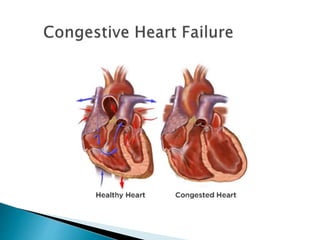
1. Heart failure is the inability of the heart to pump sufficient blood to meet the tissues' needs for oxygen and nutrients.
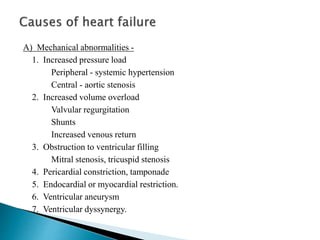
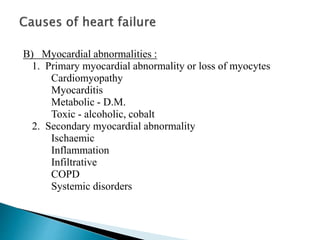
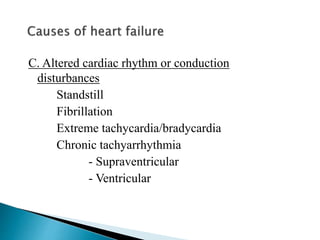
2. It can be caused by mechanical abnormalities of the heart, myocardial abnormalities, or altered cardiac rhythm/conduction disturbances.
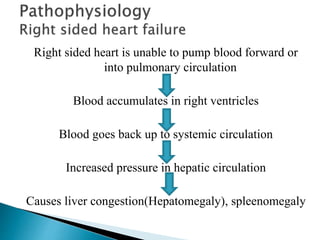
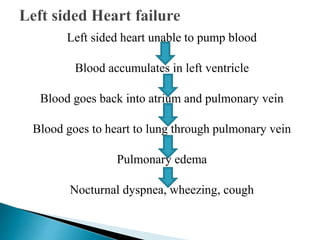
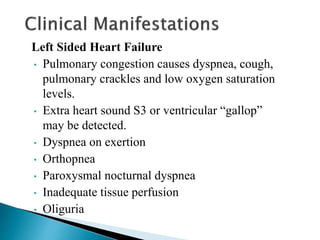
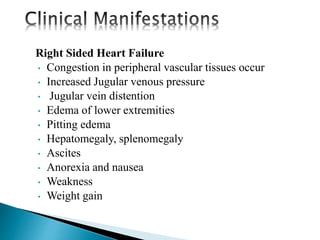
3. Symptoms of heart failure depend on whether the left or right side of the heart is affected and include shortness of breath, edema, fatigue, cough, and liver/spleen enlargement.