The document discusses several national nutritional programs launched by the Indian government to address major nutritional deficiency diseases. It provides details on the following programs:
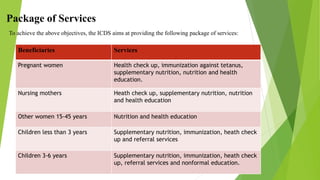
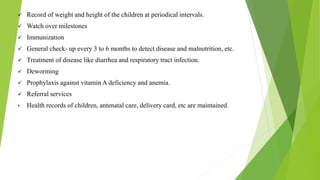
1. Integrated Child Development Scheme (ICDS) which provides supplementary nutrition, immunization, health checkups and education to children and mothers.
2. Mid-Day Meal Program which aims to provide at least one-third of daily nutritional needs to primary school children through free cooked meals.
3. National Program for Control of Blindness which aims to prevent vitamin A deficiency through supplementation and education.
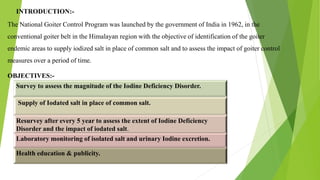
4. Iodine Deficiency Disorders Program which aims to eliminate iodine deficiency through universal salt iodization and monitoring.