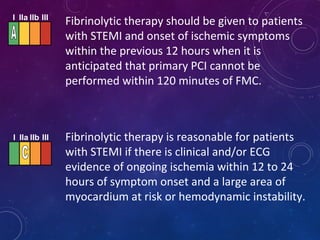
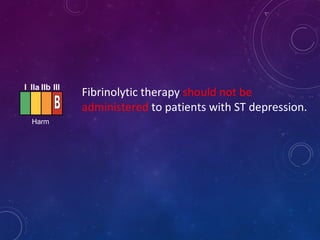
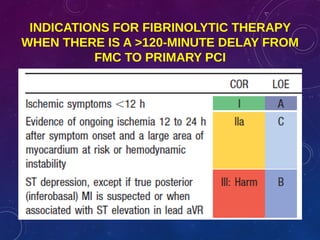
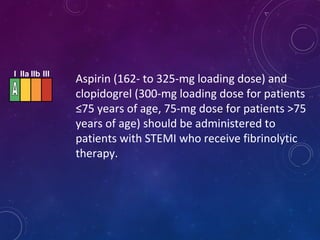
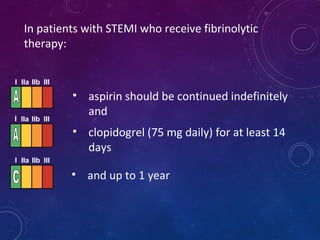
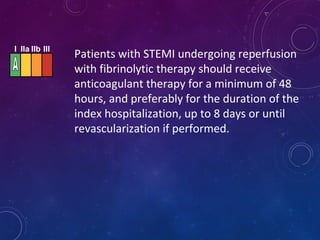
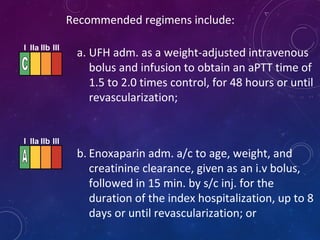
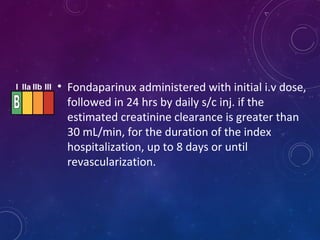
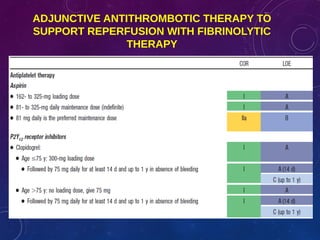
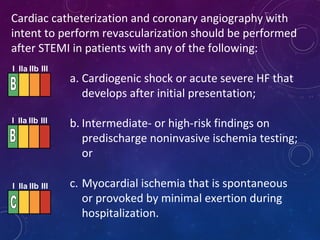
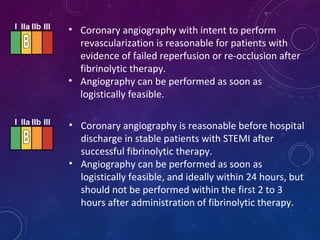
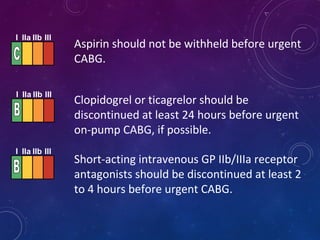
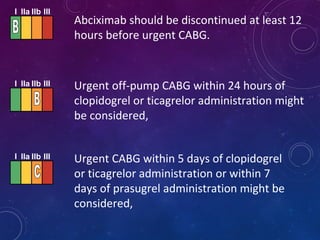
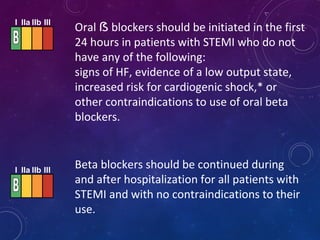
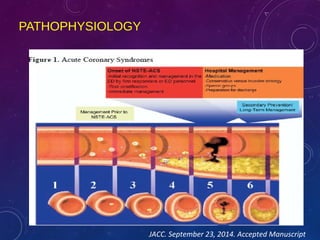
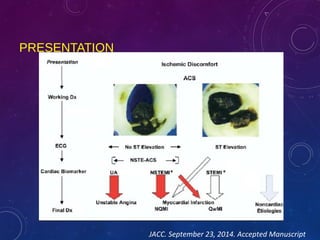
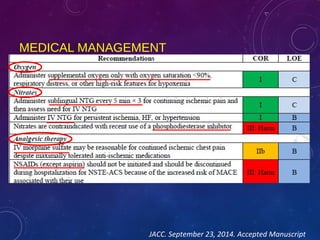
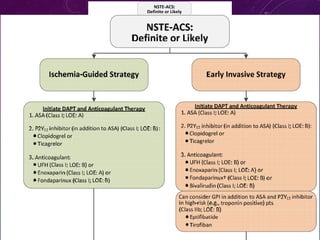
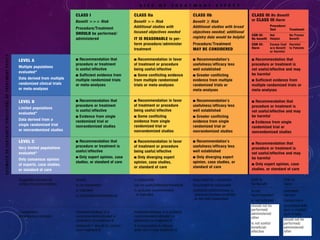
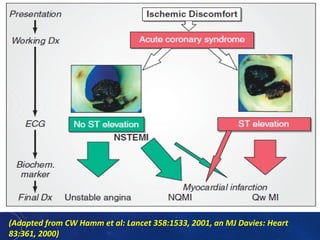
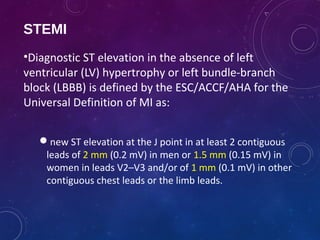
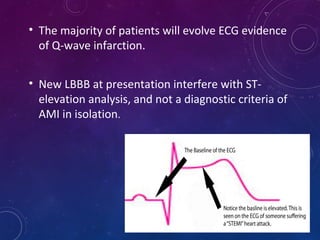
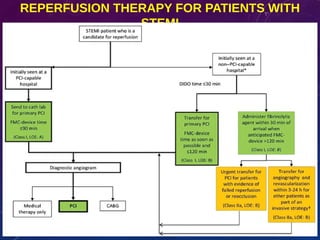
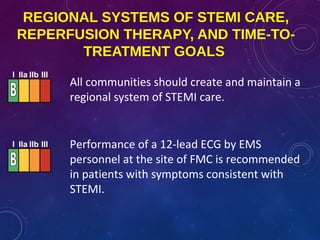
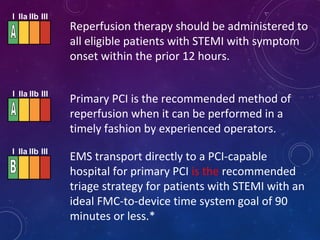
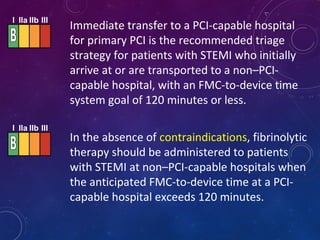
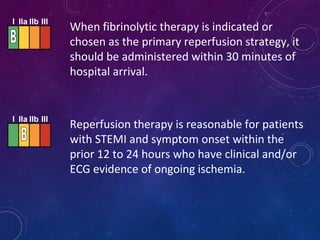
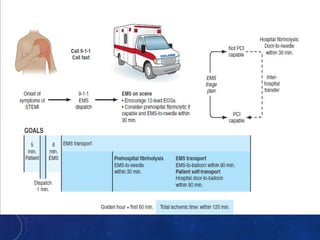
