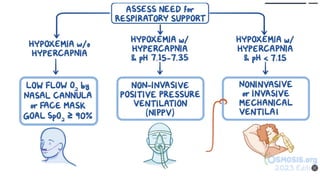
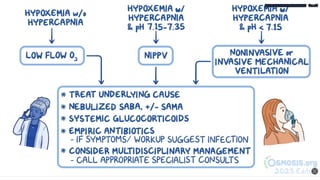
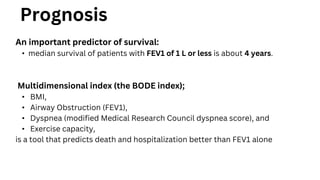
The document discusses chronic obstructive pulmonary disease (COPD), including its diagnosis, management, and emergency treatment measures. It covers key clinical features, diagnostic tests, and various treatment options such as smoking cessation, medication types, and surgical interventions. The document also highlights the importance of assessing exacerbations and outlines the prognosis for patients with different stages of COPD.