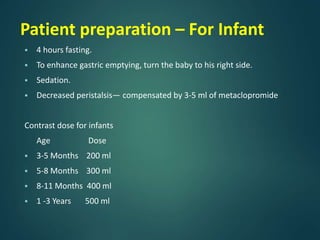
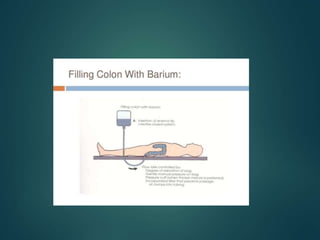
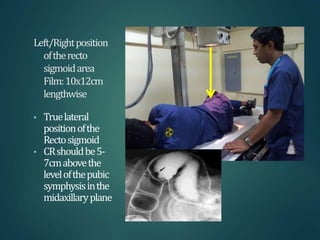
This document provides information about barium procedures, including barium swallow, barium meal, and barium follow through examinations. It defines barium as a radioopaque contrast agent used to provide a roadmap of GI tract pathologies in x-ray exams. Barium sulphate is commonly used because it is non-toxic, non-absorbable, and coats the mucosa, allowing double contrast studies. The document describes the techniques, positions, and views used in various barium exams to visualize the esophagus, stomach, and small intestine. It also lists common indications, contraindications, and complications.