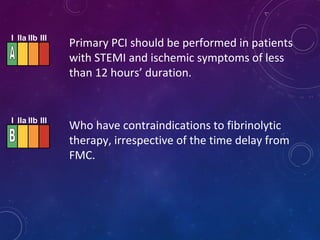
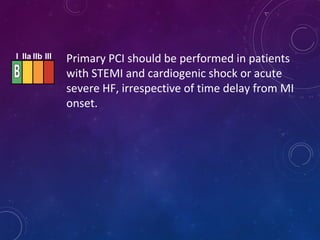
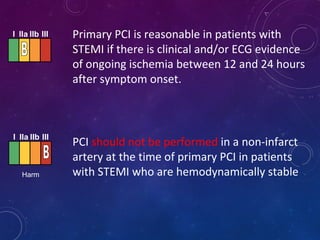
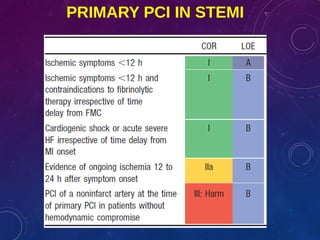
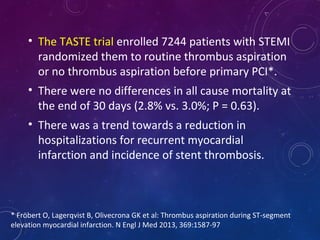
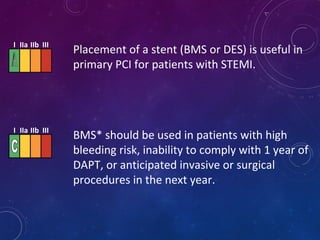
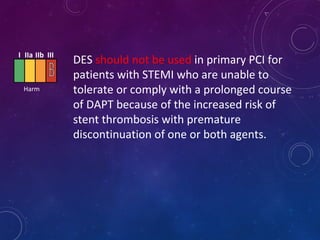
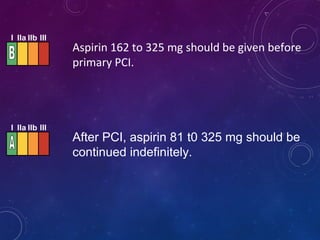
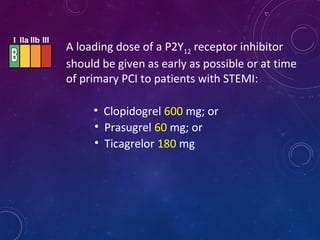
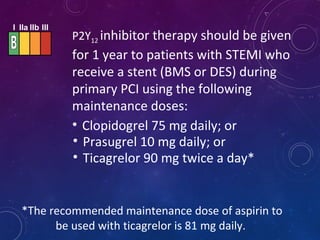
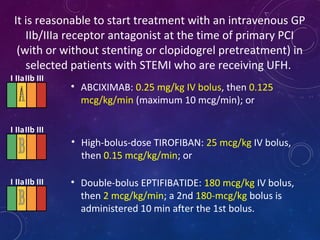
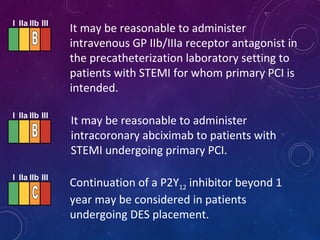
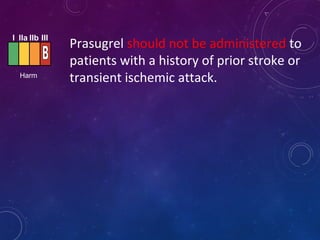
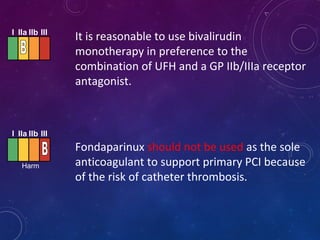
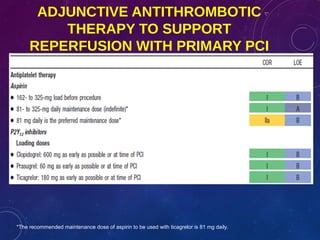
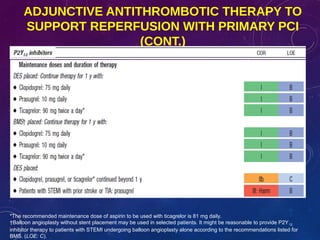
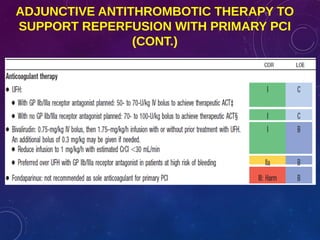
This document summarizes guidelines for the management of ST-elevation myocardial infarction (STEMI) and non-ST-elevation myocardial infarction (NSTEMI). It discusses epidemiology of cardiovascular disease globally and in India. It provides classifications for recommendations and levels of evidence. It discusses diagnostic criteria for STEMI and goals for regional STEMI systems including time to treatment. It provides recommendations for reperfusion