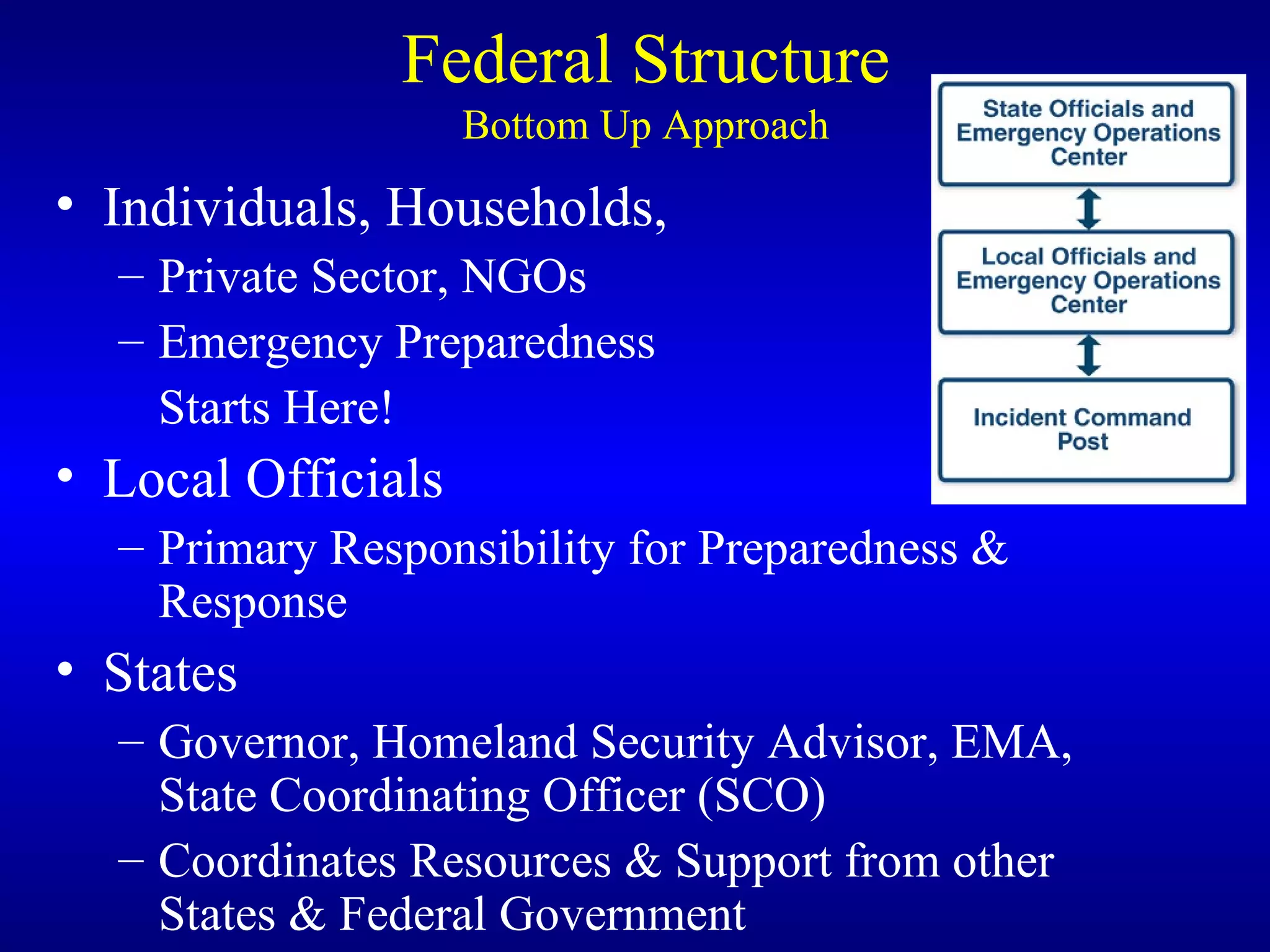
