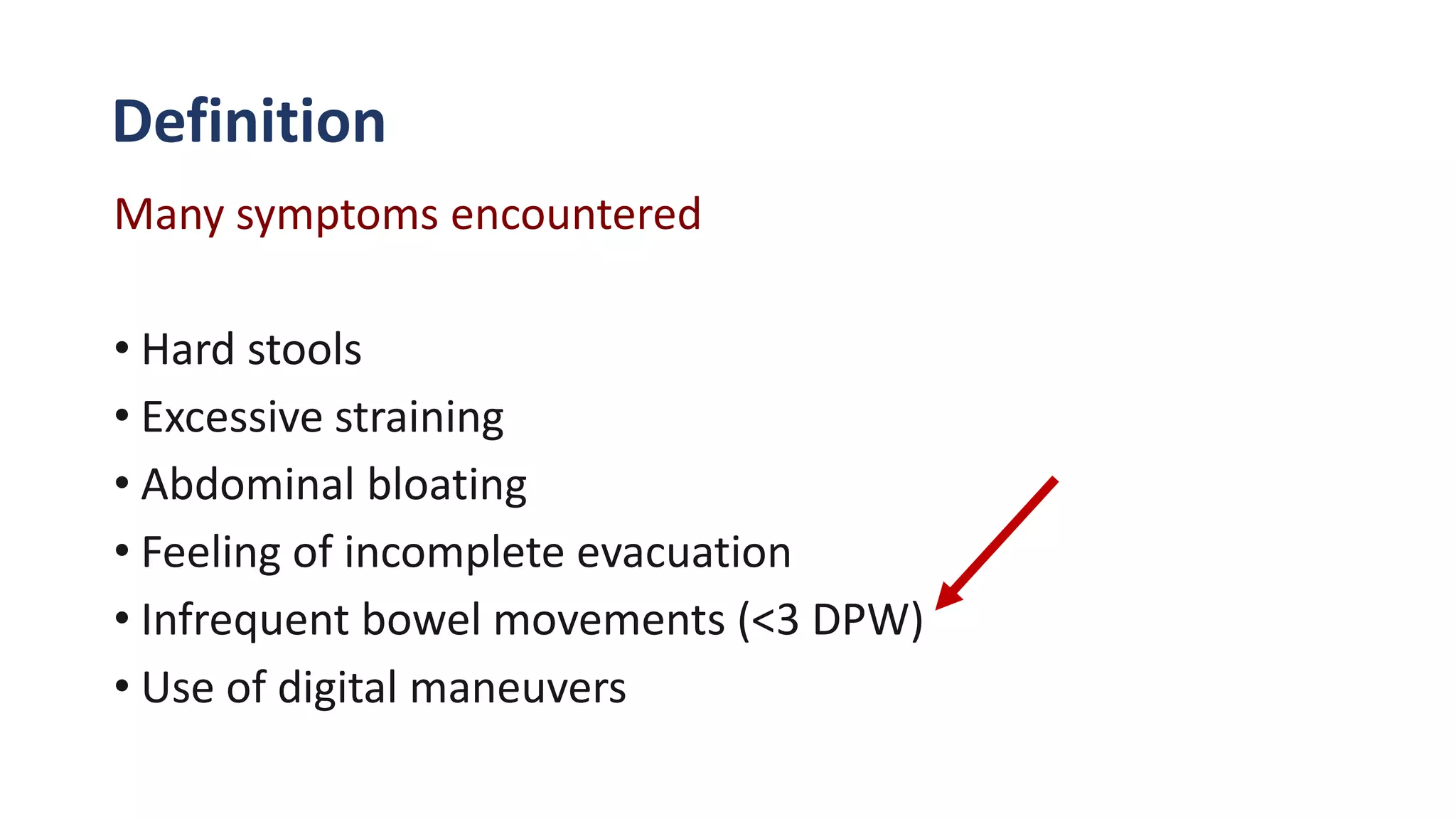
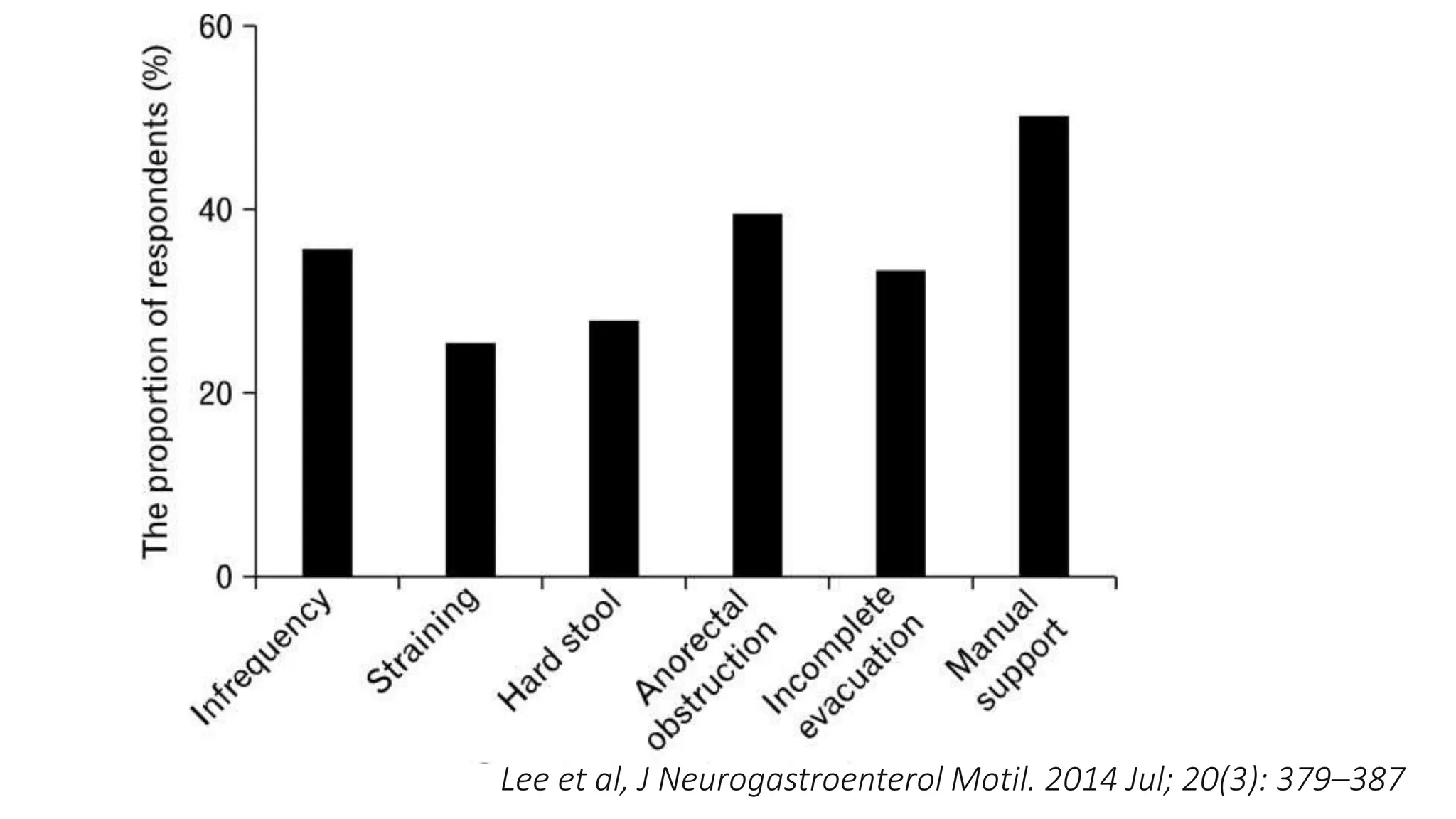
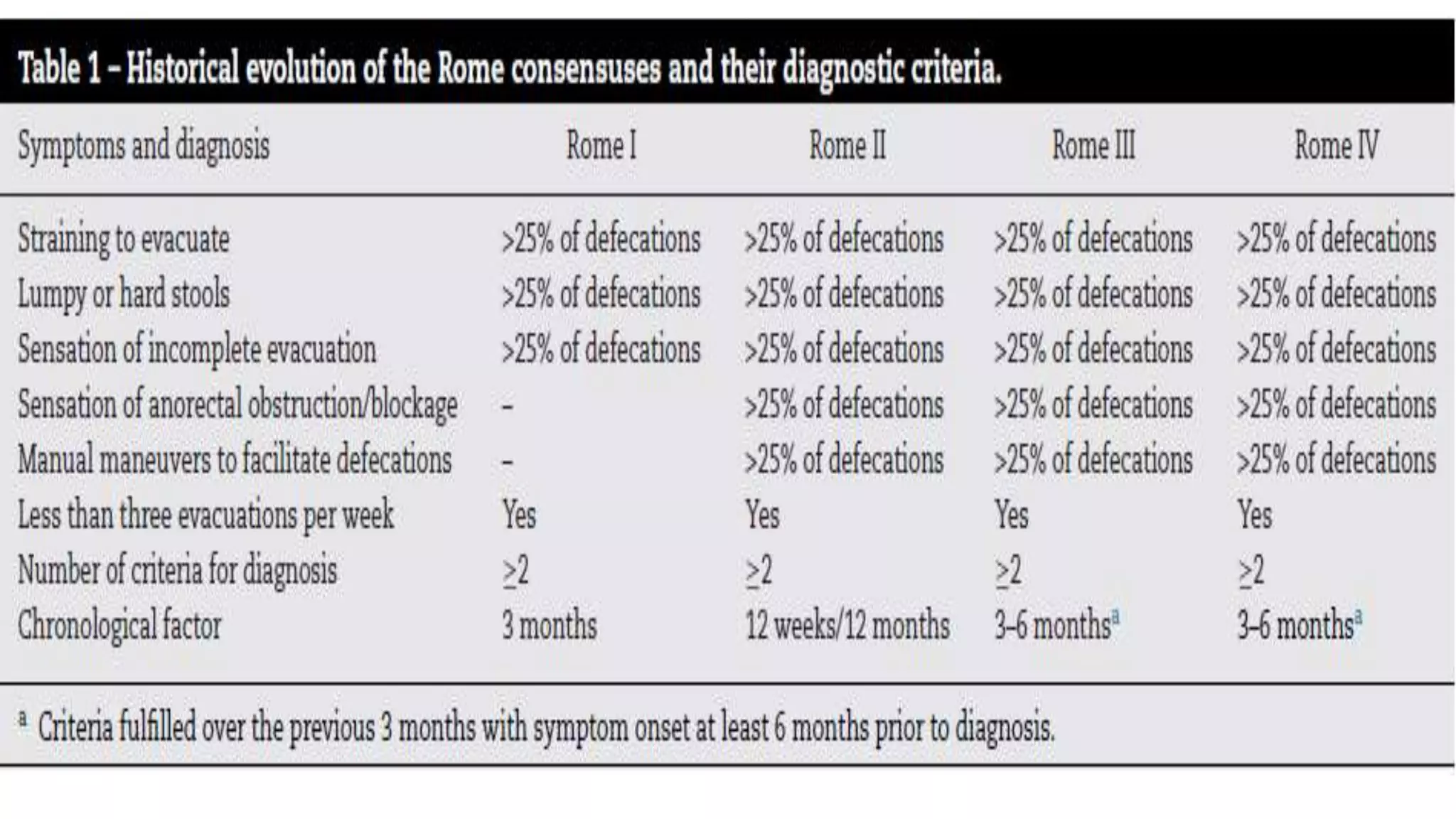
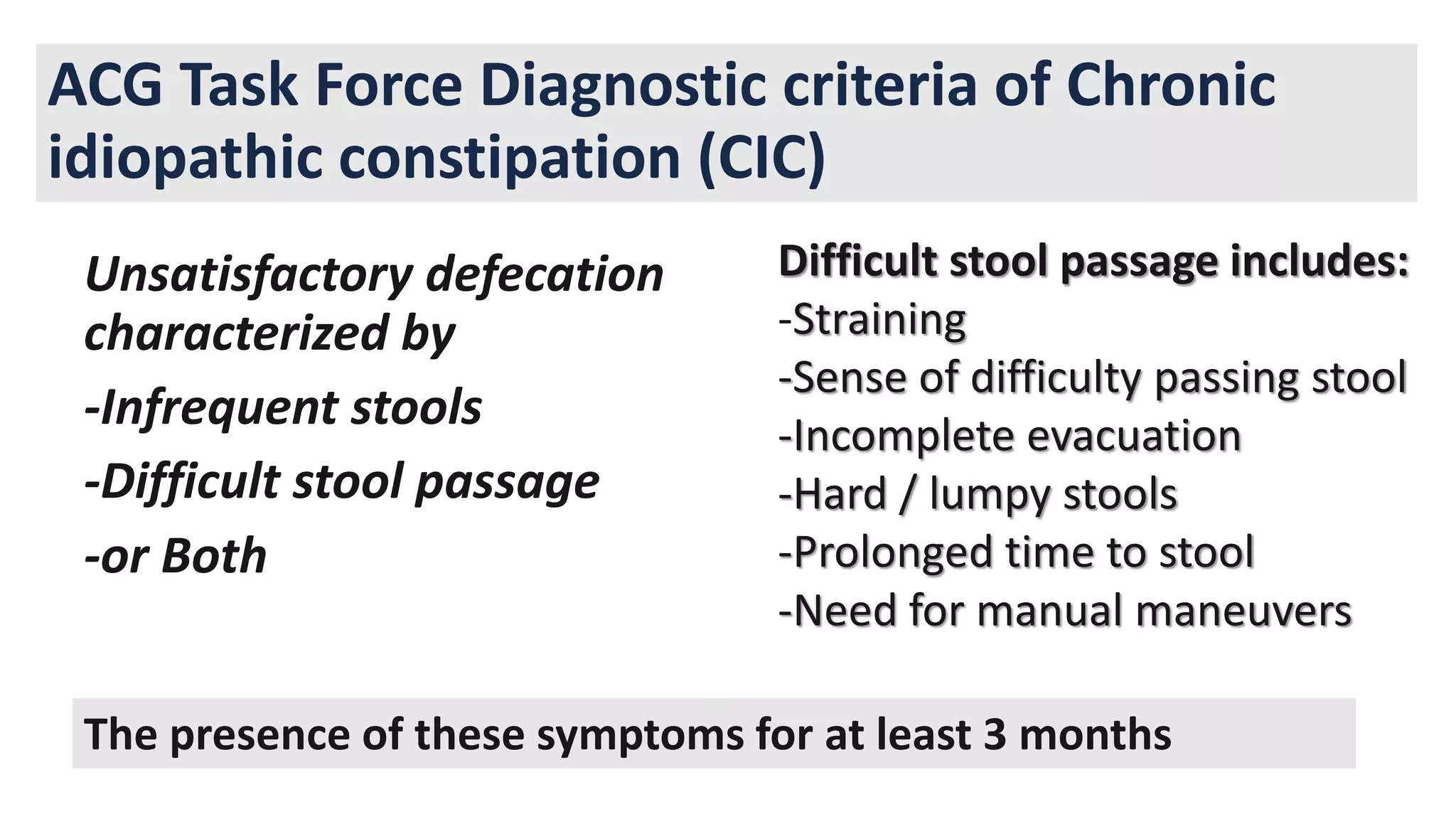