therapy including primary percutaneous coronary intervention (PCI) and fibrinolytic therapy. It also discusses adjunctive antithrombotic therapies to support primary PCI such as antiplatelet agents, anticoagulants, and glycoprotein IIb/IIIa inhibitors.
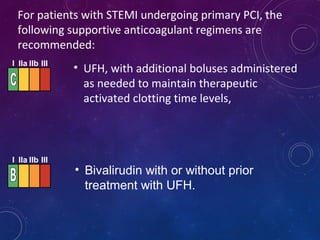
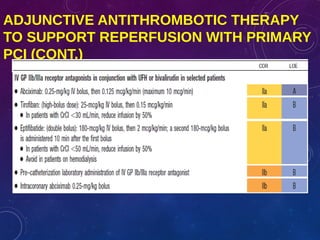
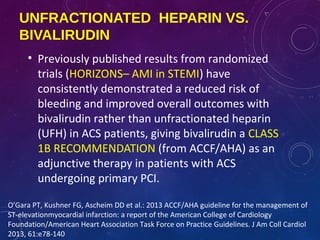
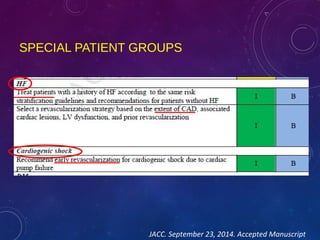
![• The benefits of bivalirudin are mainly in its ability
to reduce bleeding risk.
• Retrospective analysis from Sweden’s SCAAR
database (41,537 consecutive NSTE–ACS patients
none of whom received GP IIb/III inhibitors)
revealed no benefits from using bivalirudin rather
than heparin.
• Head to head trials comparing bivalirudin with
unfractionated heparin (VALIDATE–SWEDEHEART,
HEAT–PPCI) are currently underway.
Swedish registry questions superiority of bivalirudin over heparin in patients undergoing PCI
for NSTE-ACS. [http://www.escardio.org/about/press/press-releases/pr-13/Pages/europcr-
day1.aspx - registry].](https://image.slidesharecdn.com/acssteminstemiua-150330114328-conversion-gate01/85/Acs-stemi-nstemi-ua-43-320.jpg)