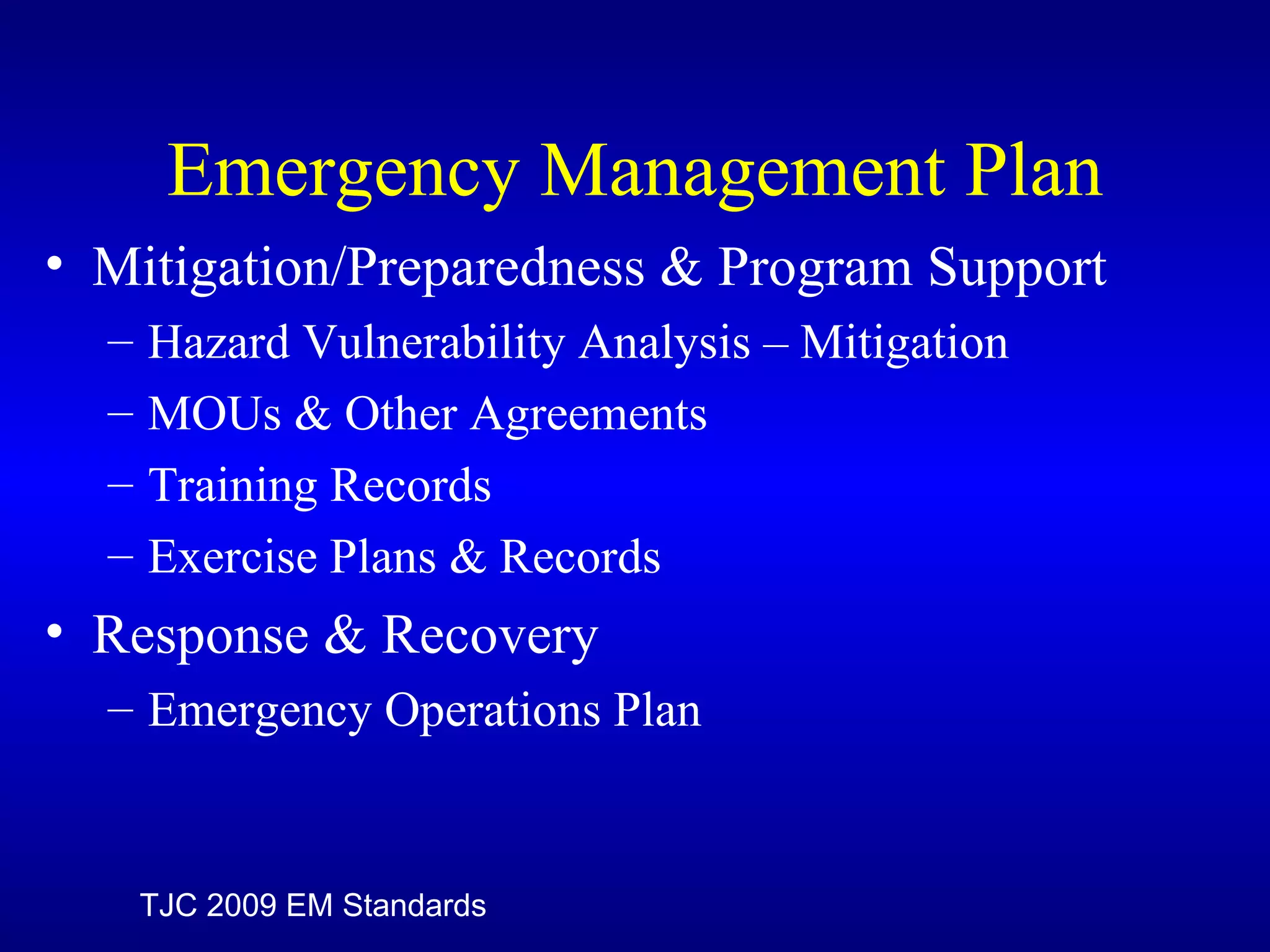
