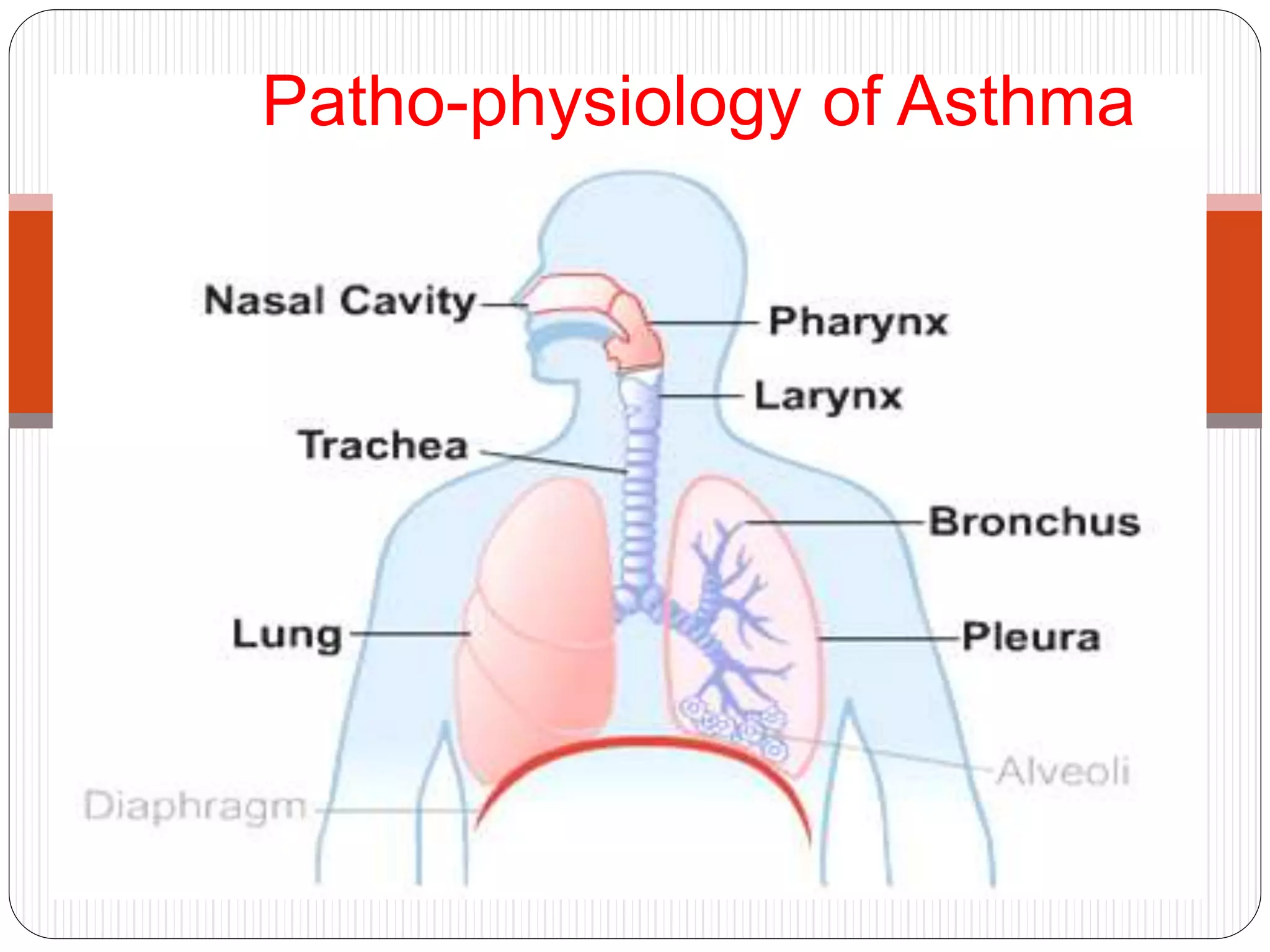
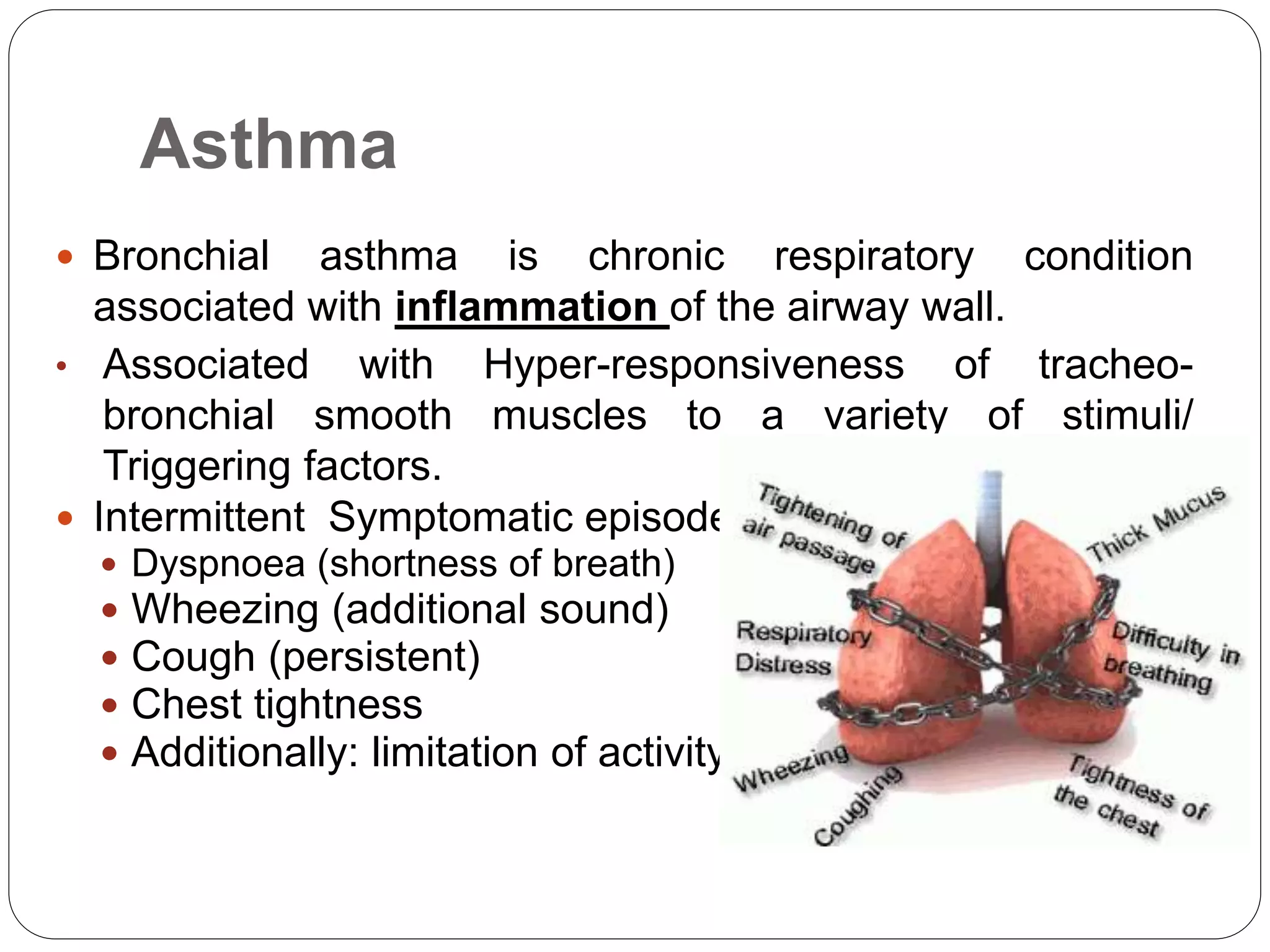
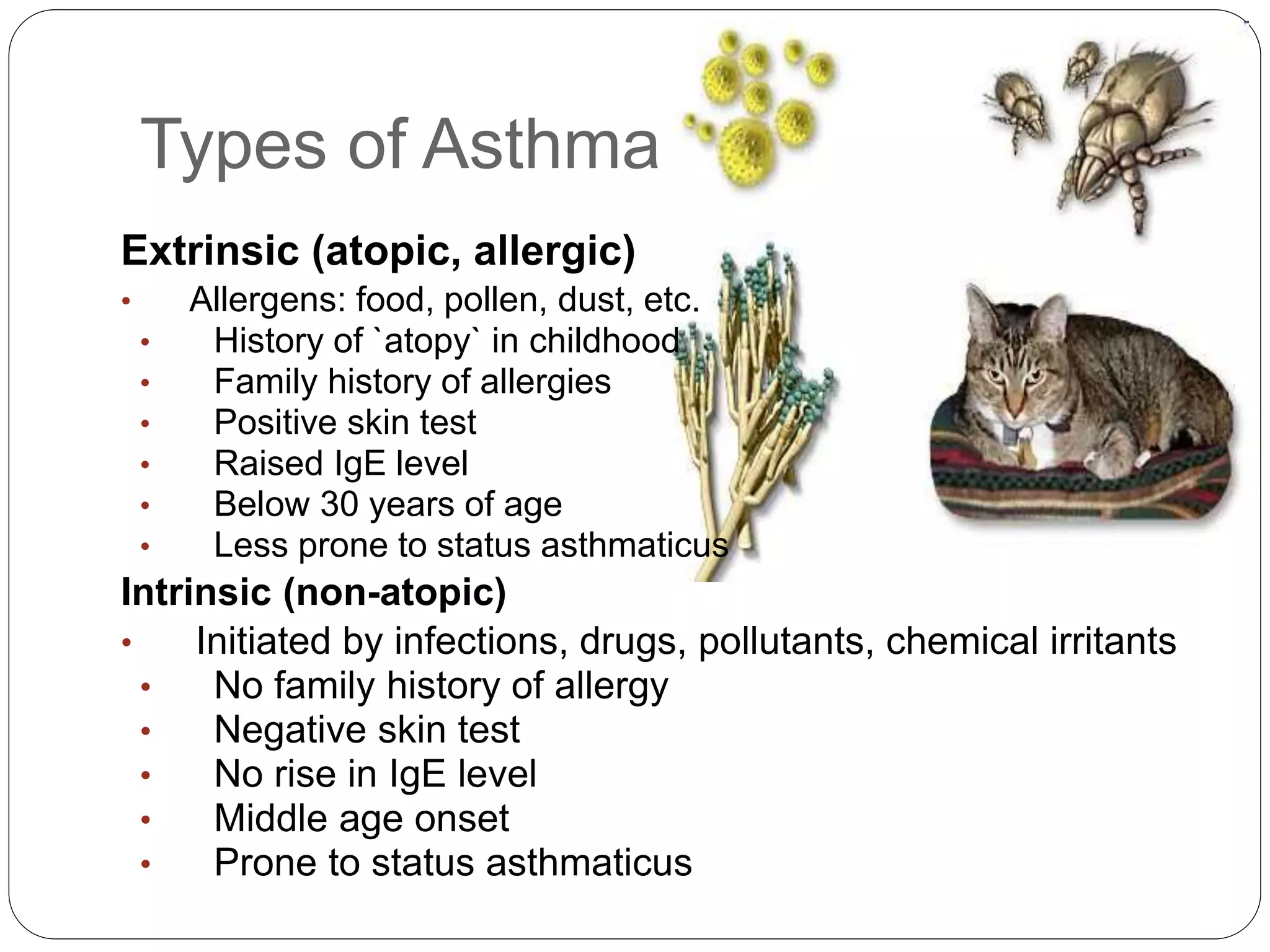
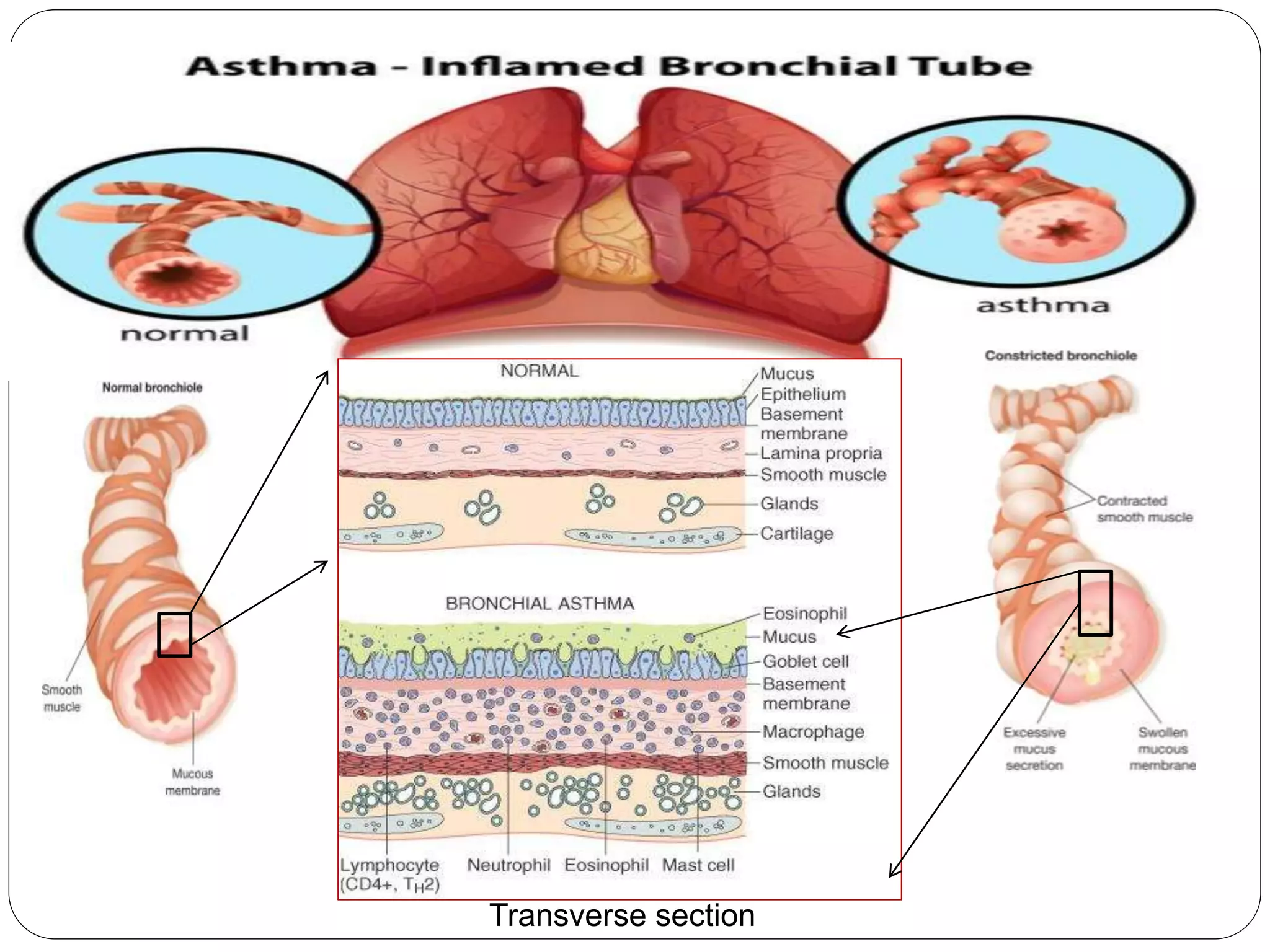