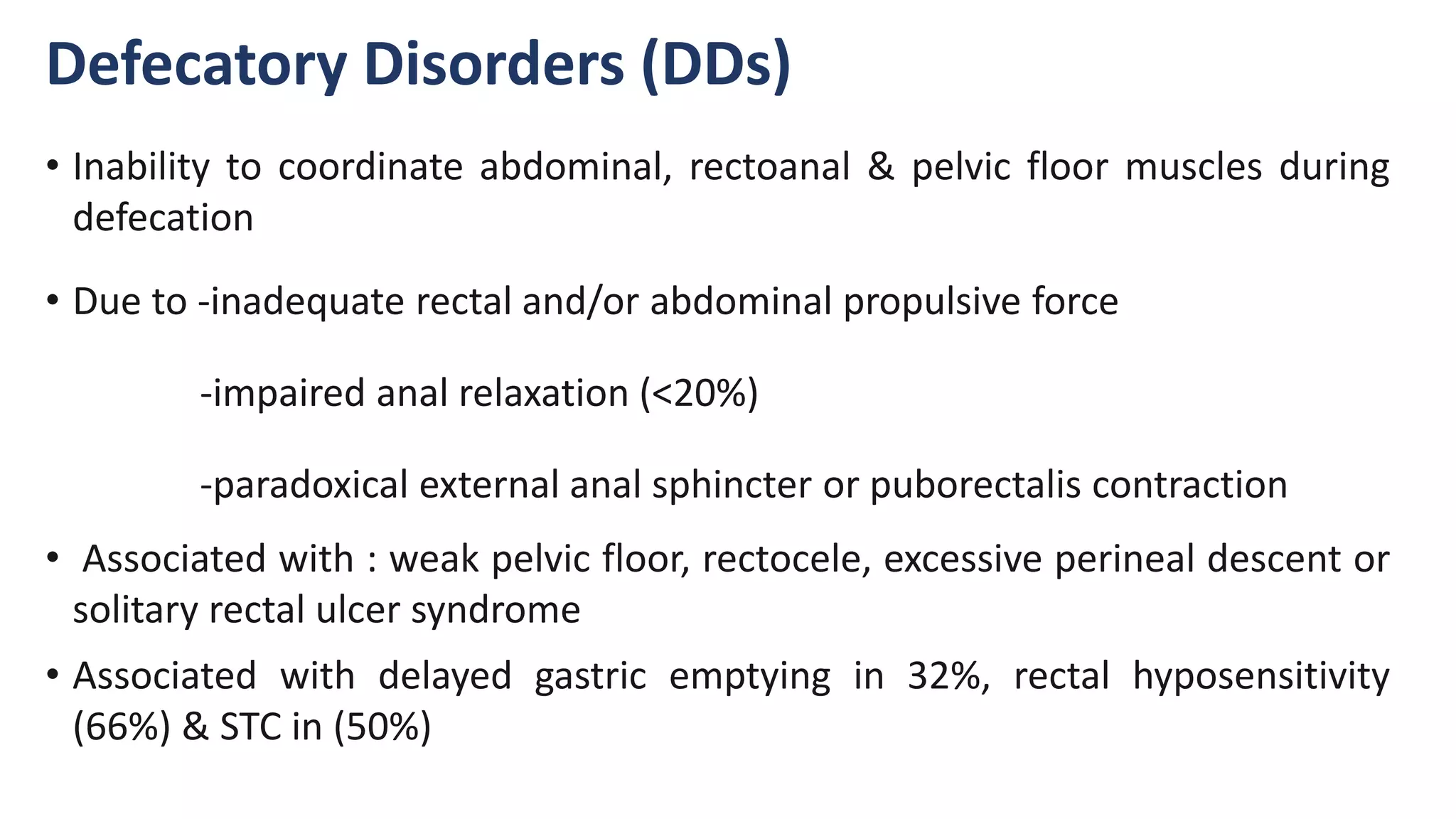
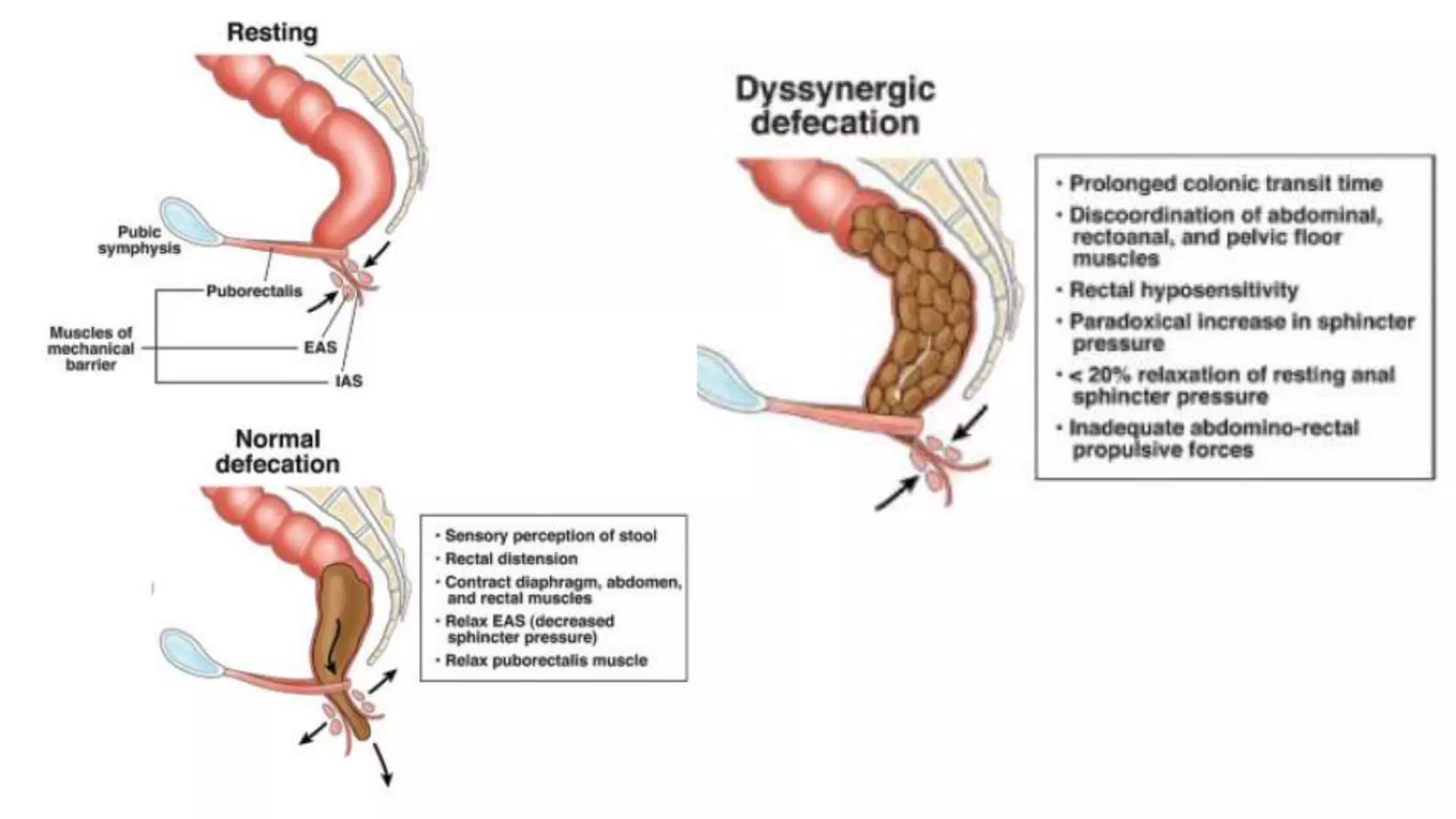
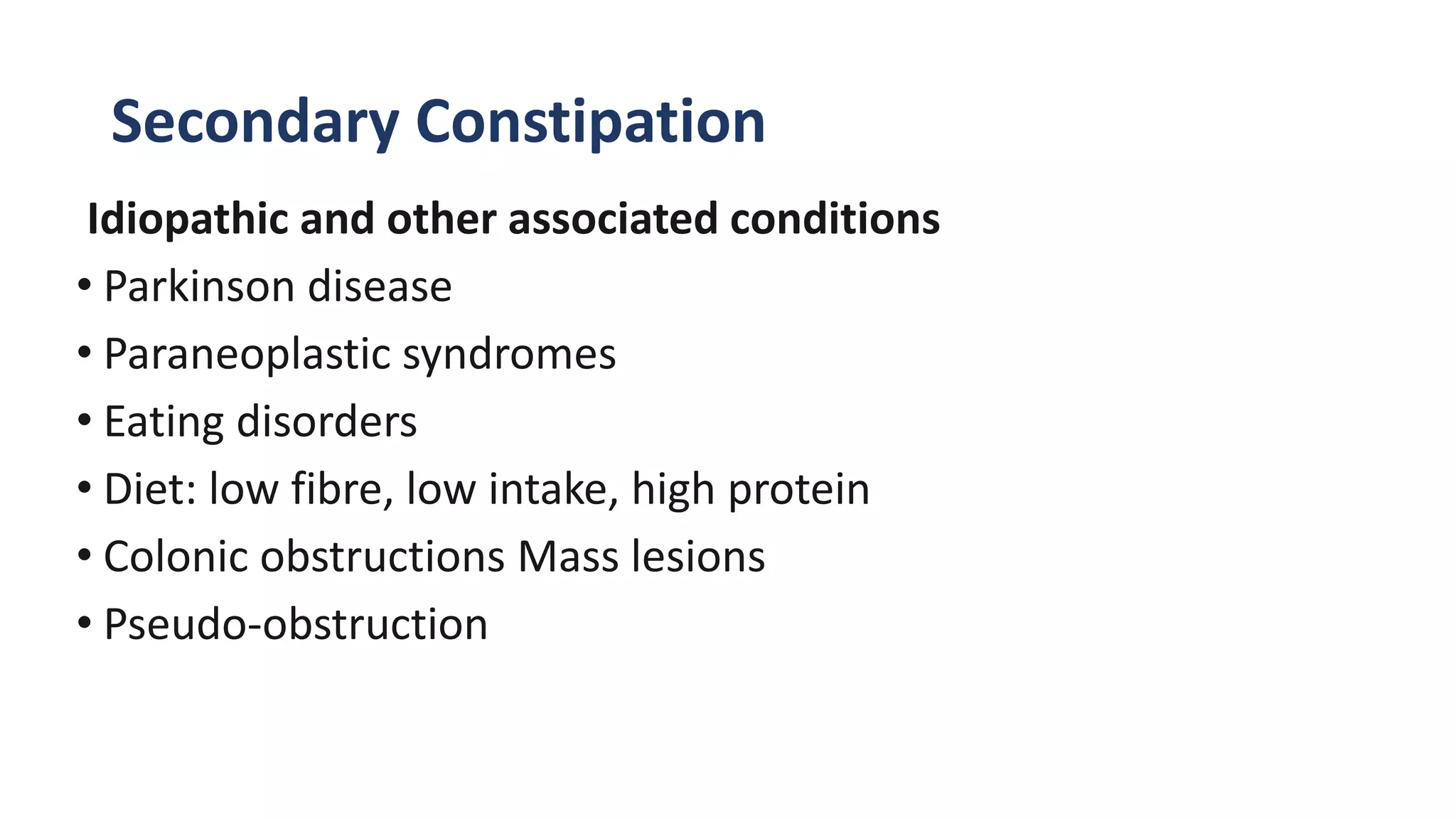
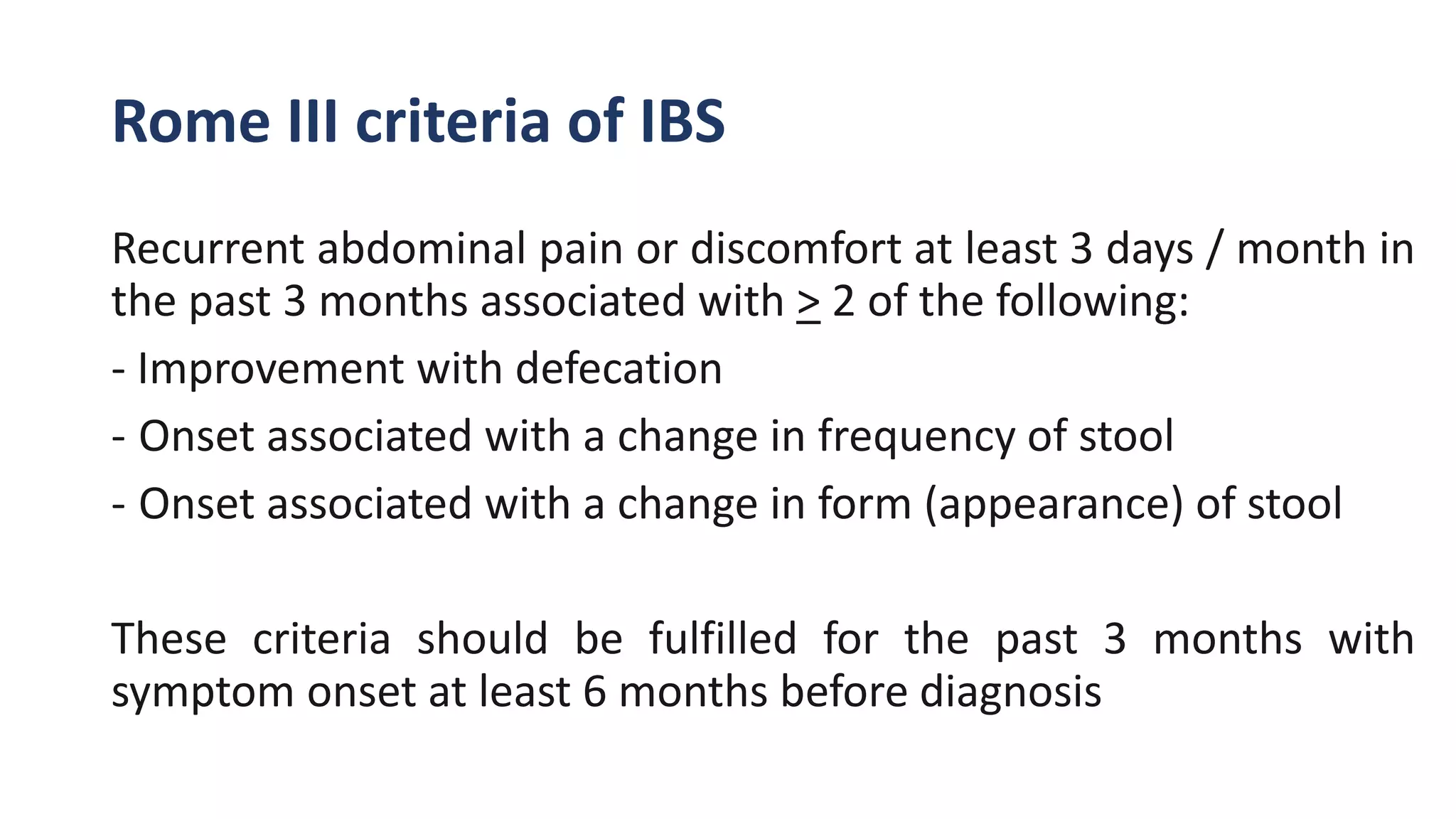
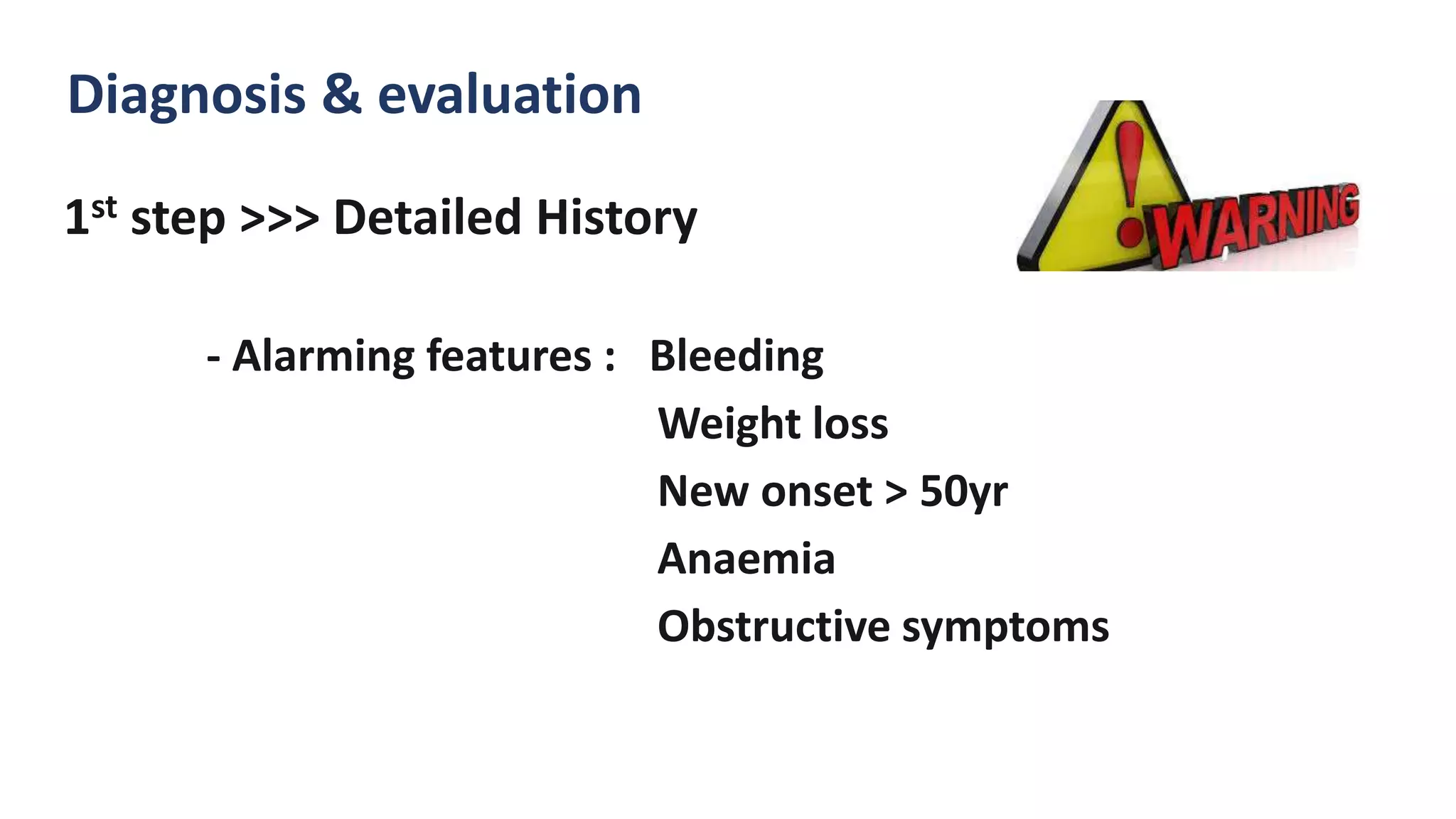