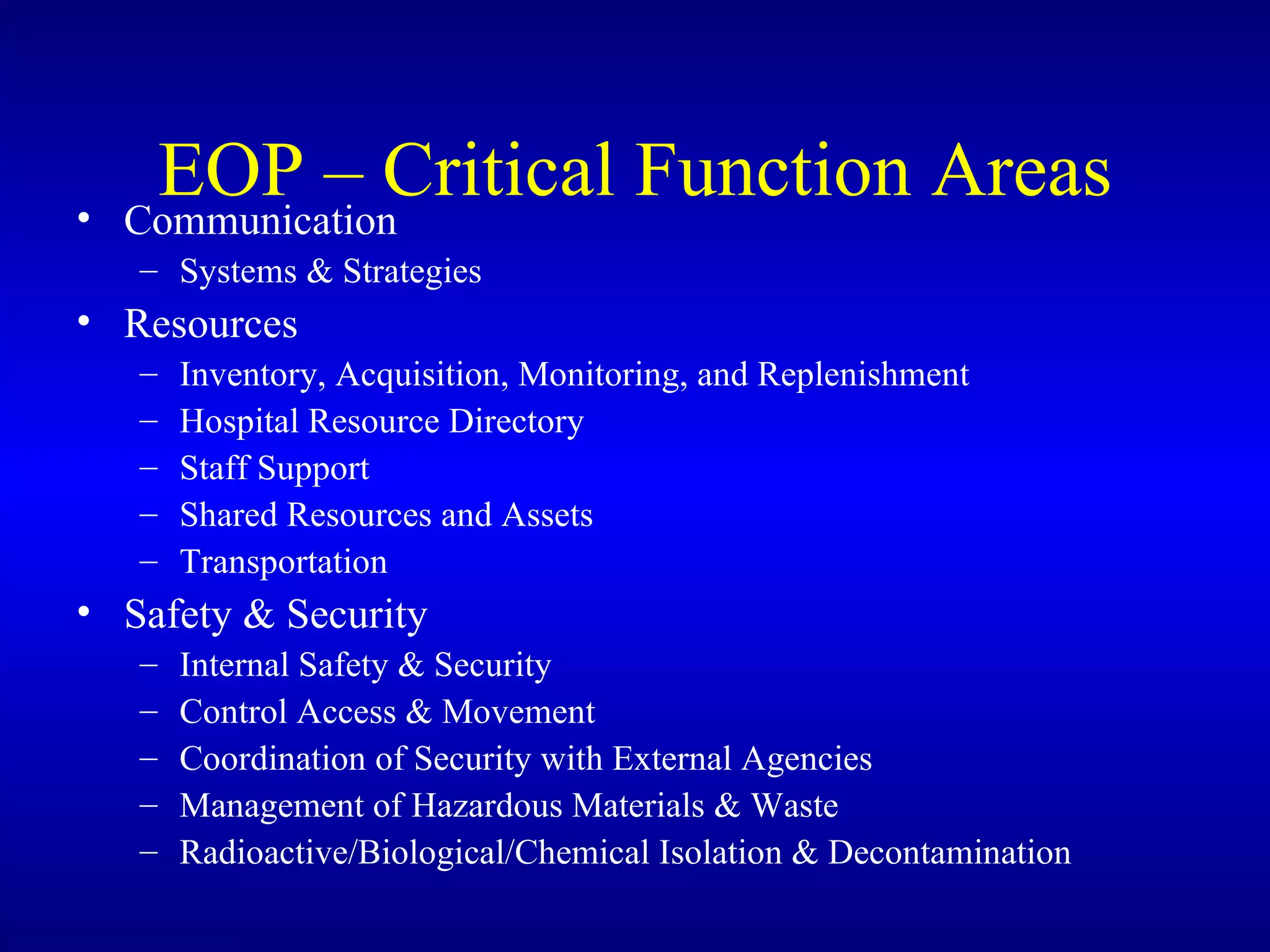
