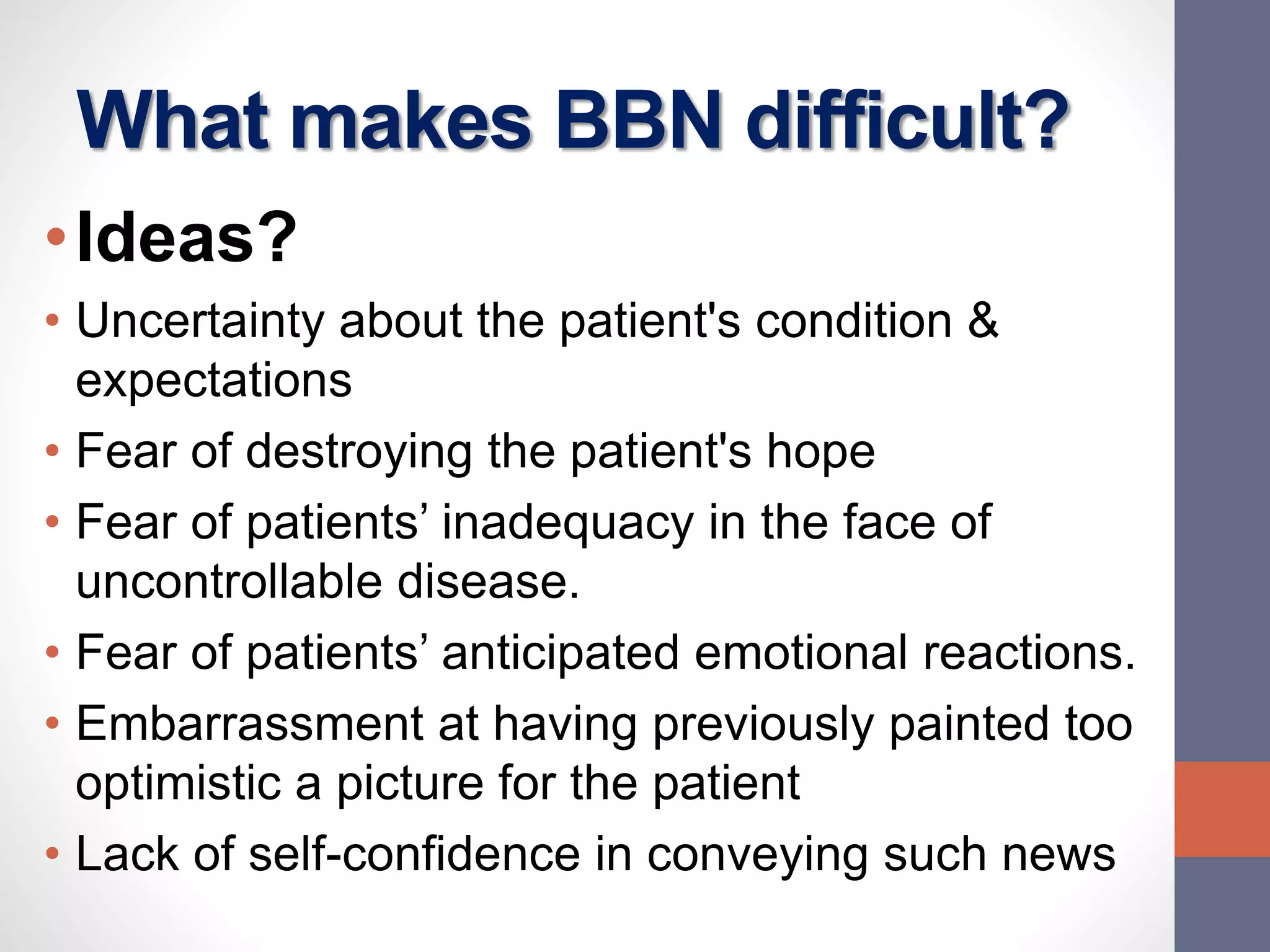
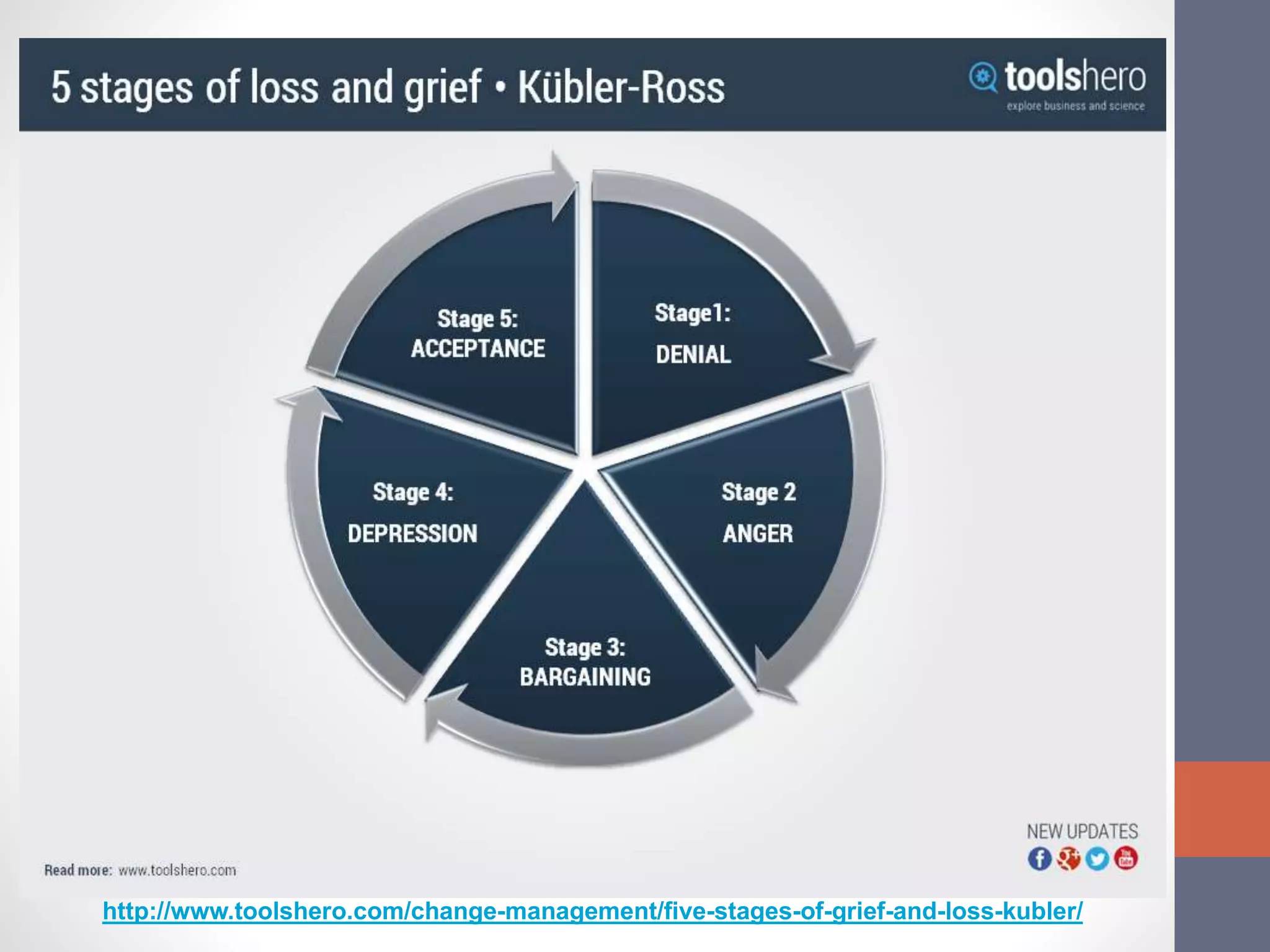
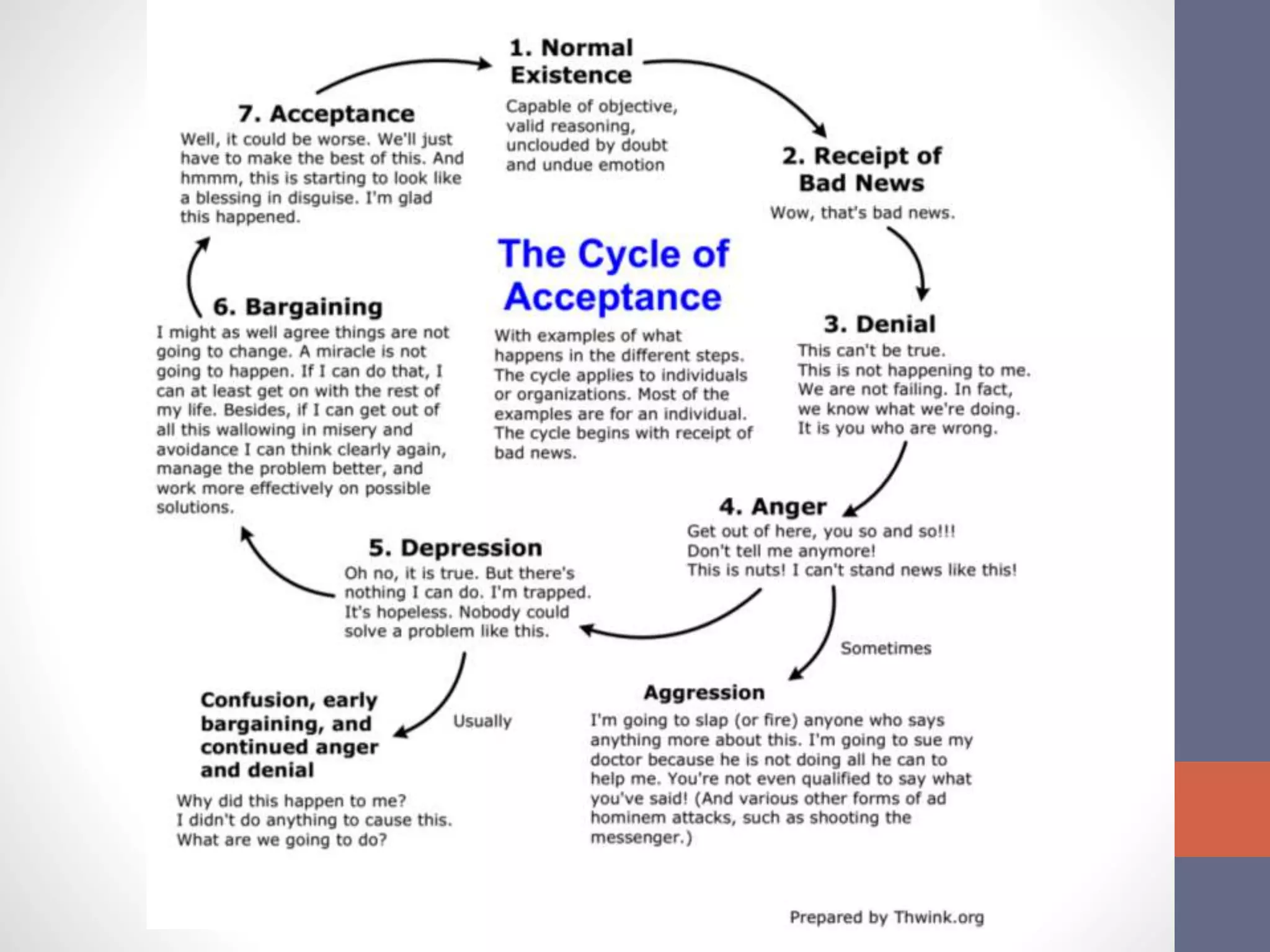
