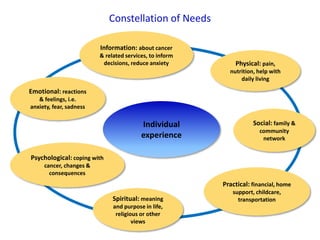
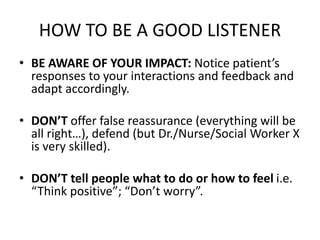
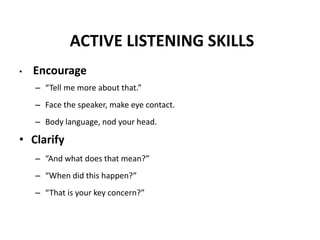
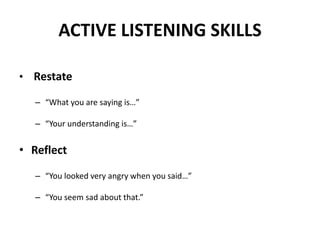
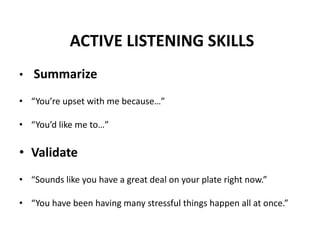
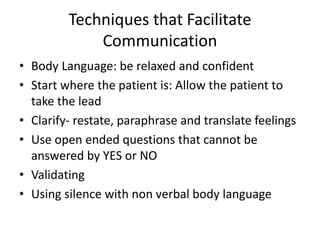
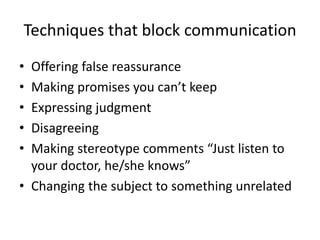
The document outlines effective communication skills and active listening techniques, particularly in the context of patient care and support for individuals facing cancer. It emphasizes the importance of empathy, understanding emotions, and adapting communication to meet patients' needs. Key strategies include active listening, validating feelings, avoiding assumptions, and using open-ended questions to facilitate meaningful conversations.
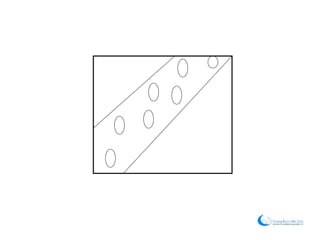



![Scenario
• “I have gone from the body of an active 18 year old doing pretty
much whatever I wanted, to a much weaker and more fragile one. [I
had a] seemingly never ending list of complications ranging from
routine fevers to pancreatitis, which caused severe pain attacks and
further complications which I am still dealing with. This may have
been the most trying period mentally as well, because it seemed
like I got a never ending stream of bad news.
• I did not really want to make my issues public, especially at first... I
find that I have to make an effort to will myself to go out and be
with my friends.
• [Cancer] has forced me to sit back and take a look at life and what it
means, who I am and where I am going... as well as seeing the value
of just living day to day, for the moment.”
[Young man, diagnosed with Leukemia]](https://image.slidesharecdn.com/presentationjunestudents-2-160623213121/85/Communication-Skills-and-Focused-Listening-Module-22-320.jpg)