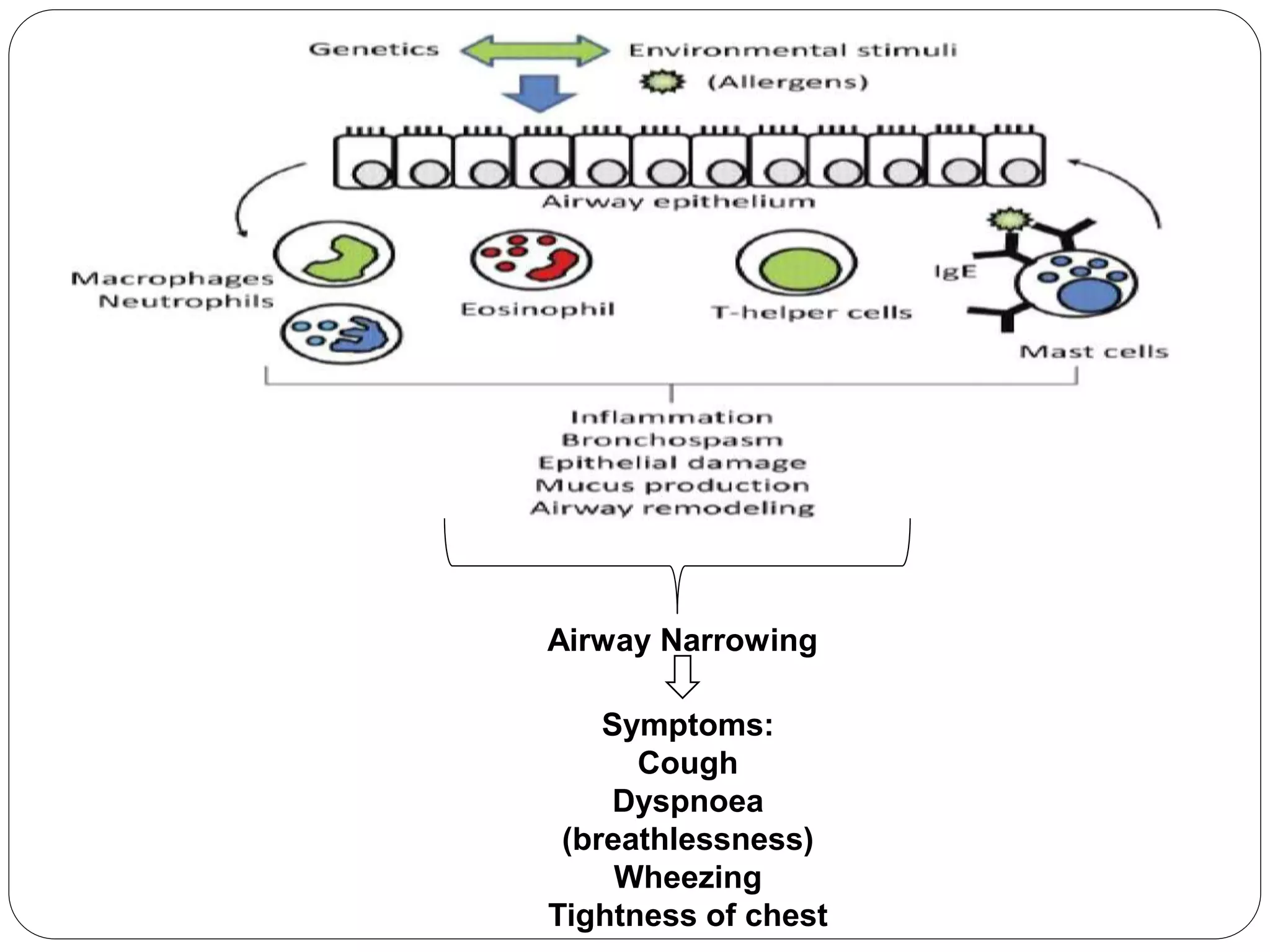
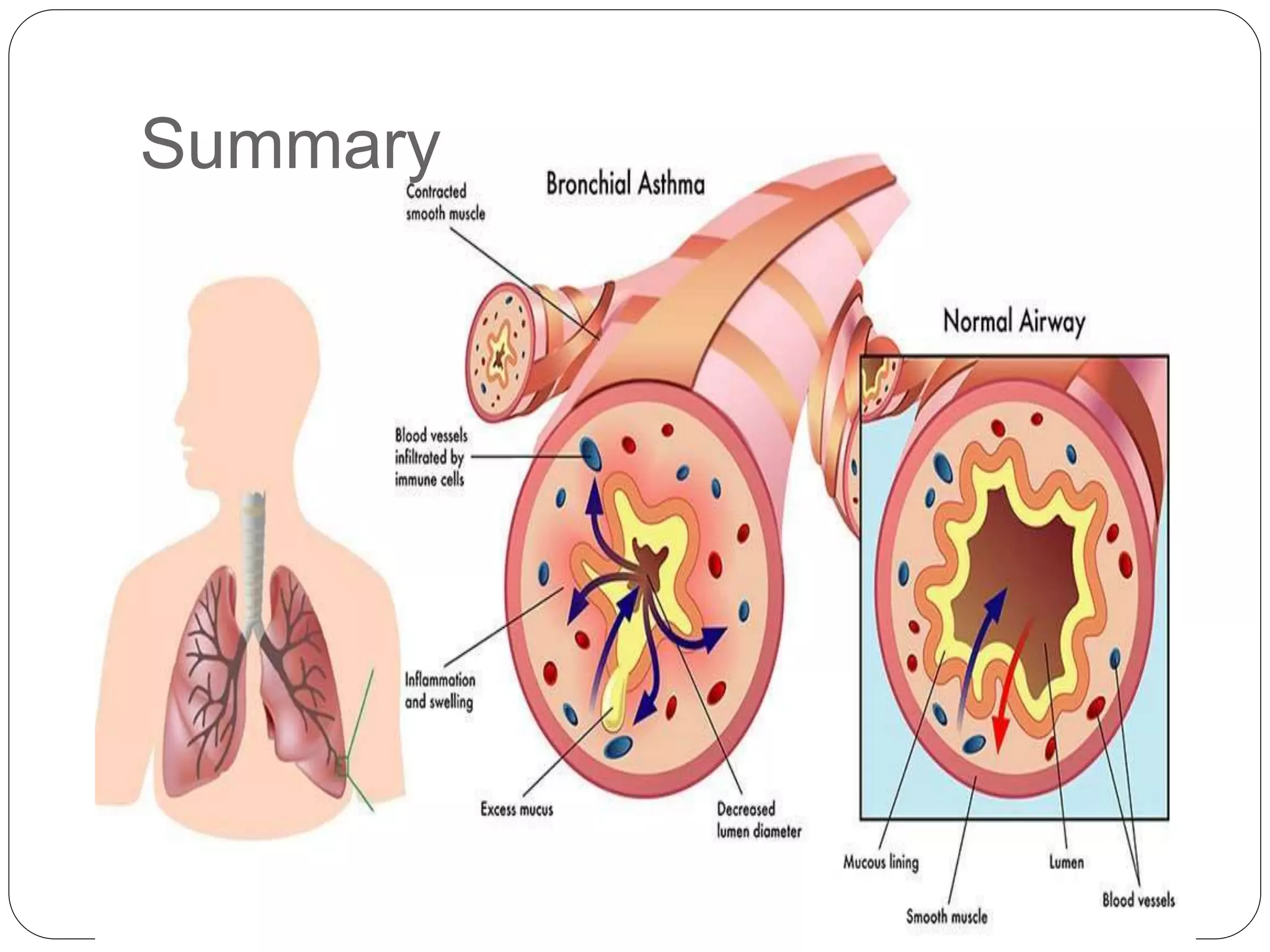
Bronchial asthma is a chronic respiratory condition characterized by inflammation of the airways and hyperresponsiveness to various triggers. Symptoms include shortness of breath, wheezing, coughing, and chest tightness. Triggers include allergens, infections, air pollution, weather changes, emotions, and certain drugs. There are two main types - extrinsic (allergic) asthma associated with family history of allergies and intrinsic asthma initiated by non-allergic factors. Pathogenesis involves airway inflammation from mast cells, eosinophils, and lymphocytes, bronchoconstriction, edema, remodeling, and obstruction leading to symptoms.