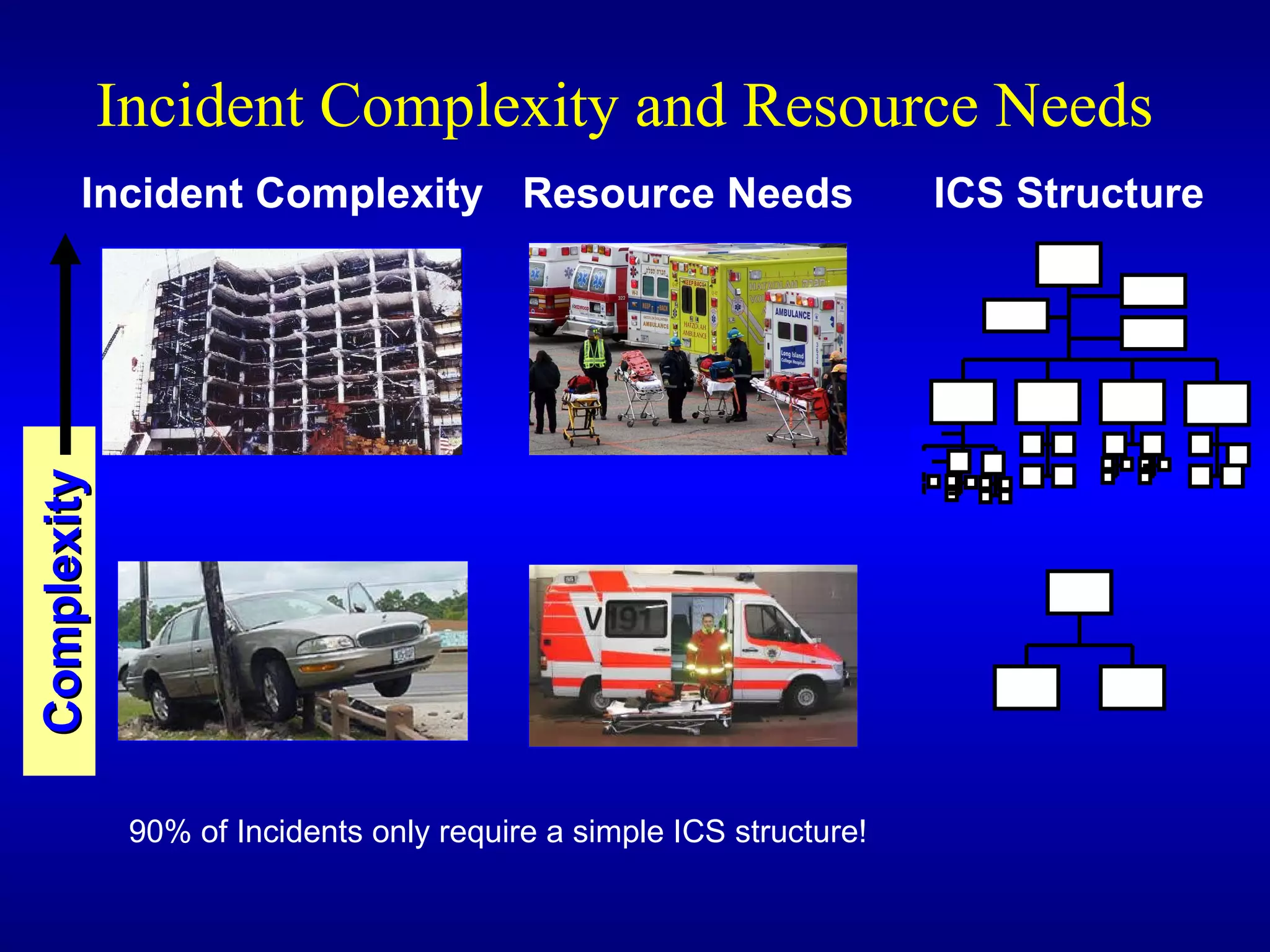
