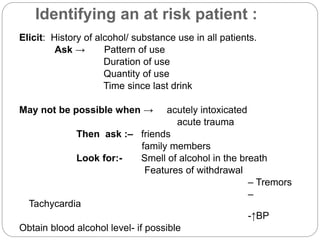
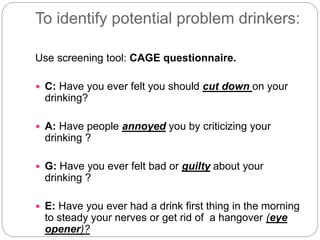
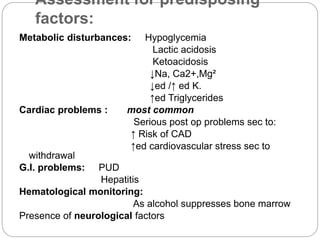
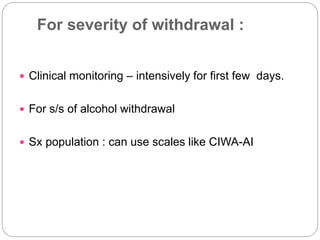
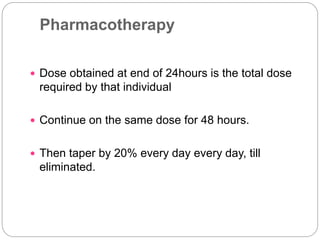
Dr. Sumit Chandak discusses the management of alcohol withdrawal, including identifying at-risk patients, assessing severity, and treating complications. Key points include using the CAGE questionnaire to screen for problem drinking, monitoring for withdrawal symptoms using the CIWA-Ar scale, and managing complications like delirium pharmacologically with benzodiazepines while also employing environmental interventions and frequent reorientation. The goal is to promote abstinence and safely manage withdrawal to prevent associated increased morbidity.




![Delirium
Diagnostic criteria:
A] Disturbance of consciousness (i.e. reduced clarity
of awareness of the environment) with reduced
ability to focus, sustain, or shift attention.
B] A change in cognition (such as memory deficit ,
disorientation, language disturbance) or the
development of a perceptual disturbance that is not
better accounted for by a preexisting, established,
or evolving dementia
.](https://image.slidesharecdn.com/alcoholwithdrawalmm-150606061031-lva1-app6891/85/Alcohol-withdrawal-mm-13-320.jpg)
![Delirium:
Diagnostic criteria:
C] The disturbance develops over a short period of time
(usually hours to days) and tends to fluctuate during
the course of the day.
D] There is evidence from the history, physical
examination, or laboratory findings of either (1) or (2):
1] The symptoms in Criteria A and B developed during
substance intoxication.
2] Medication use is etiologically related to the
disturbance.](https://image.slidesharecdn.com/alcoholwithdrawalmm-150606061031-lva1-app6891/85/Alcohol-withdrawal-mm-14-320.jpg)

![Management of alcohol withdrawal /
risk patient:
In at risk patient promote abstinence for at least 4
weeks of an elective pre-op procedure as it
decreases morbidity from 74% -31%
Modalities of Intervention:
1]Pharmacotherapy : Substitute
Adjuvant
2] Counseling](https://image.slidesharecdn.com/alcoholwithdrawalmm-150606061031-lva1-app6891/85/Alcohol-withdrawal-mm-16-320.jpg)


![Pharmacotherapy:
Adjuvant :For symptomatic control:
1] Propranolol
2]CBZ
For metabolic parameters :
Plenty of oral fluids
Injection Thiamine/MVBC before any I.V. fluids
especially containing sugar
Tb Thiamine 75/100mg bid](https://image.slidesharecdn.com/alcoholwithdrawalmm-150606061031-lva1-app6891/85/Alcohol-withdrawal-mm-21-320.jpg)