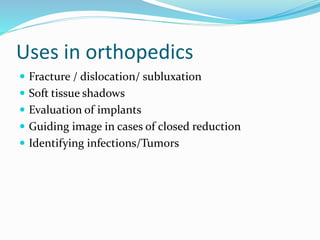
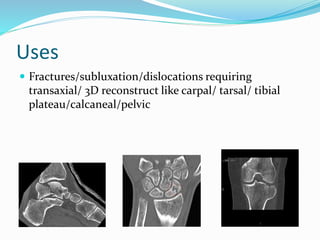
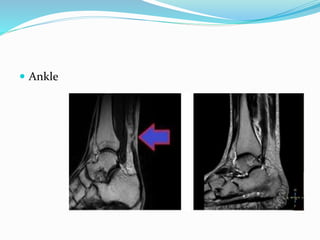
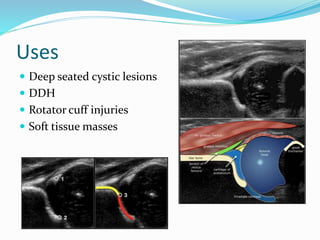
This document discusses various imaging modalities used in orthopedics, including their mechanisms and uses. It covers conventional x-rays, computed tomography, magnetic resonance imaging, ultrasound, nuclear medicine techniques like PET and bone scintigraphy, and bone densitometry. X-rays remain a commonly used first-line test due to low cost and radiation exposure. CT provides cross-sectional imaging while MRI enables excellent soft tissue contrast without radiation. Emerging techniques like PET allow functional imaging of disease processes. Overall, selecting the appropriate imaging modality depends on the diagnostic question and each has advantages and limitations for orthopedic applications.