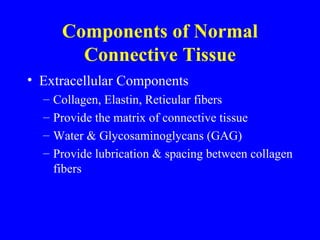
1. Normal connective tissue contains collagen, elastin, proteoglycans, water, and fibroblasts that provide structure and allow movement.
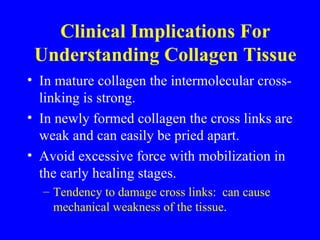
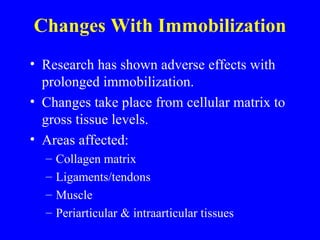
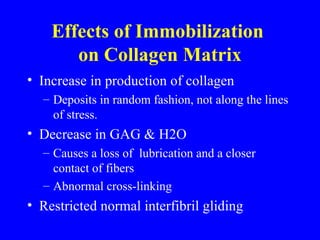
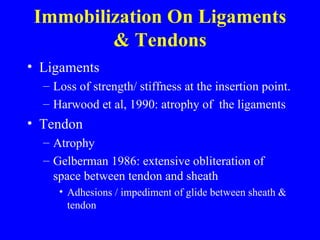
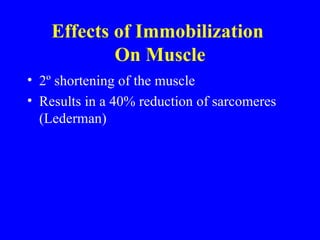
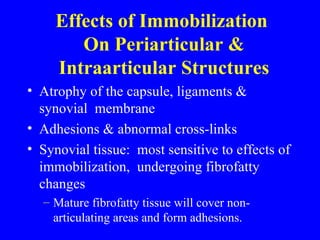
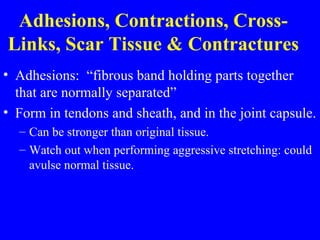
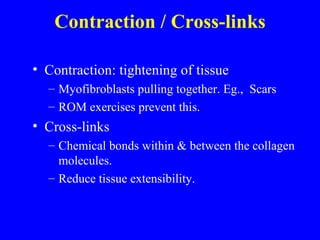
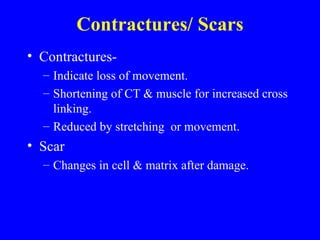
2. Immobilization causes the collagen matrix to deposit randomly without lubrication, increased cross-linking, and adhesion formation in ligaments, tendons and muscles.
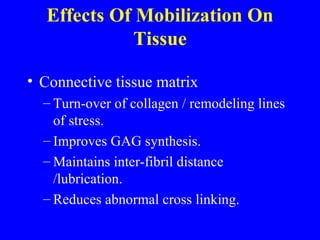
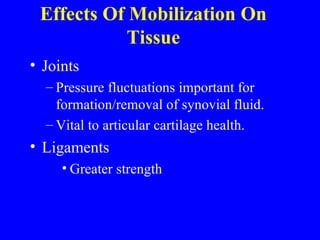
3. Mobilization improves the collagen matrix organization, lubrication, vascularization and strength of connective tissue, muscles and joints while decreasing adhesions.