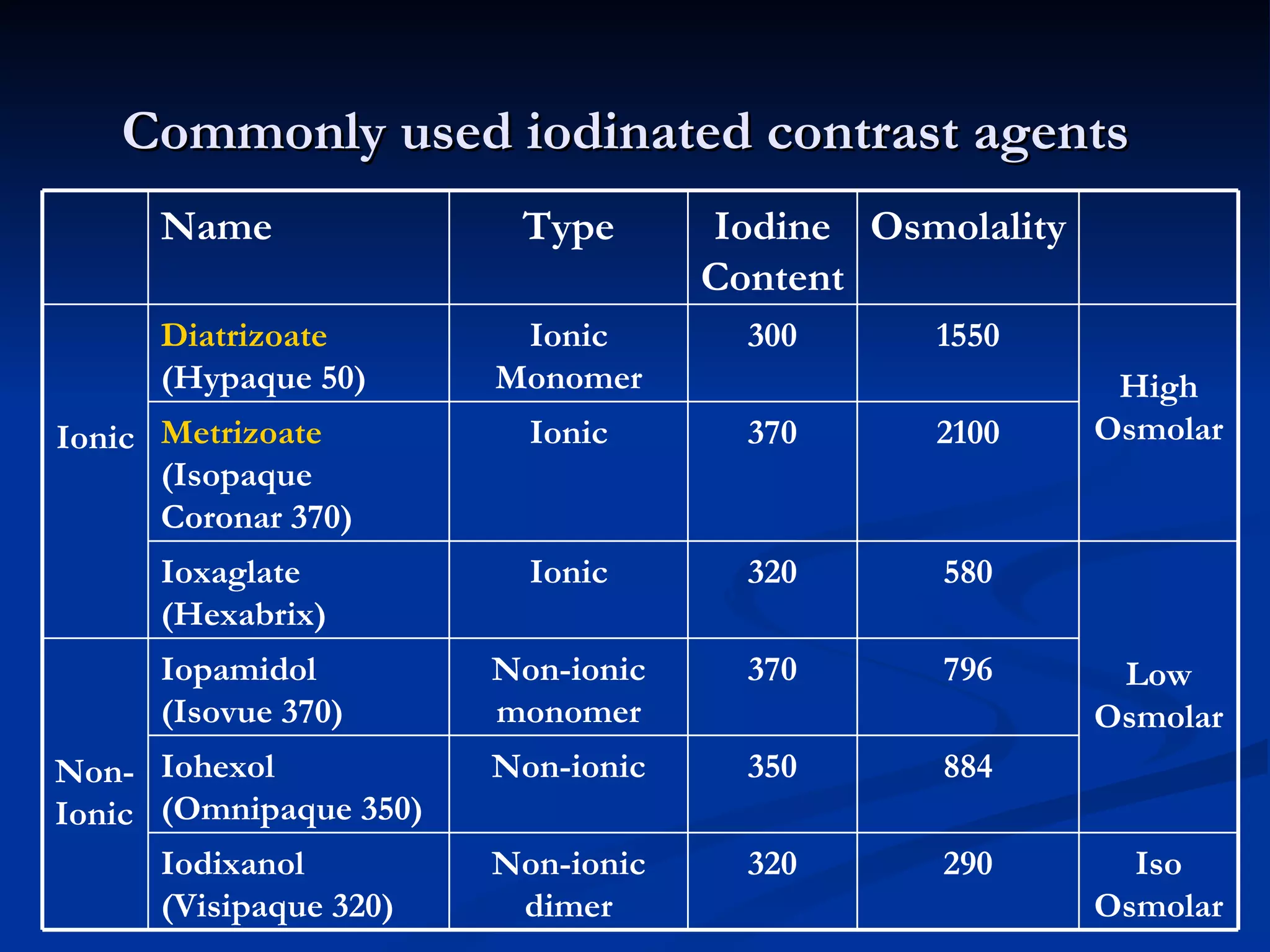
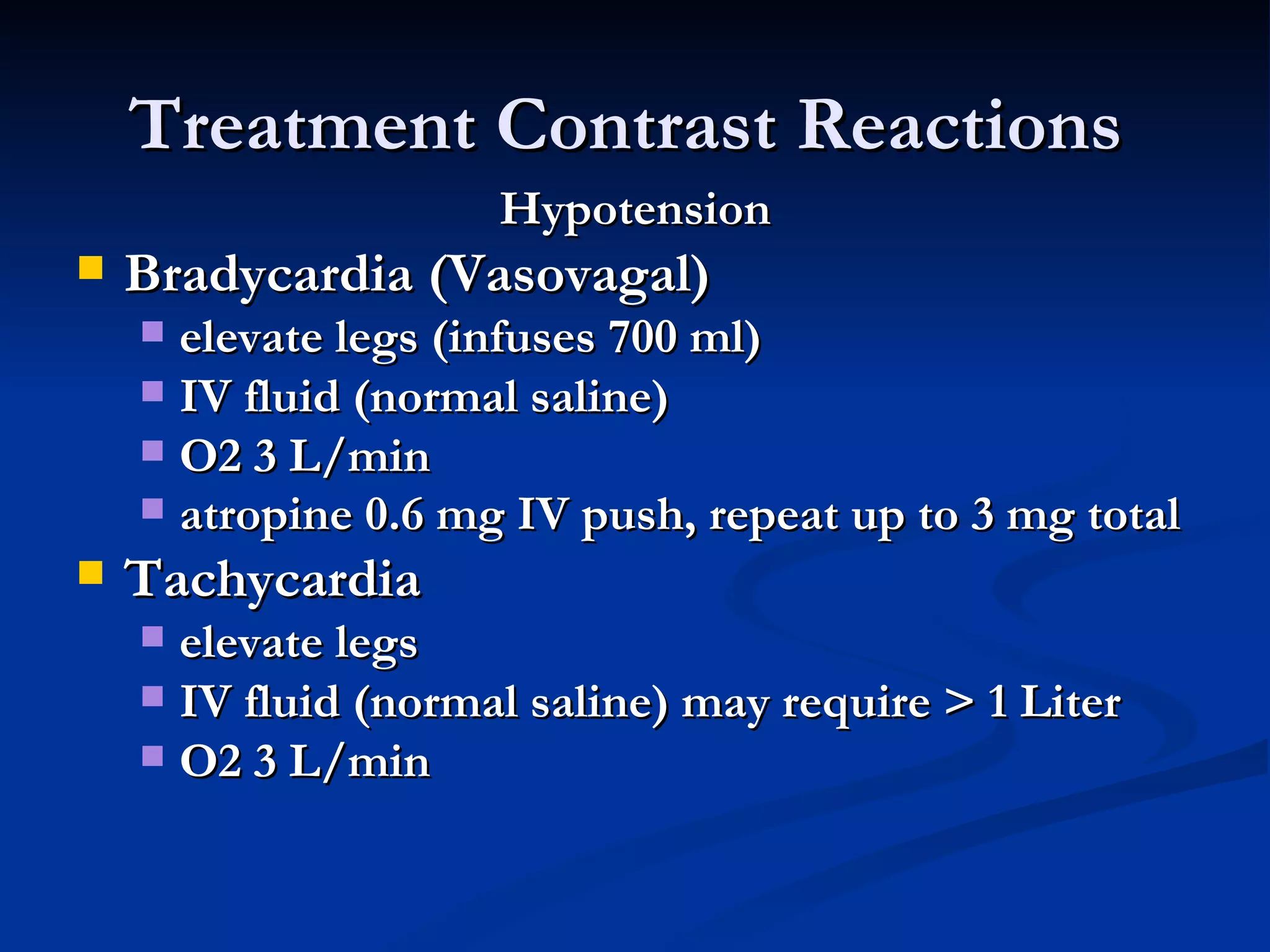
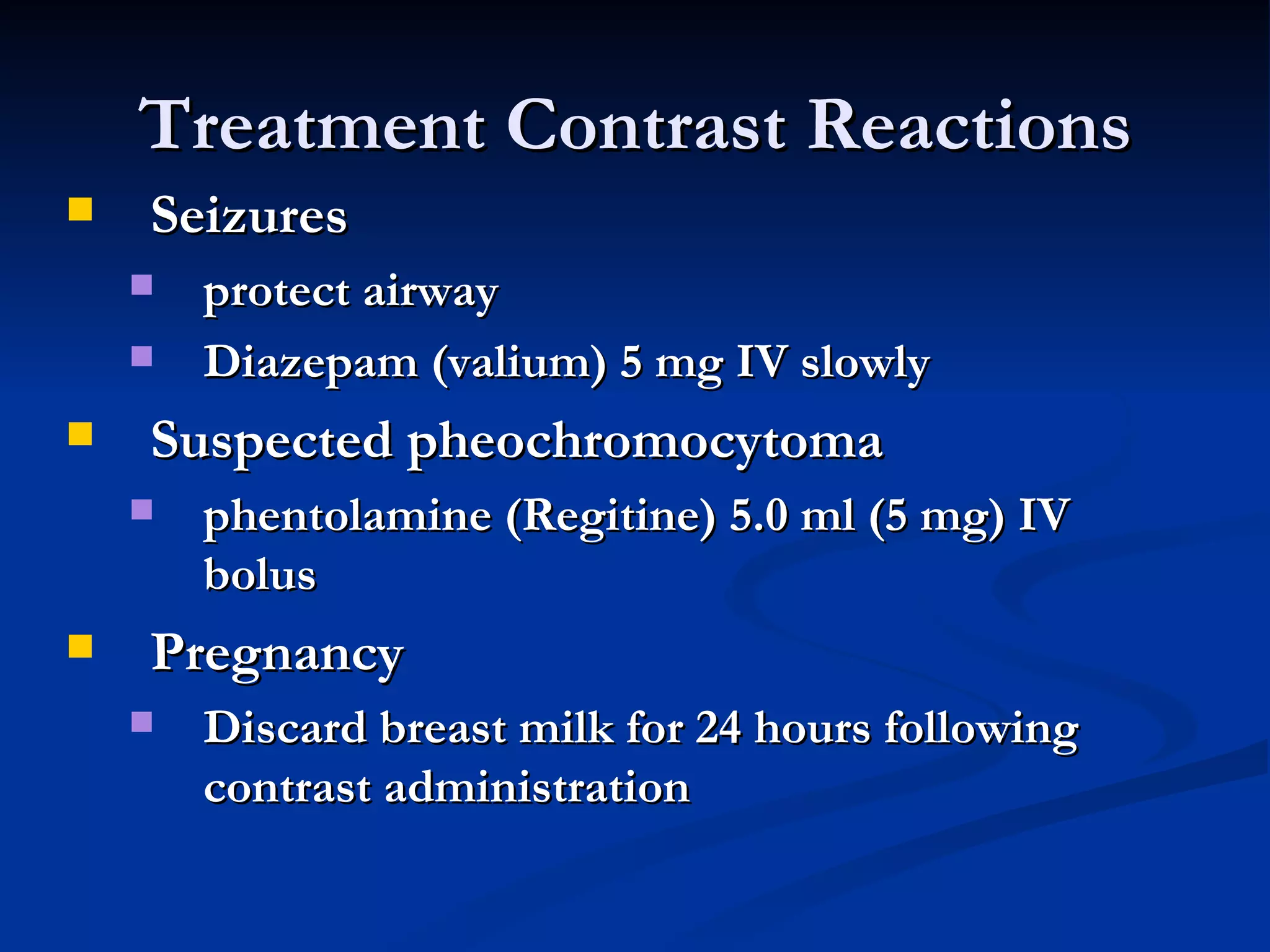
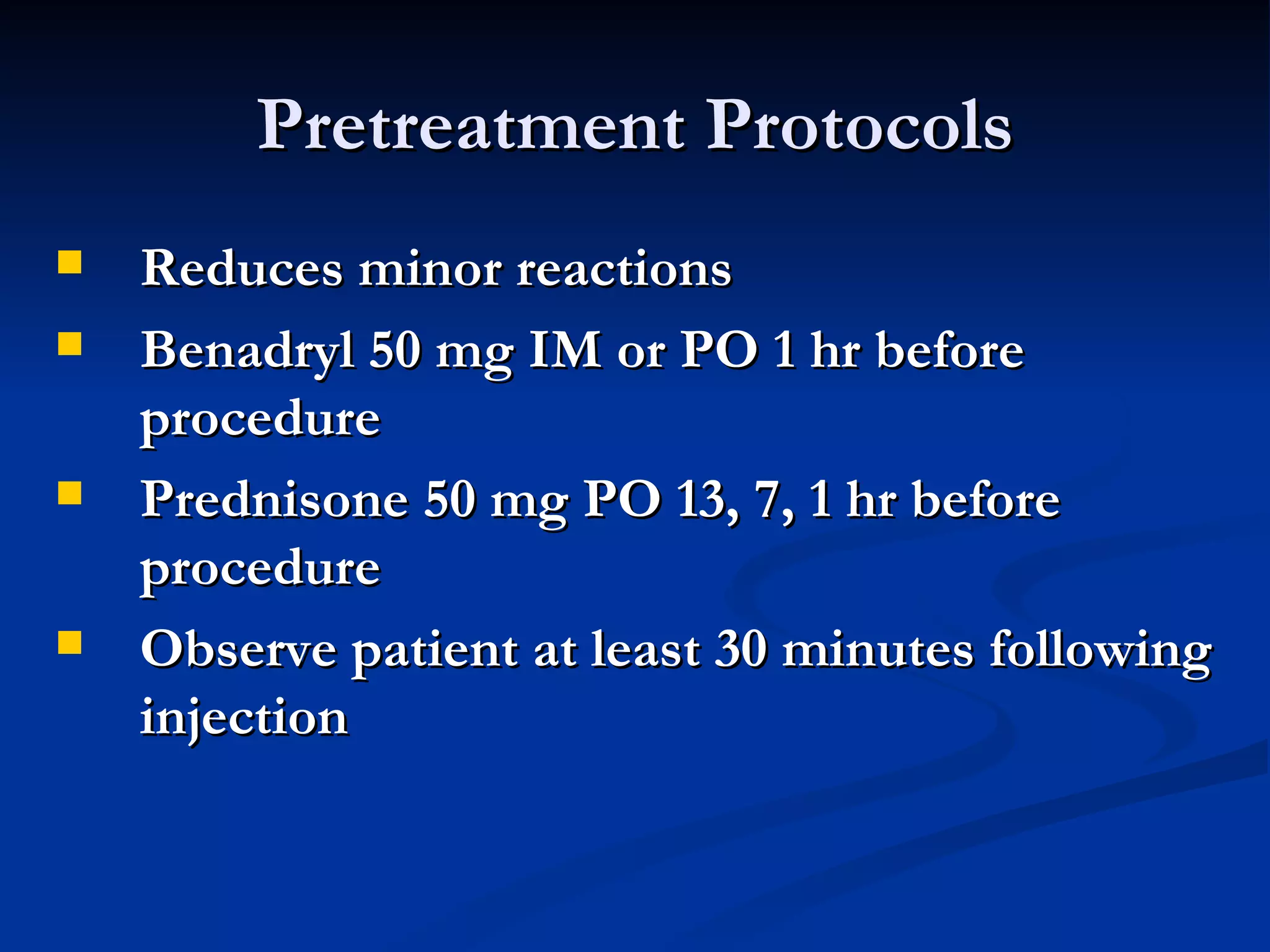
