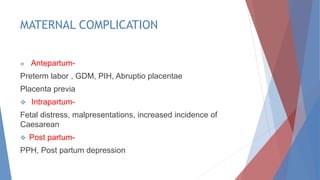
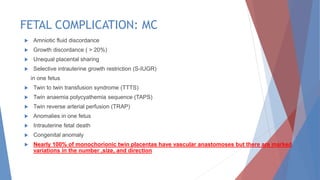
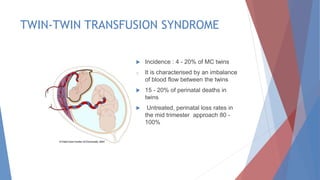
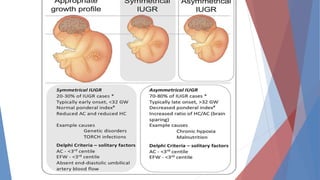
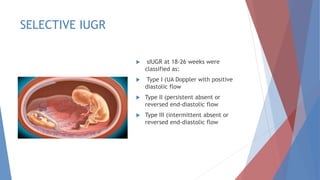
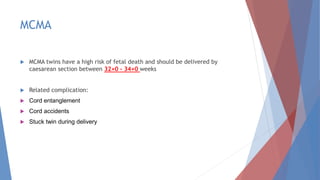
This document discusses complications and management of monochorionic twin pregnancies. It notes that monochorionic twins have higher risks of fetal loss and neurological issues than dichorionic twins. Complications can include twin-twin transfusion syndrome, selective intrauterine growth restriction, single fetal demise, and congenital anomalies. Management may involve planned delivery between 34-36 weeks depending on the complication. For uncomplicated monochorionic twins, an aim is vaginal delivery from 36 weeks with monitoring, though risks remain. Caesarean delivery is recommended for complications like monoamniotic twins or conjoined twins. Close monitoring in a fetal medicine center is important due to the risks.