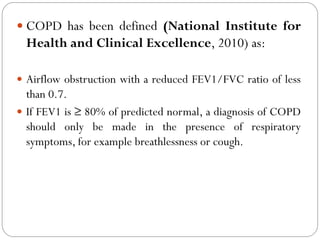
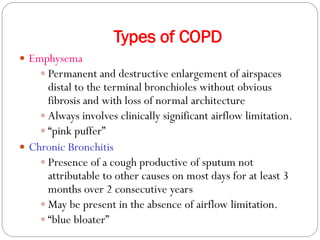
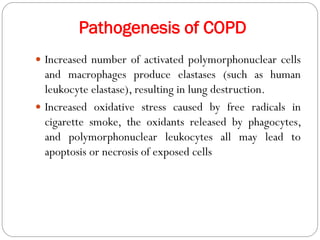
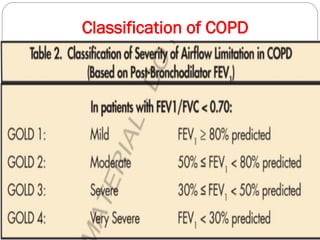
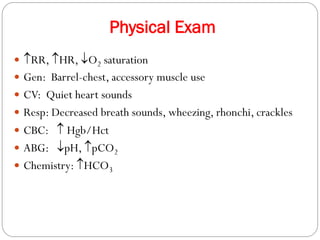
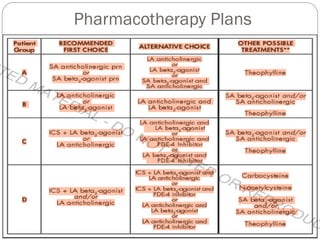
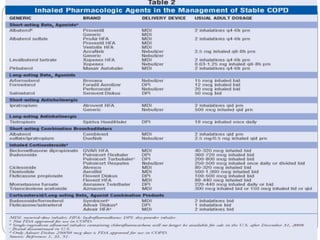
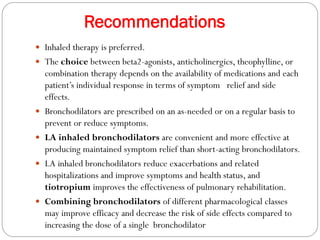
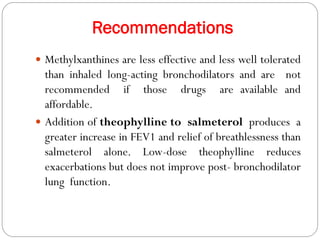
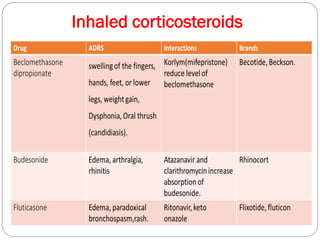
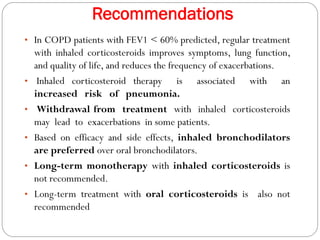
Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung disease characterized by limited airflow. It is caused most often by smoking or long-term exposure to lung irritants. Symptoms include shortness of breath, cough, wheezing, and fatigue. Diagnosis involves spirometry testing showing reduced airflow. Treatment focuses on bronchodilators, inhaled corticosteroids, pulmonary rehabilitation, oxygen therapy, and managing exacerbations. The goal is improving symptoms, lung function and quality of life.