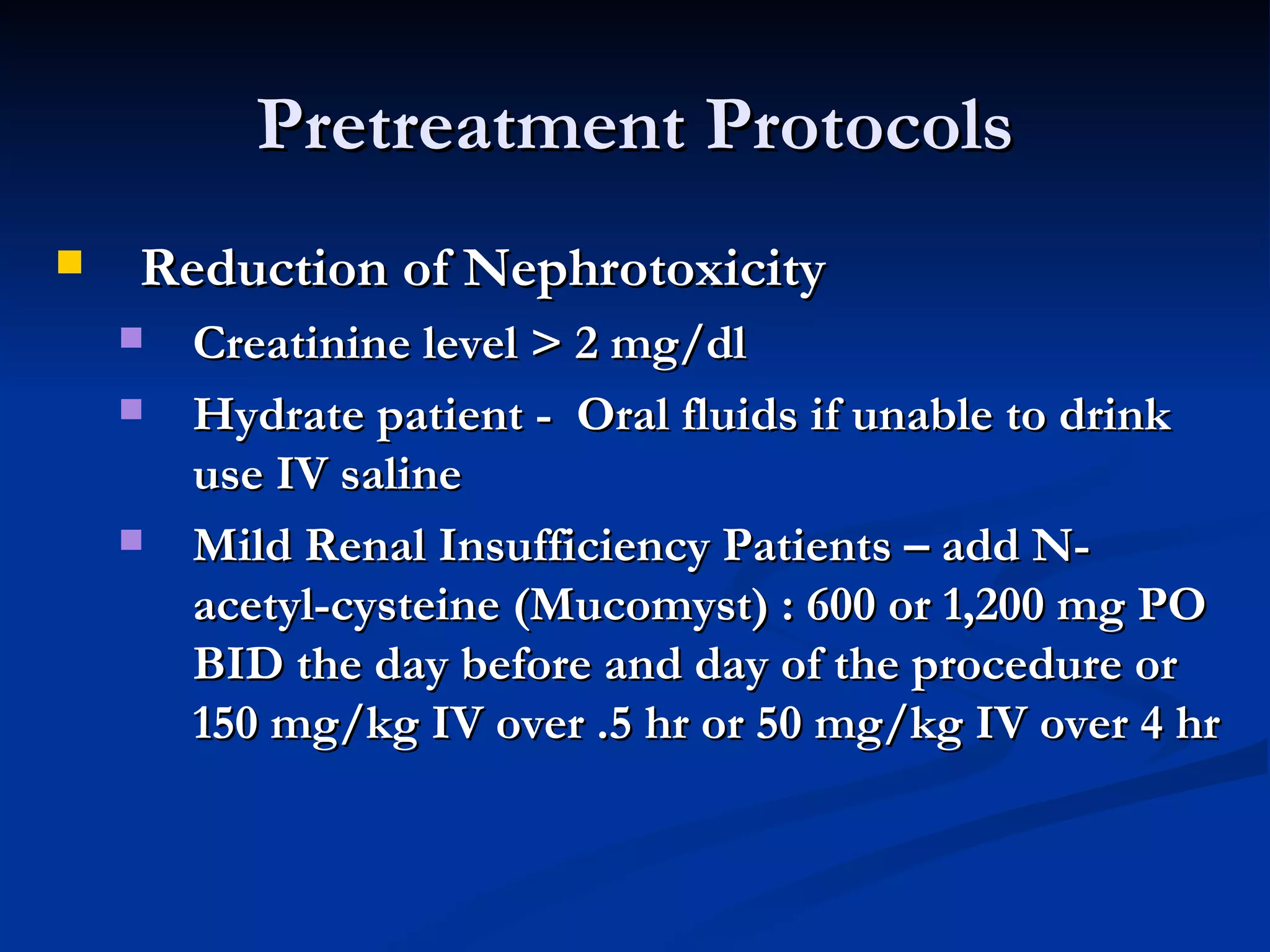
Contrast agents are compounds used to improve visibility of internal structures in images. Common types are iodine-based radiographic agents that can be ionic or non-ionic, and vary in osmolality. While contrast reactions are generally mild, severe reactions including anaphylaxis can occur. Risk factors include a history of previous reactions or asthma. Treatment depends on symptoms but may include epinephrine, steroids, oxygen and IV fluids. Proper screening, hydration and pre-treatment can help reduce risks of reactions and nephrotoxicity.