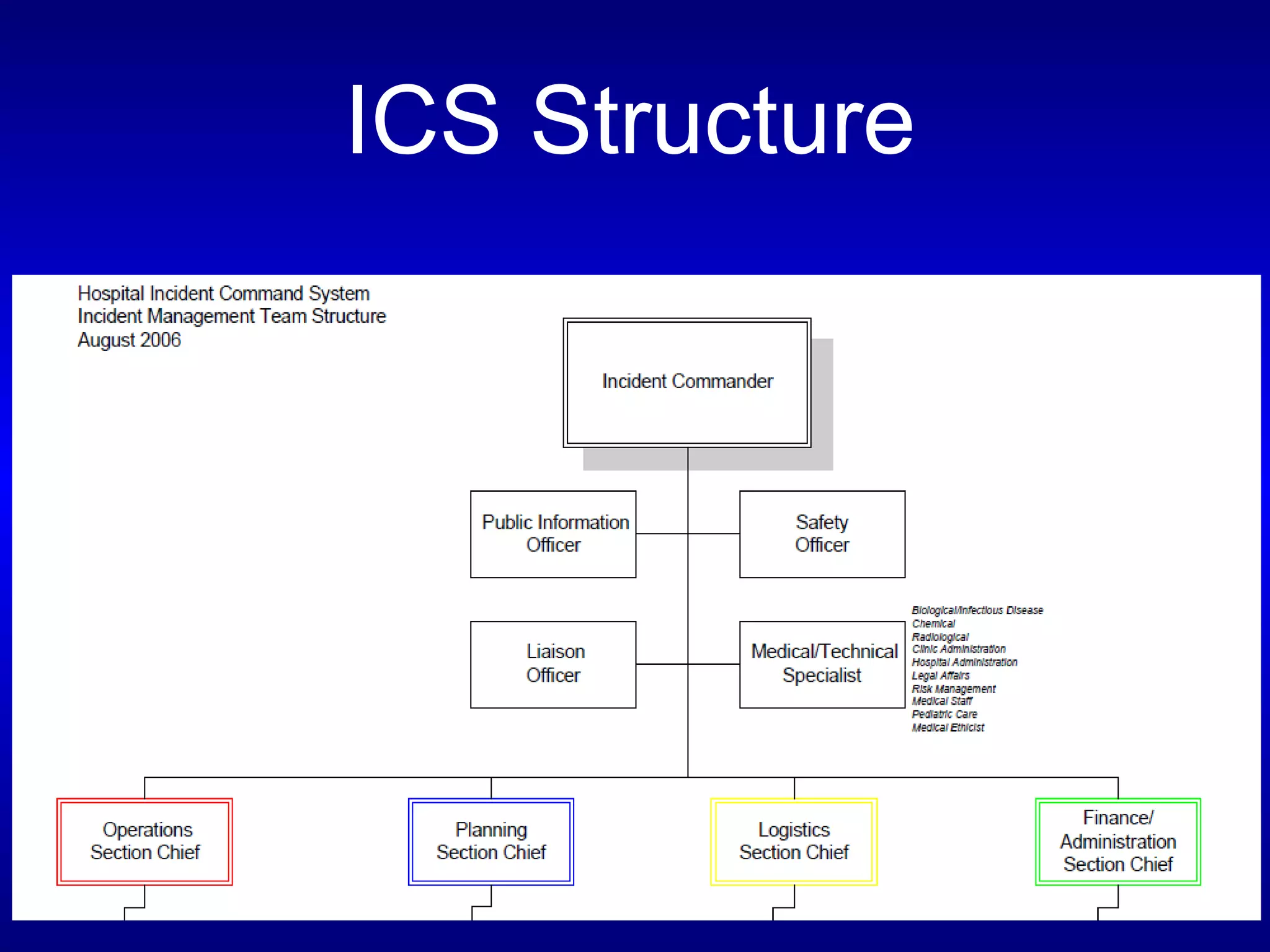