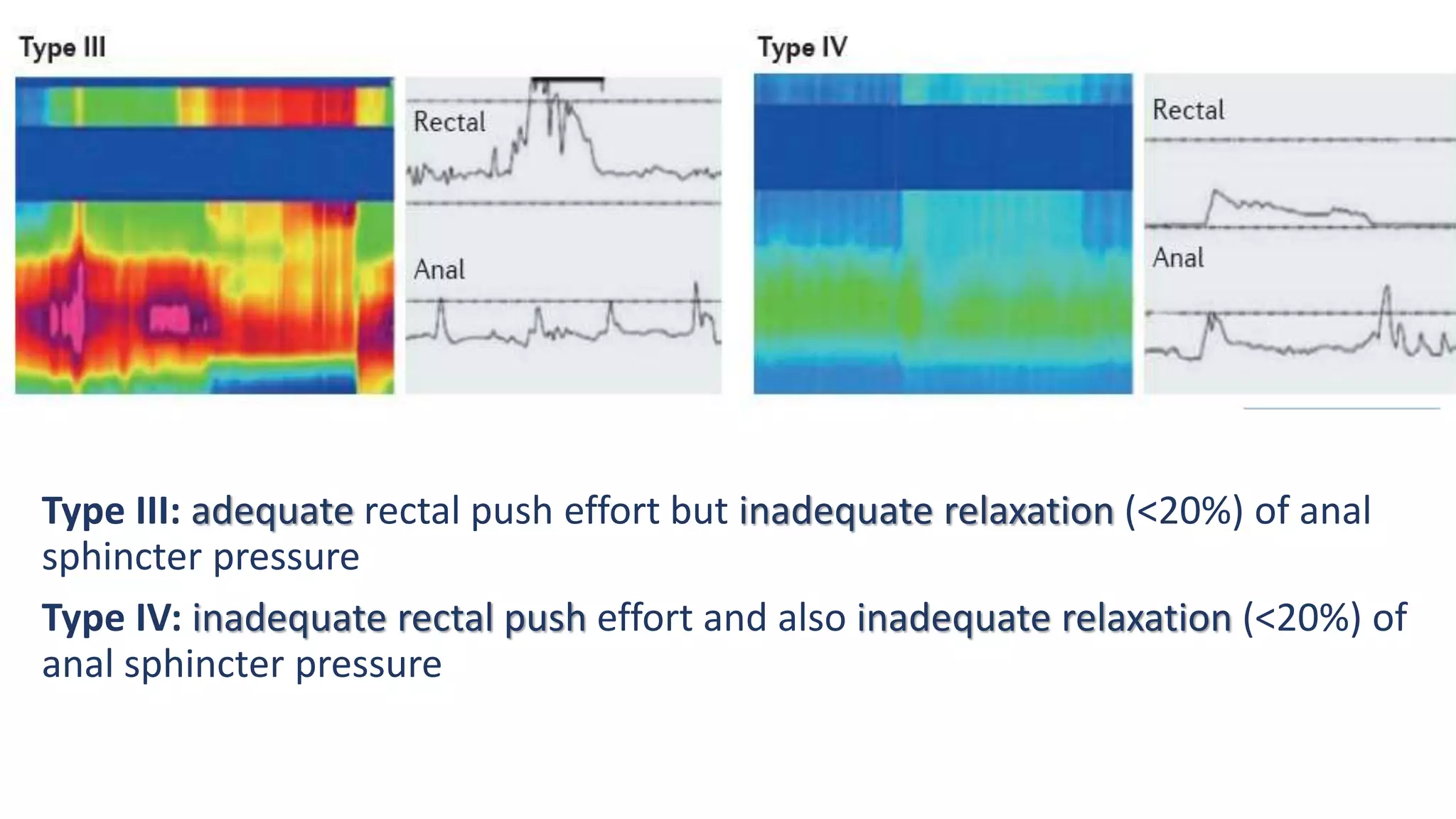
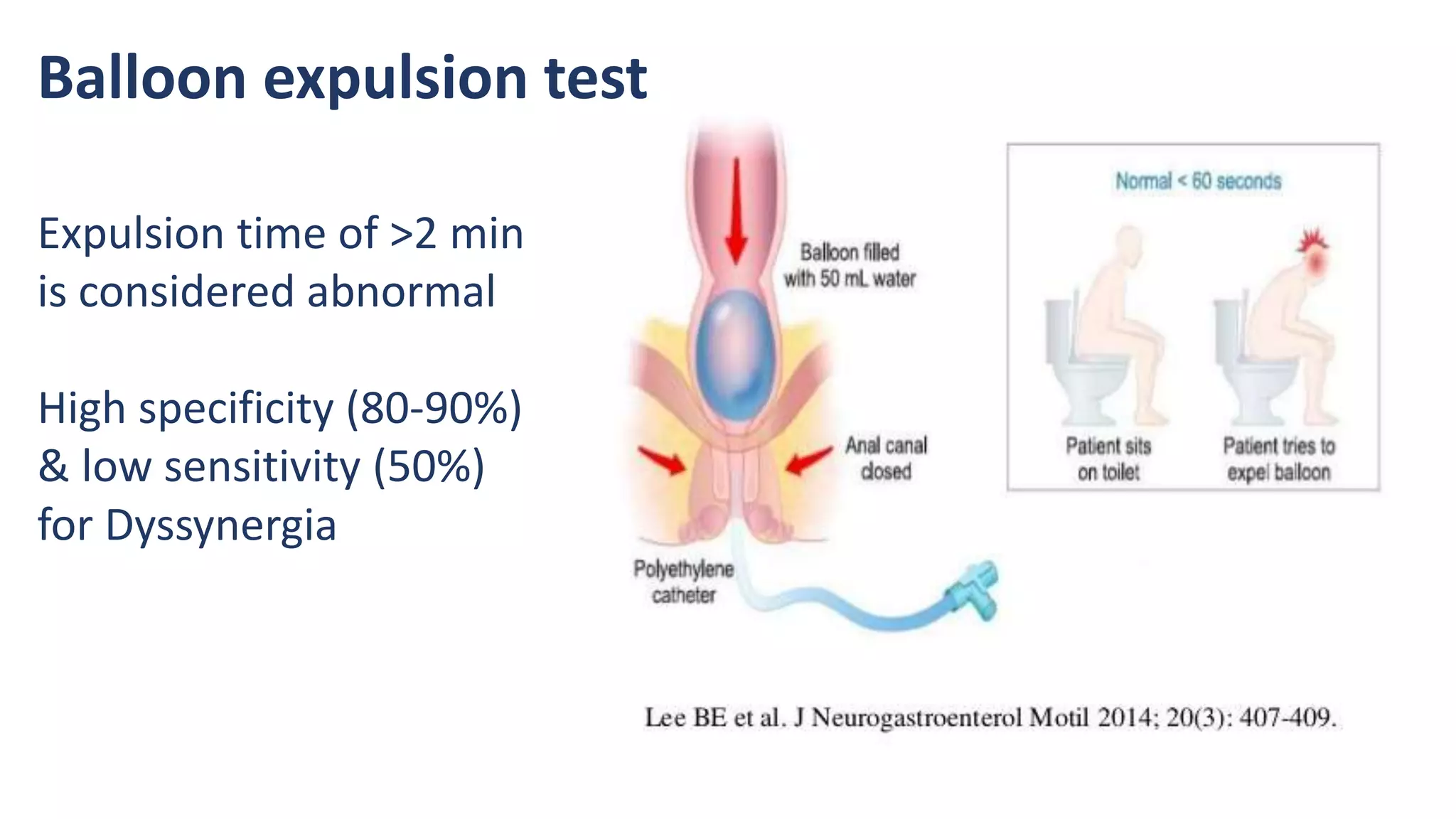
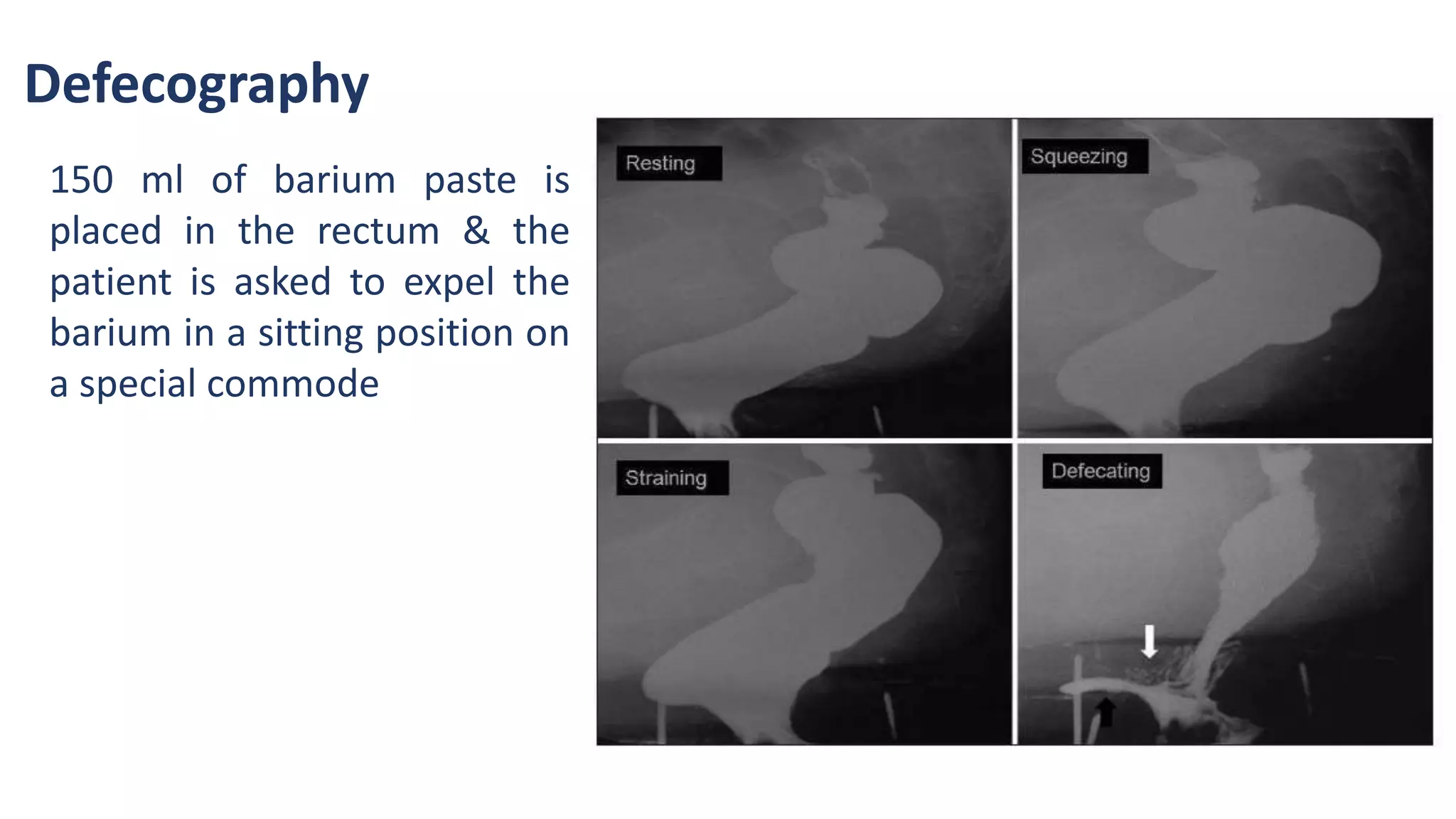
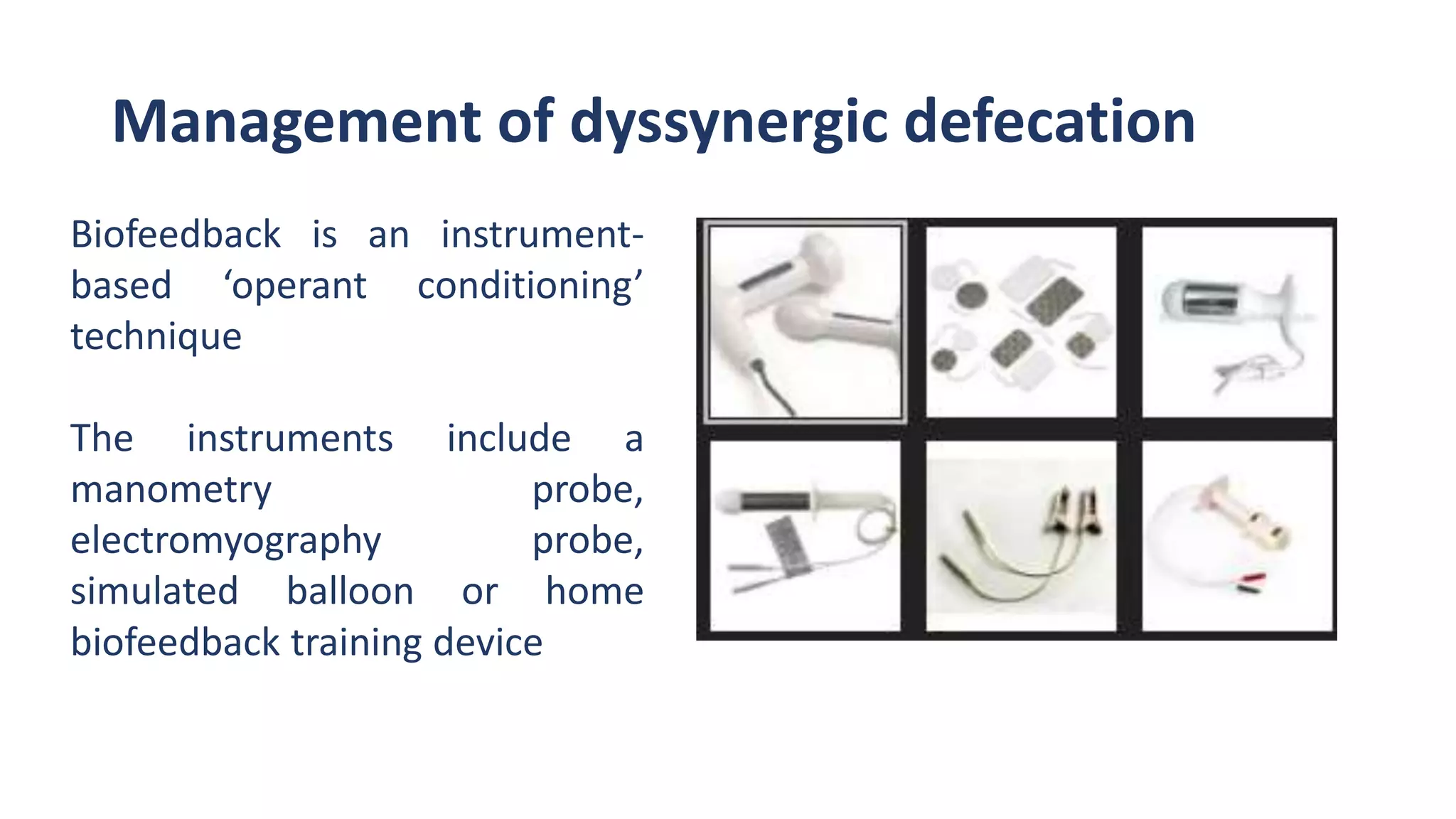