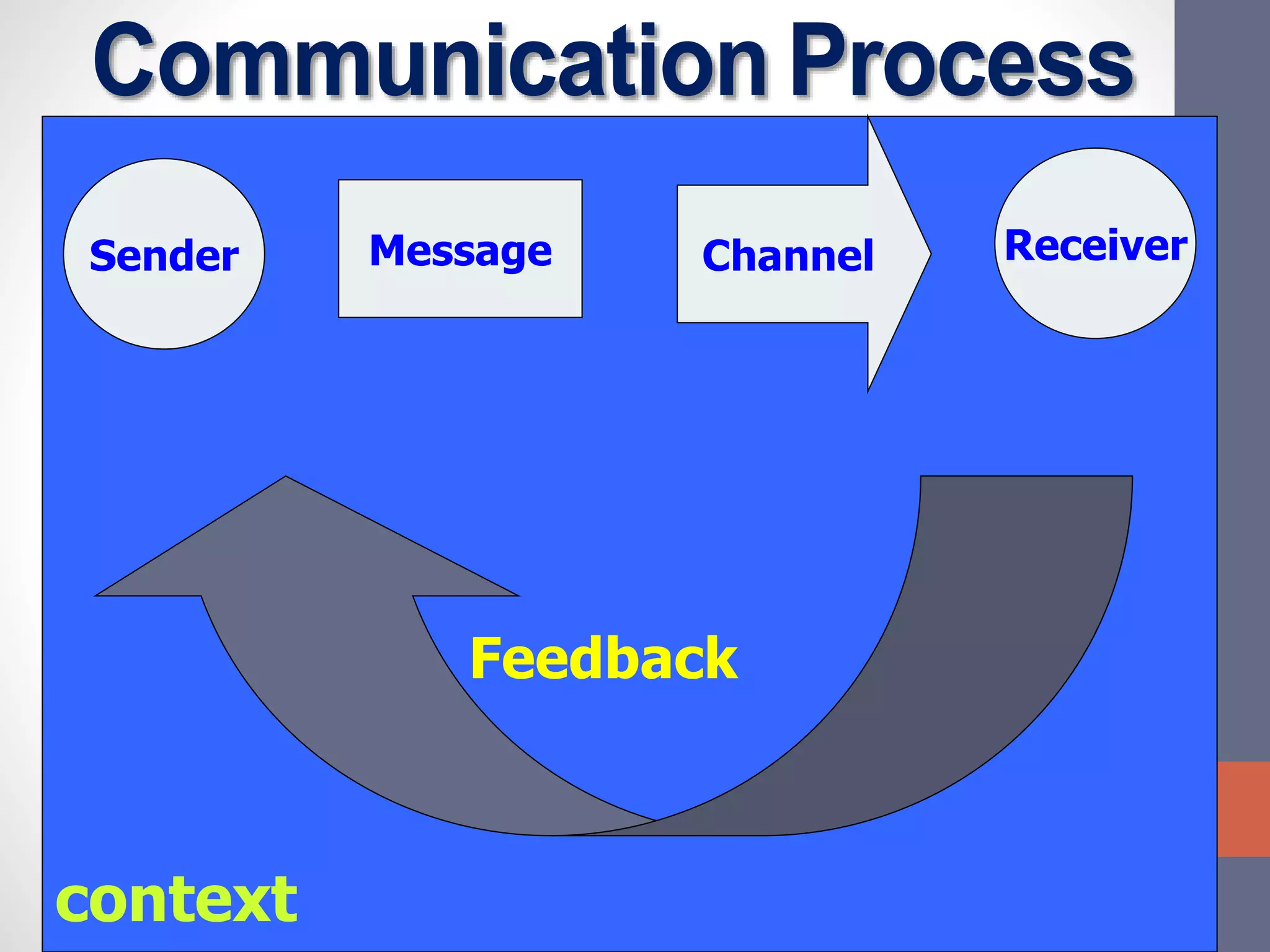
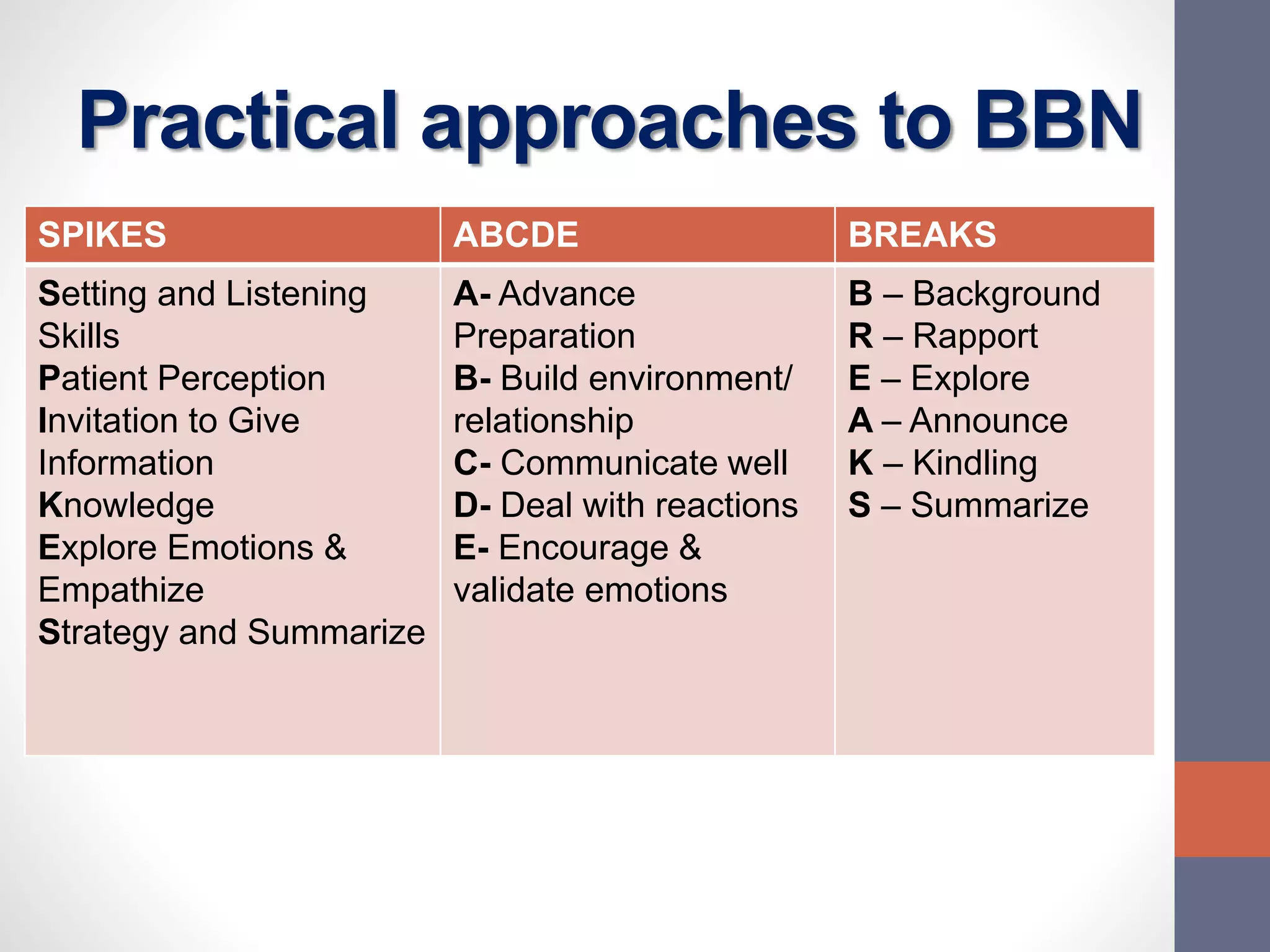
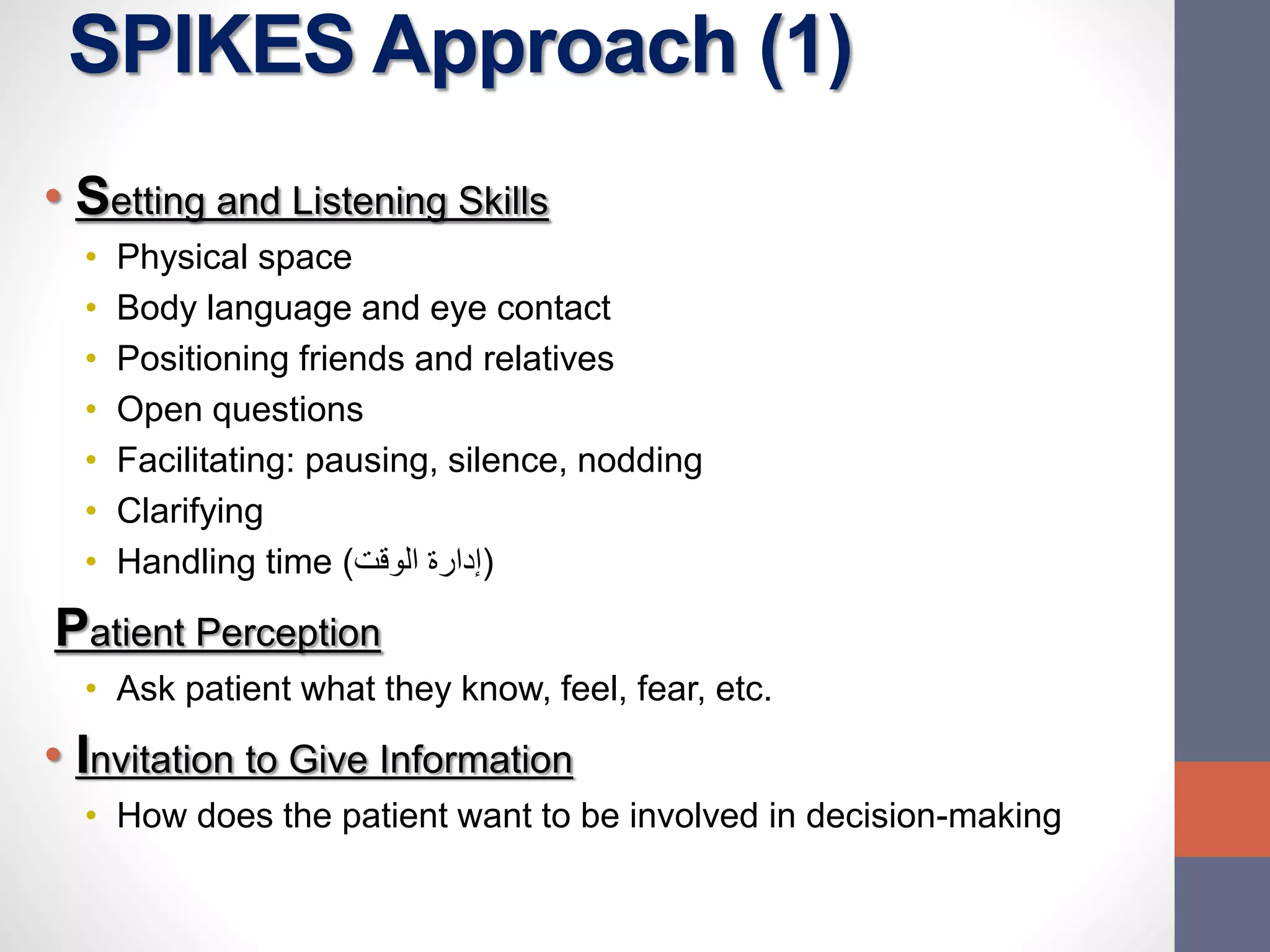