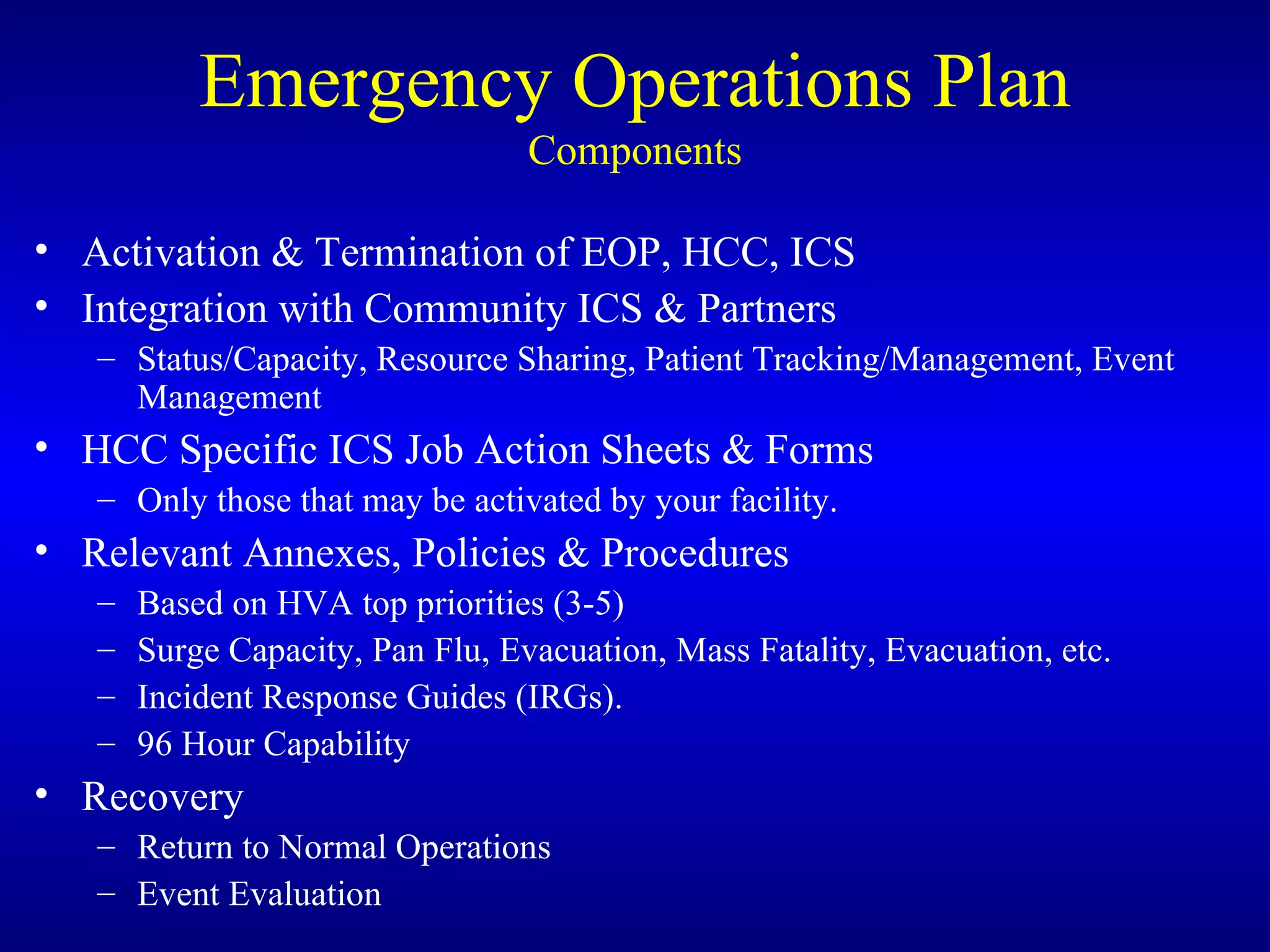