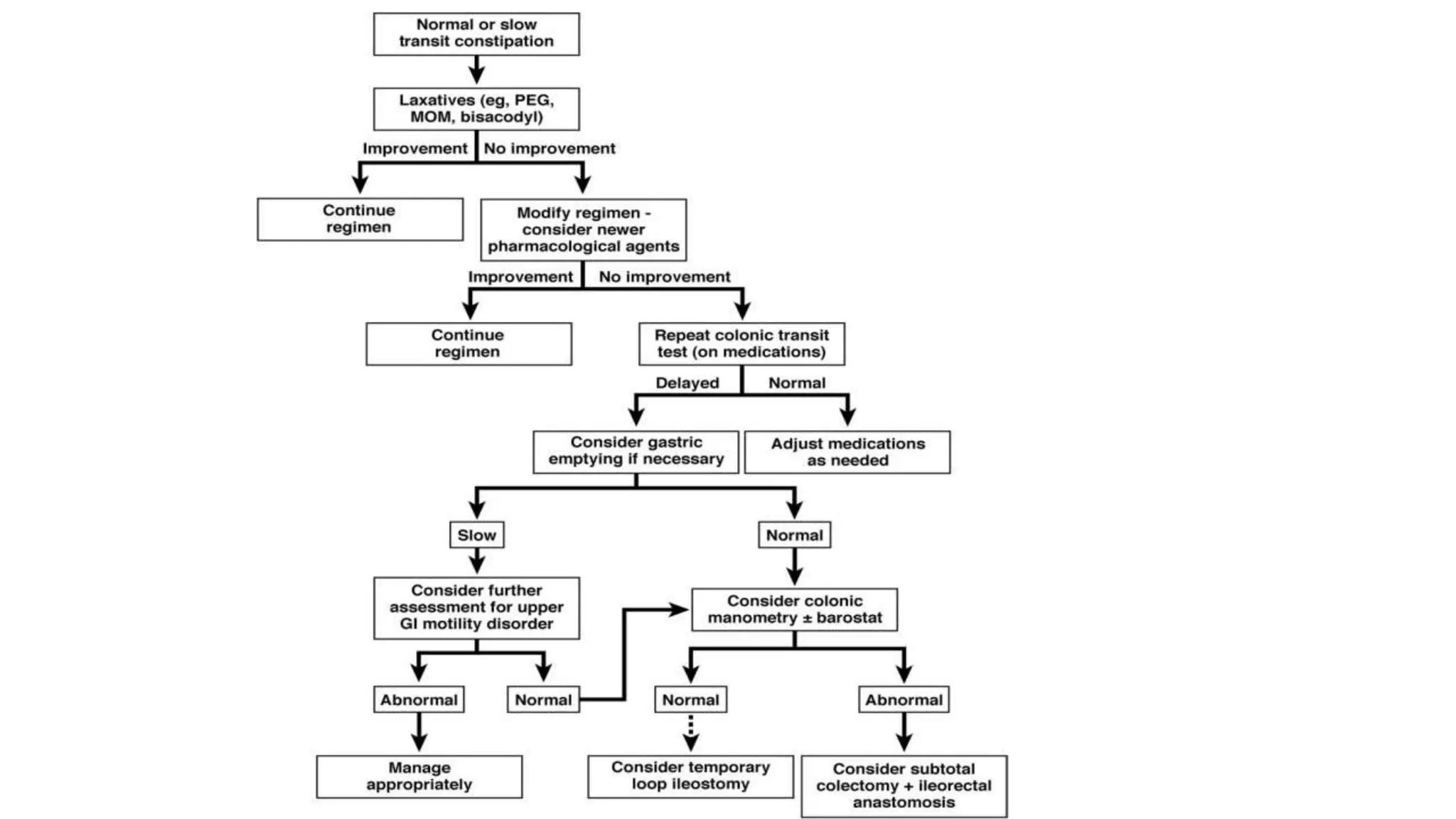
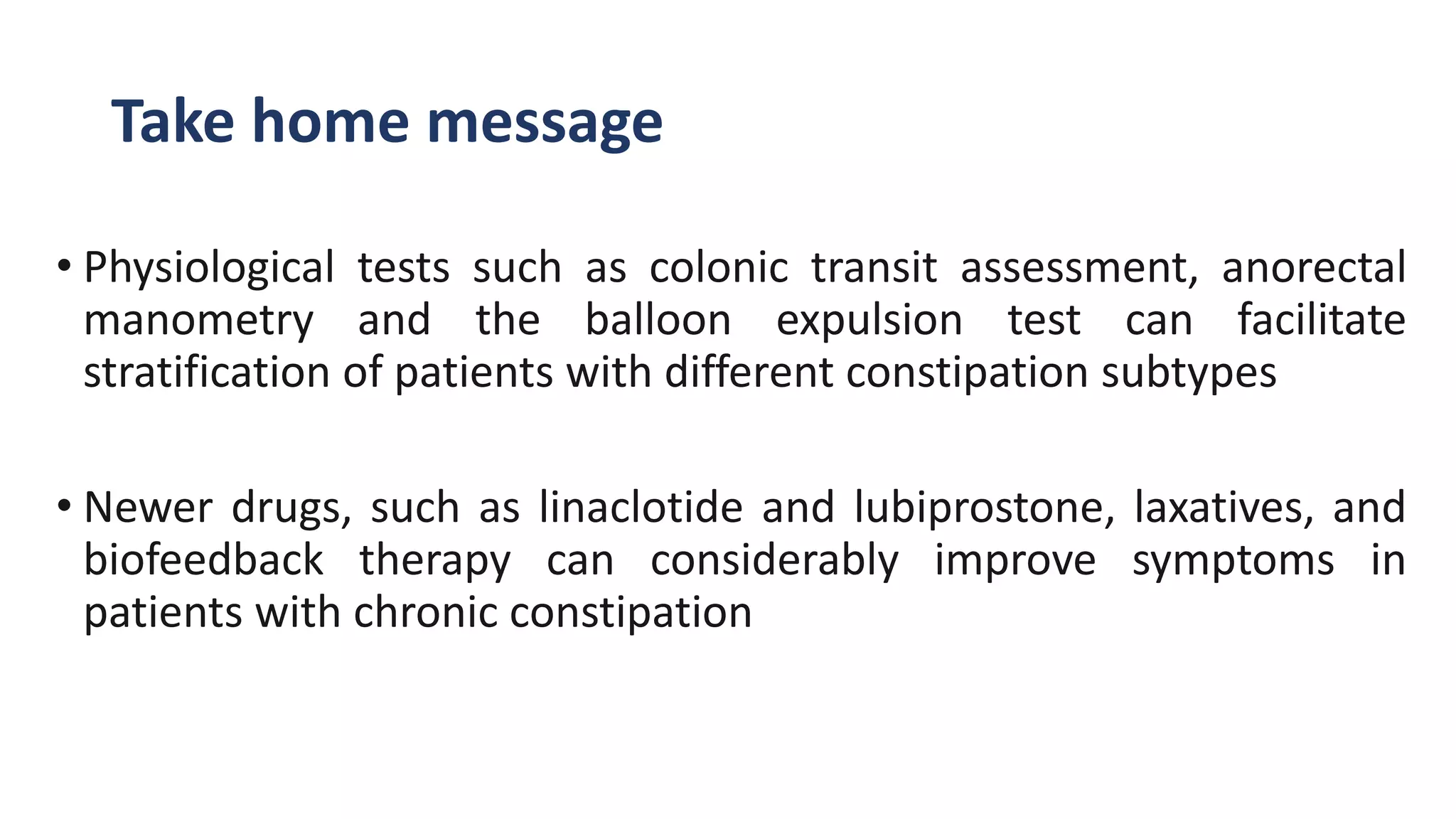
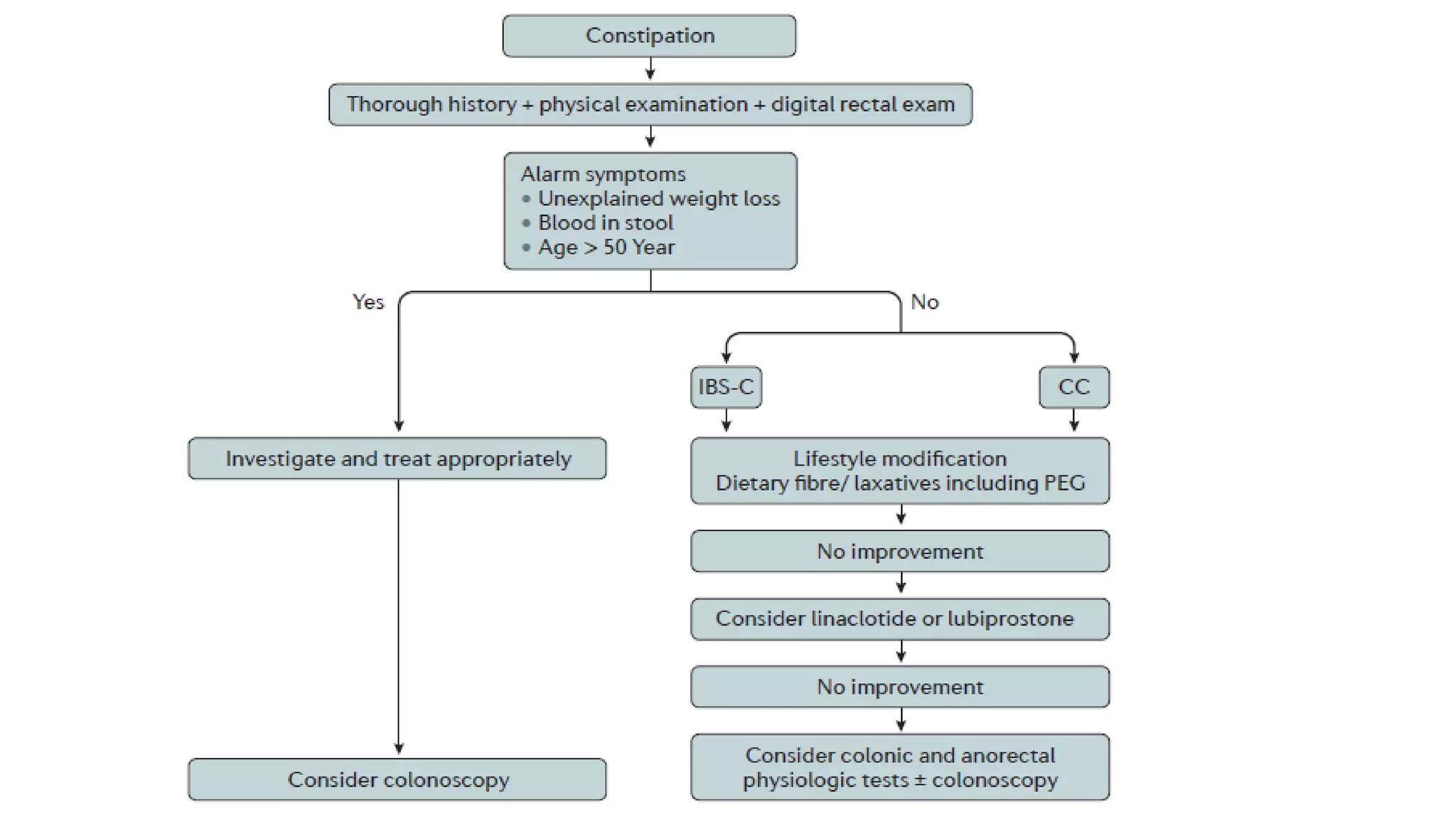
This document discusses constipation, including its definition, diagnostic criteria, types, diagnosis and evaluation, approach, and management. It begins by defining constipation and its most common symptoms. It then discusses the Rome III and ACG diagnostic criteria. It describes the main types of constipation as primary (normal transit, slow transit, defecatory disorders) and secondary. Various diagnostic tests are outlined including colonic transit tests, anorectal manometry, and defecography. The approach prioritizes evaluating for secondary causes and alarming features. The role of endoscopy is to exclude conditions like cancer or Hirschsprung's disease. Management options discussed include lifestyle changes, fiber supplements, laxatives, newer drugs like lub