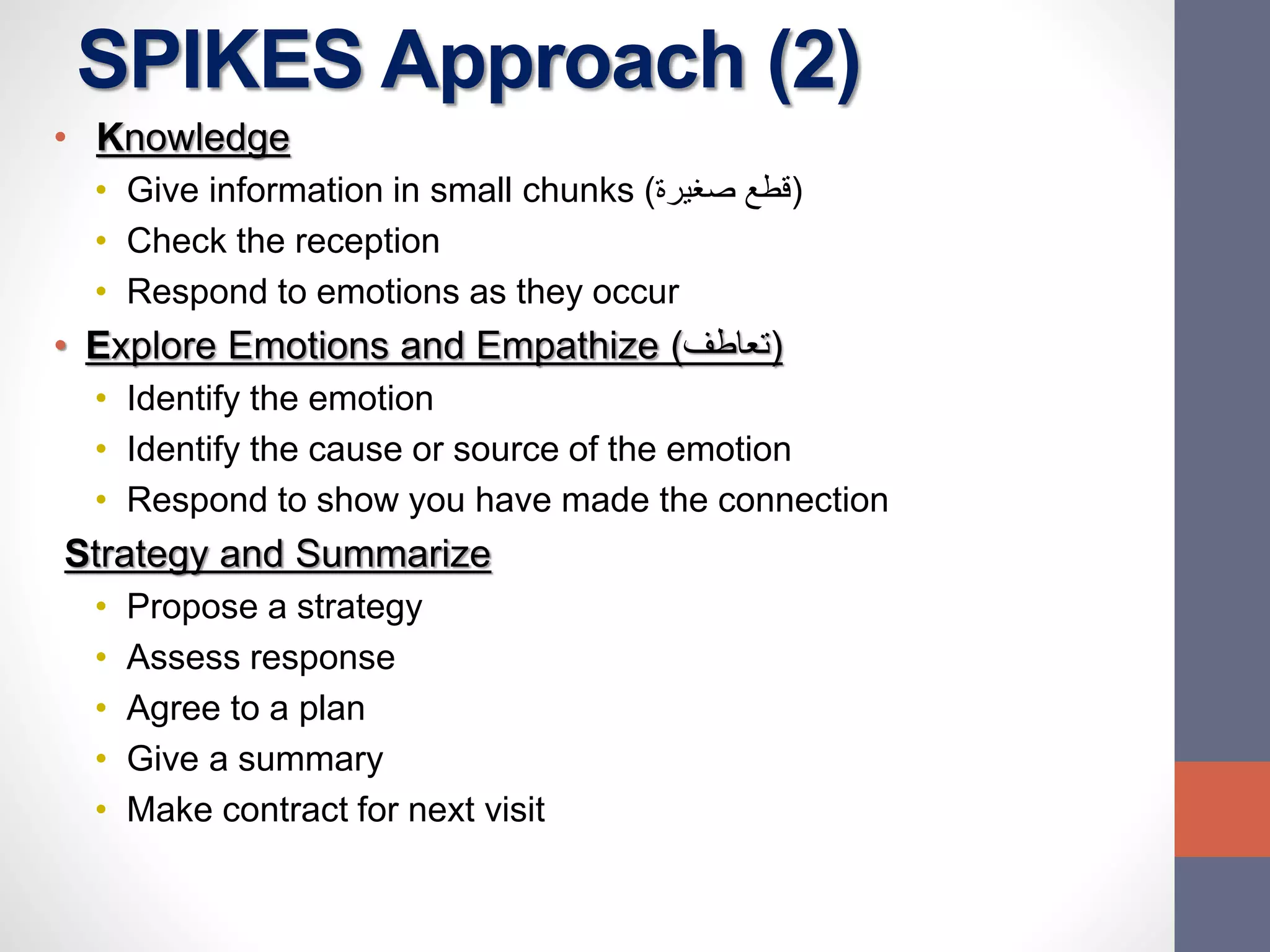
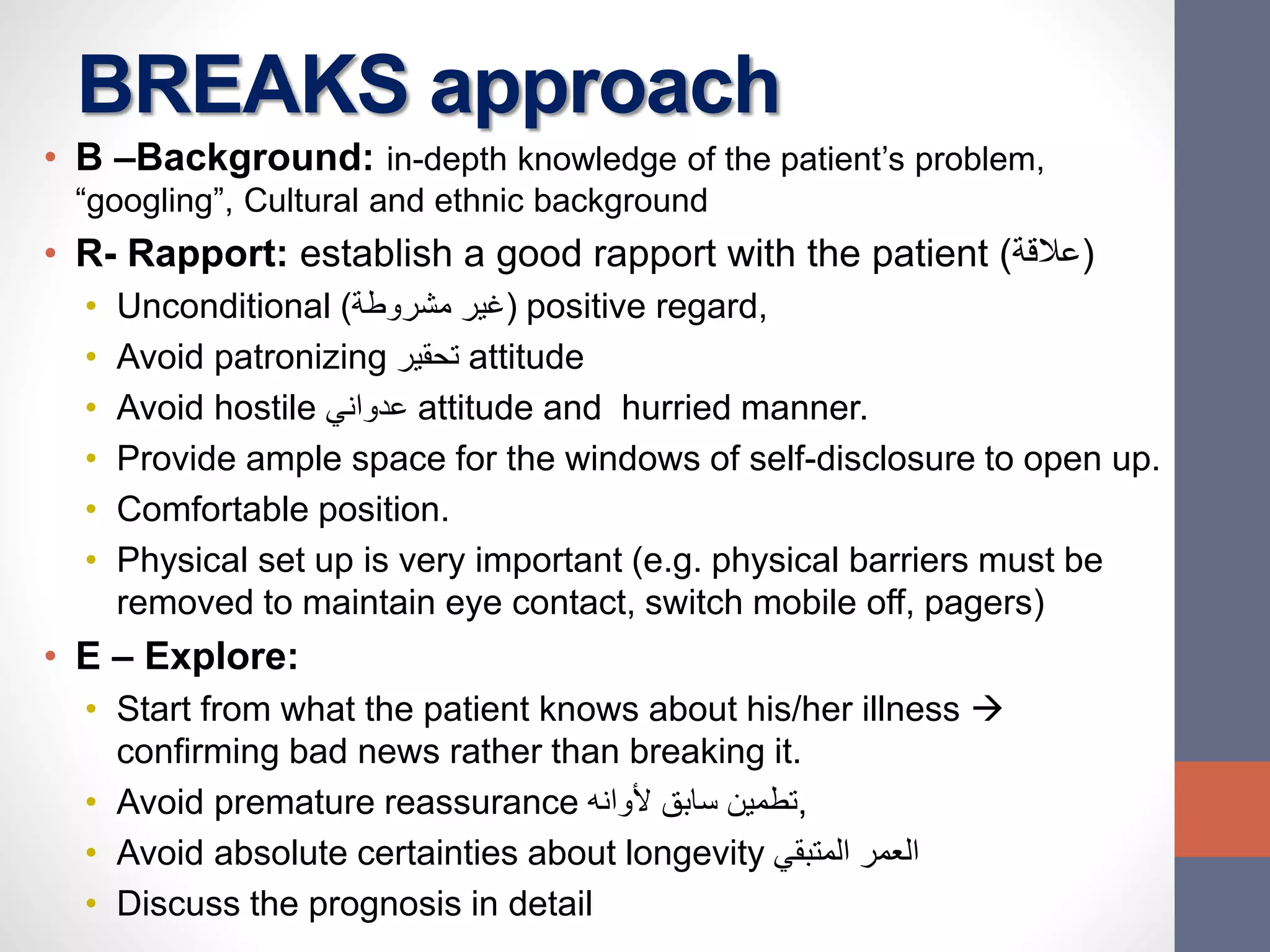
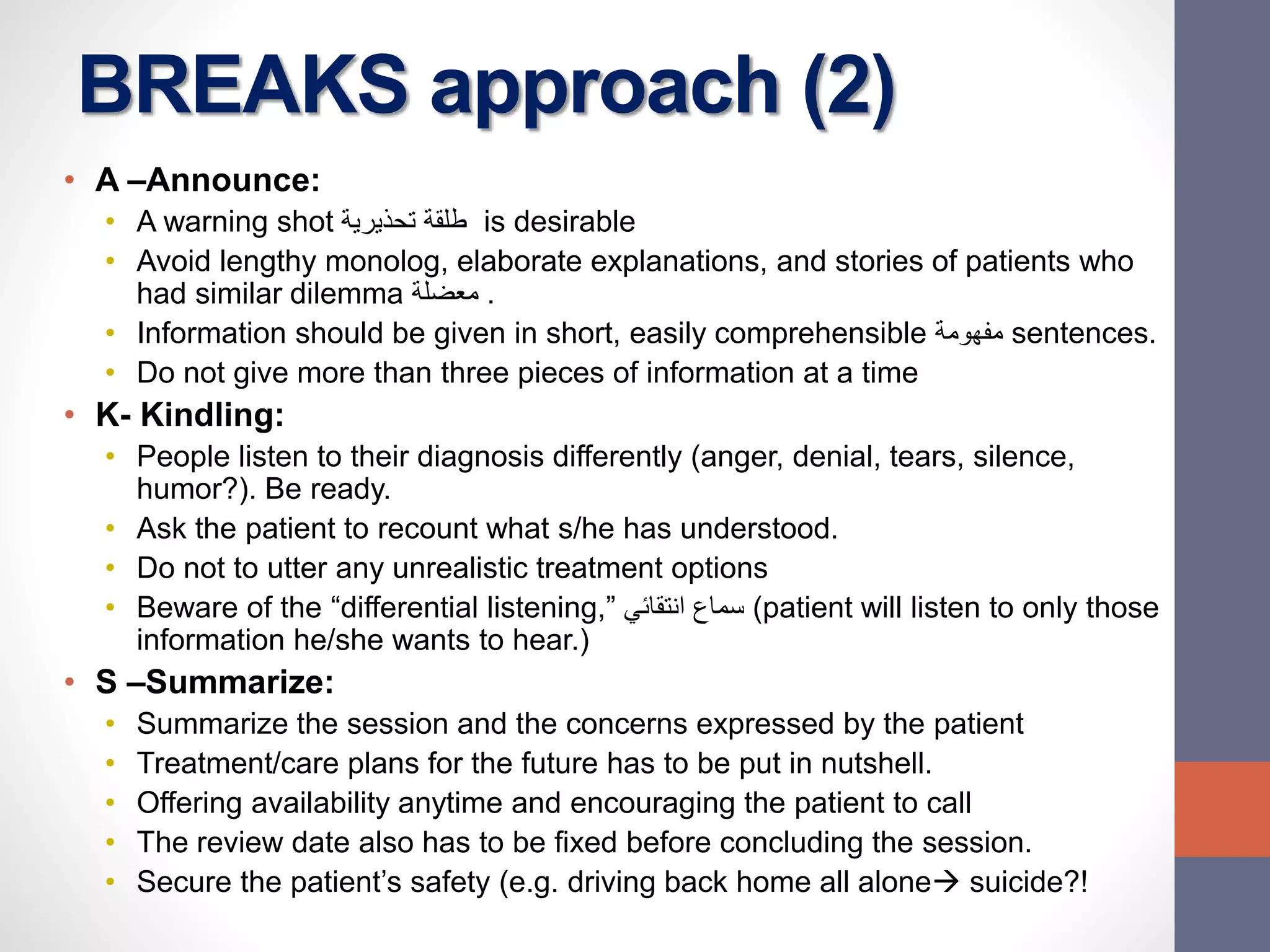
