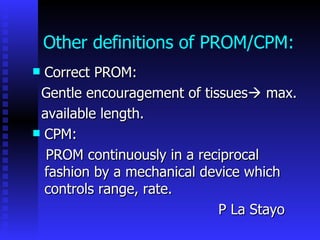
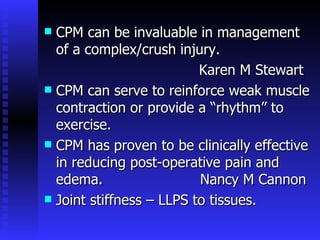
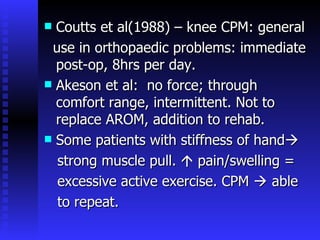
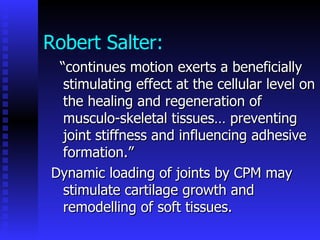
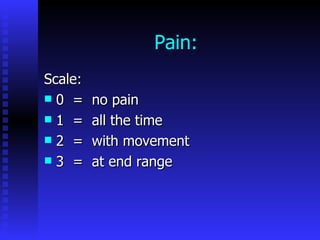
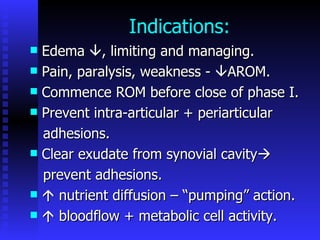
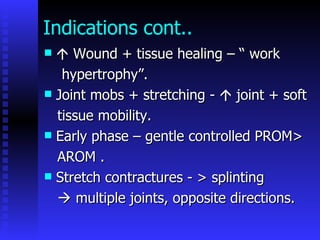
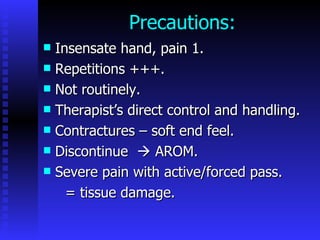
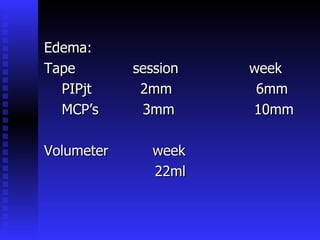
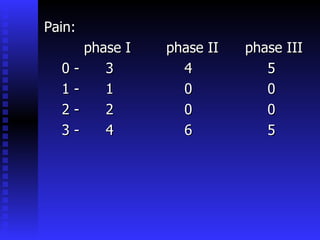
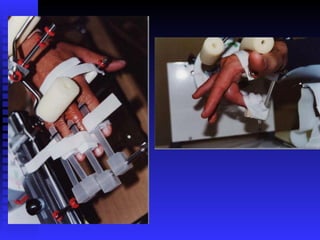
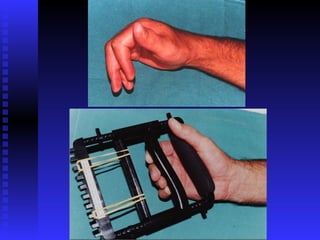
The document discusses the use of continuous passive motion (CPM) machines in hand therapy. It describes how CPM machines can help increase range of motion, decrease edema and pain, and prevent joint stiffness following injuries or surgeries by continuously moving the joints in a gentle, passive motion. Research shows CPM is effective for reducing postoperative pain and swelling and can help reinforce muscle contraction. The document concludes that CPM is a valuable tool in hand therapy for improving range of motion and decreasing edema and pain.