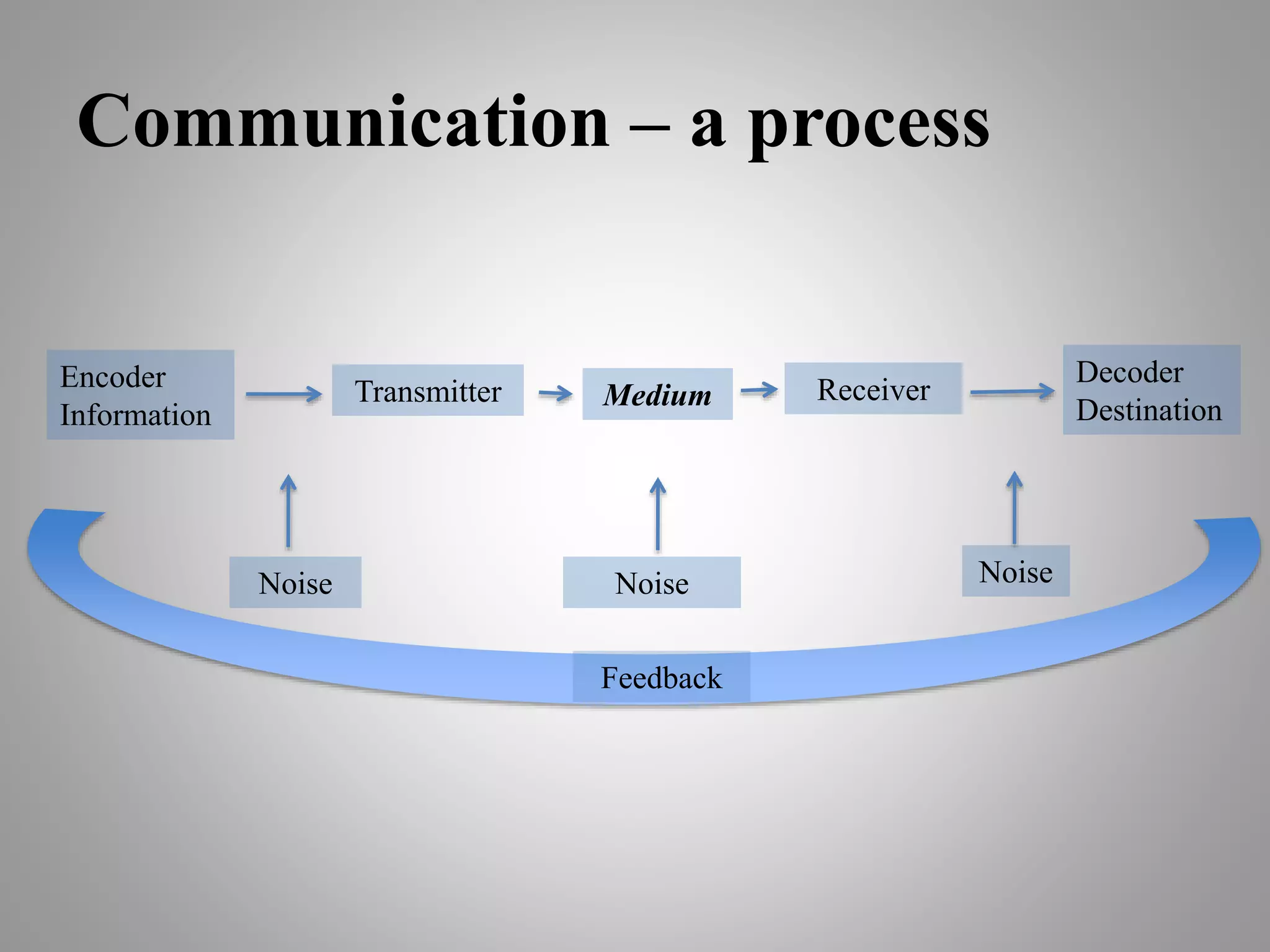
This document discusses the importance of effective communication in emergency medical settings. It notes that the emergency room is an uncontrolled environment with many patients, anxieties, interruptions and legal issues. Good communication can improve patient health and satisfaction, enhance teamwork and decrease litigation. The document recommends establishing rapport, gathering information, providing information to patients, addressing concerns, and using clear documentation and handovers. Effective communication is key to ensuring patient safety, quality care and satisfaction in high-pressure emergency departments.