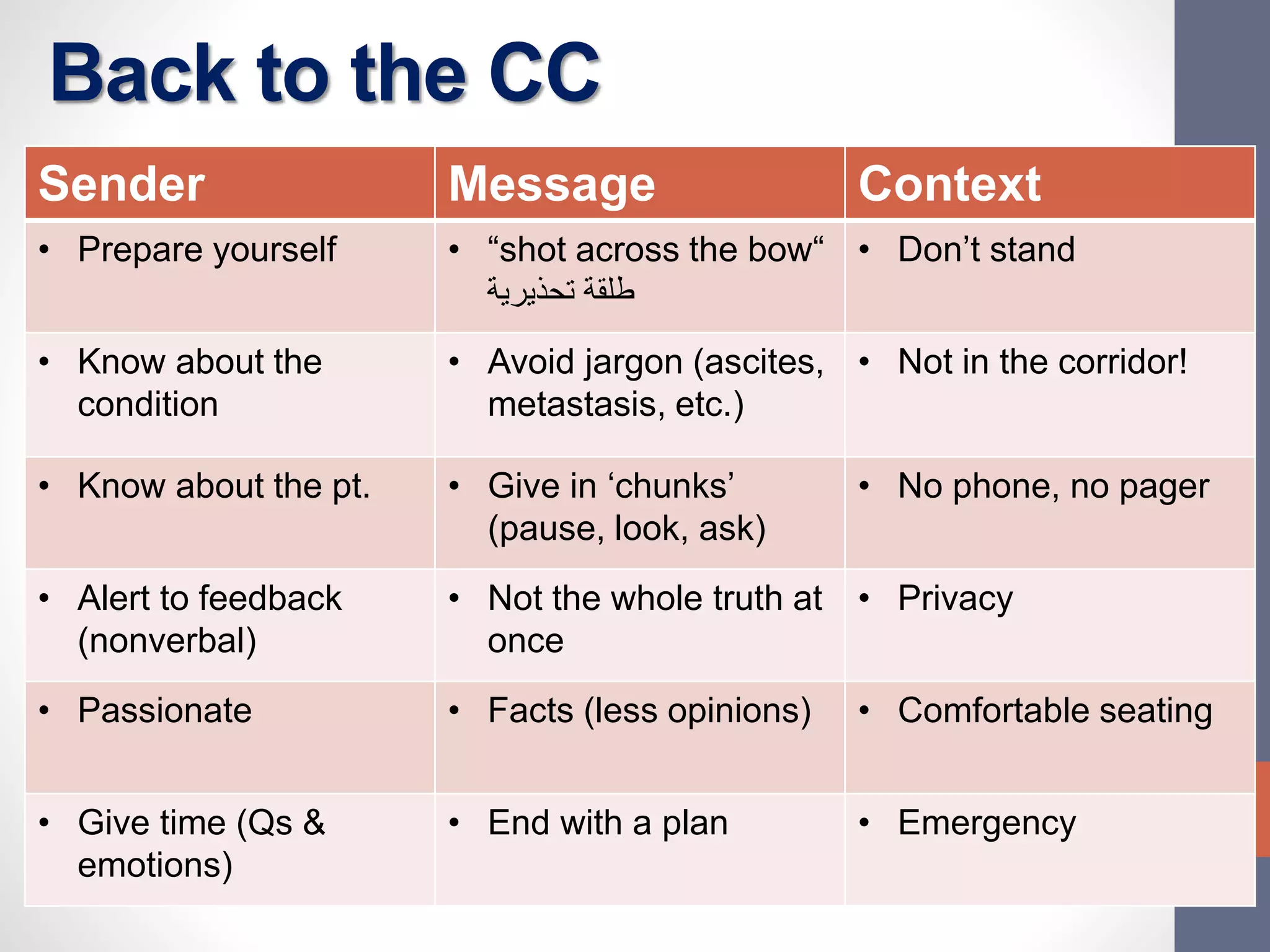
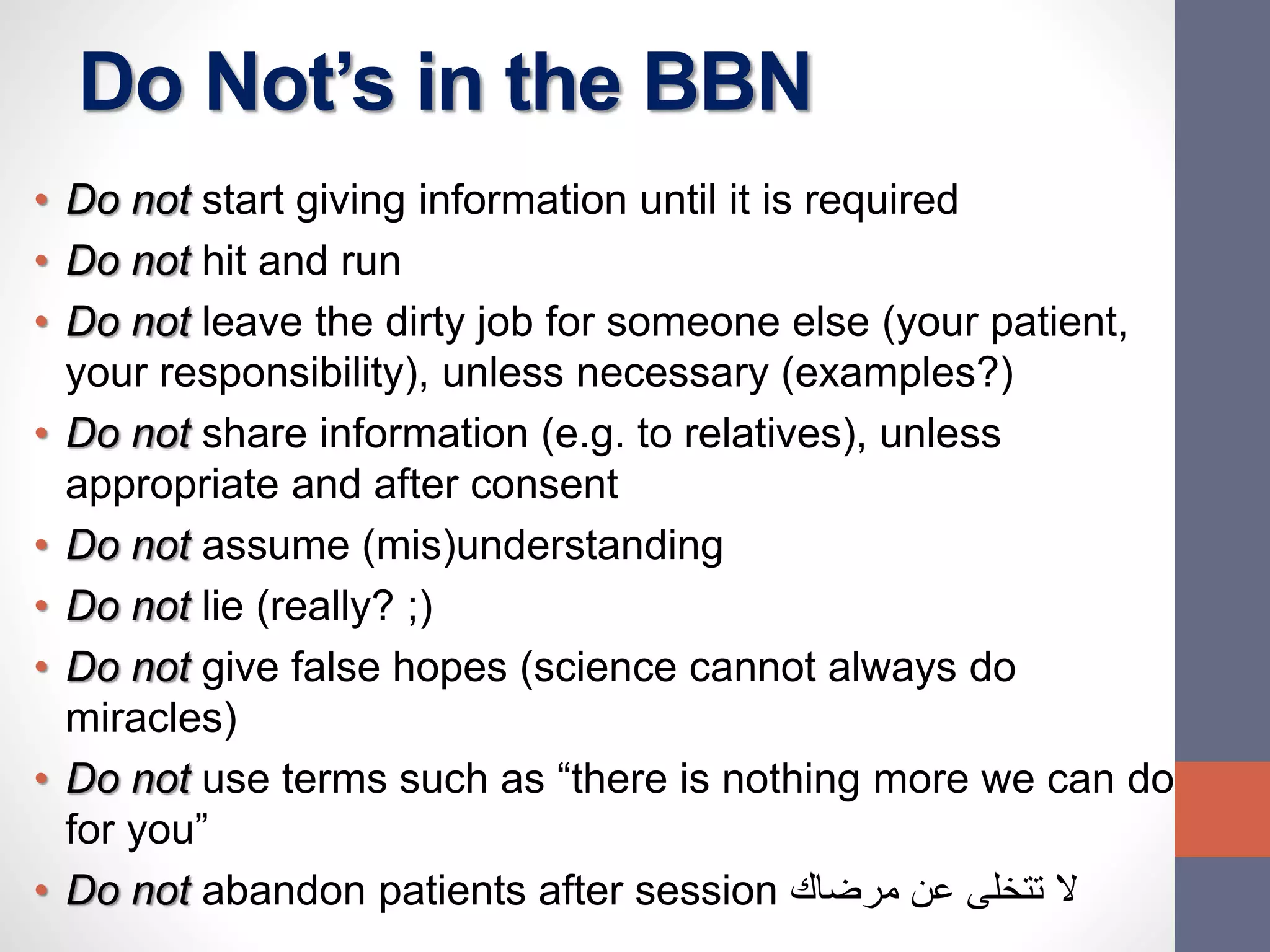
The document discusses the complexities and importance of breaking bad news (BBN) in a medical context, emphasizing ethical, legal, and professional responsibilities. It defines bad news, explores practical communication strategies such as the SPIKES and ABCDE frameworks, and highlights the emotional reactions patients may have, including the stages of grief. The document also addresses key considerations for effective communication, including preparation, empathy, and patient involvement.