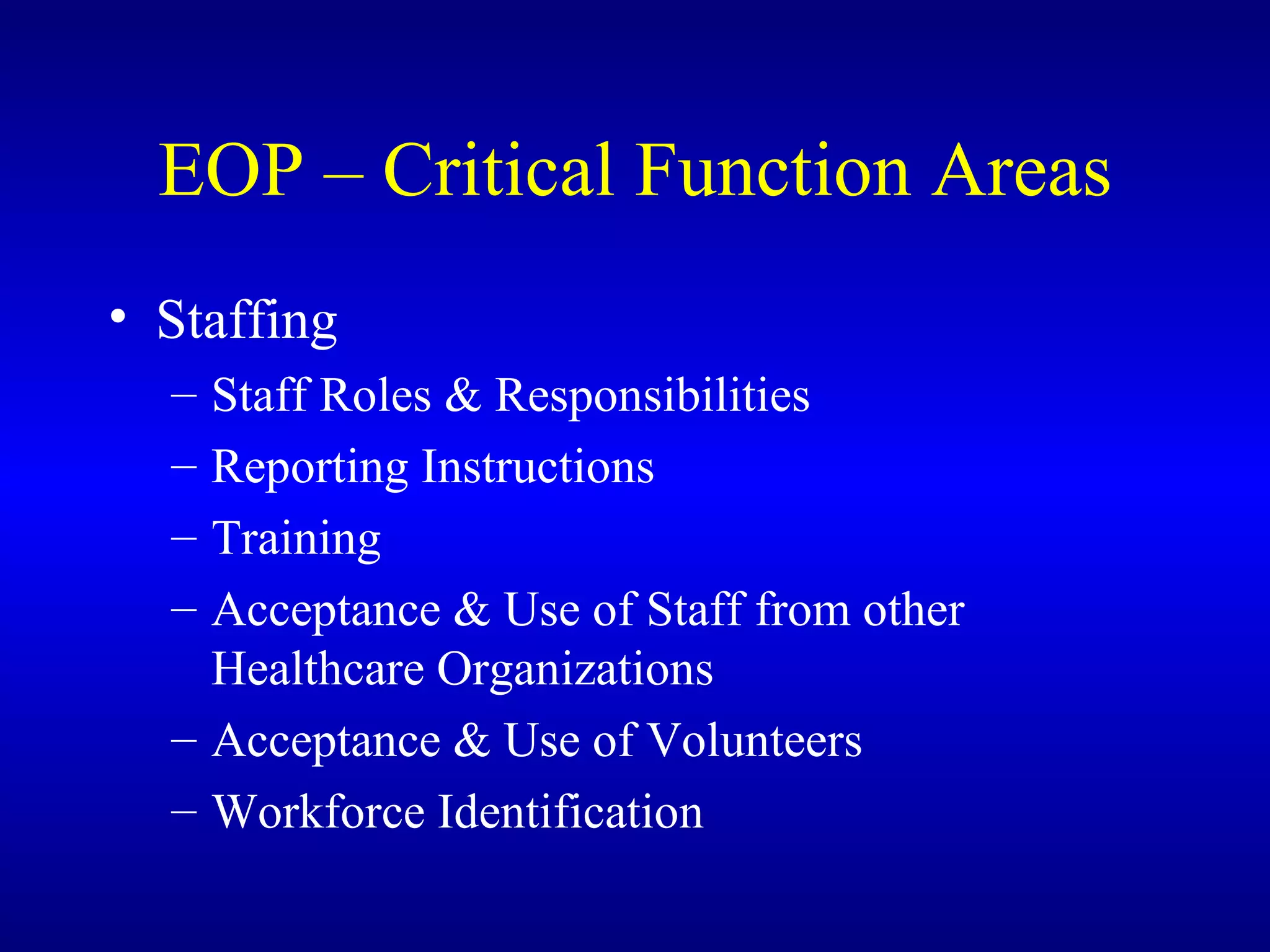
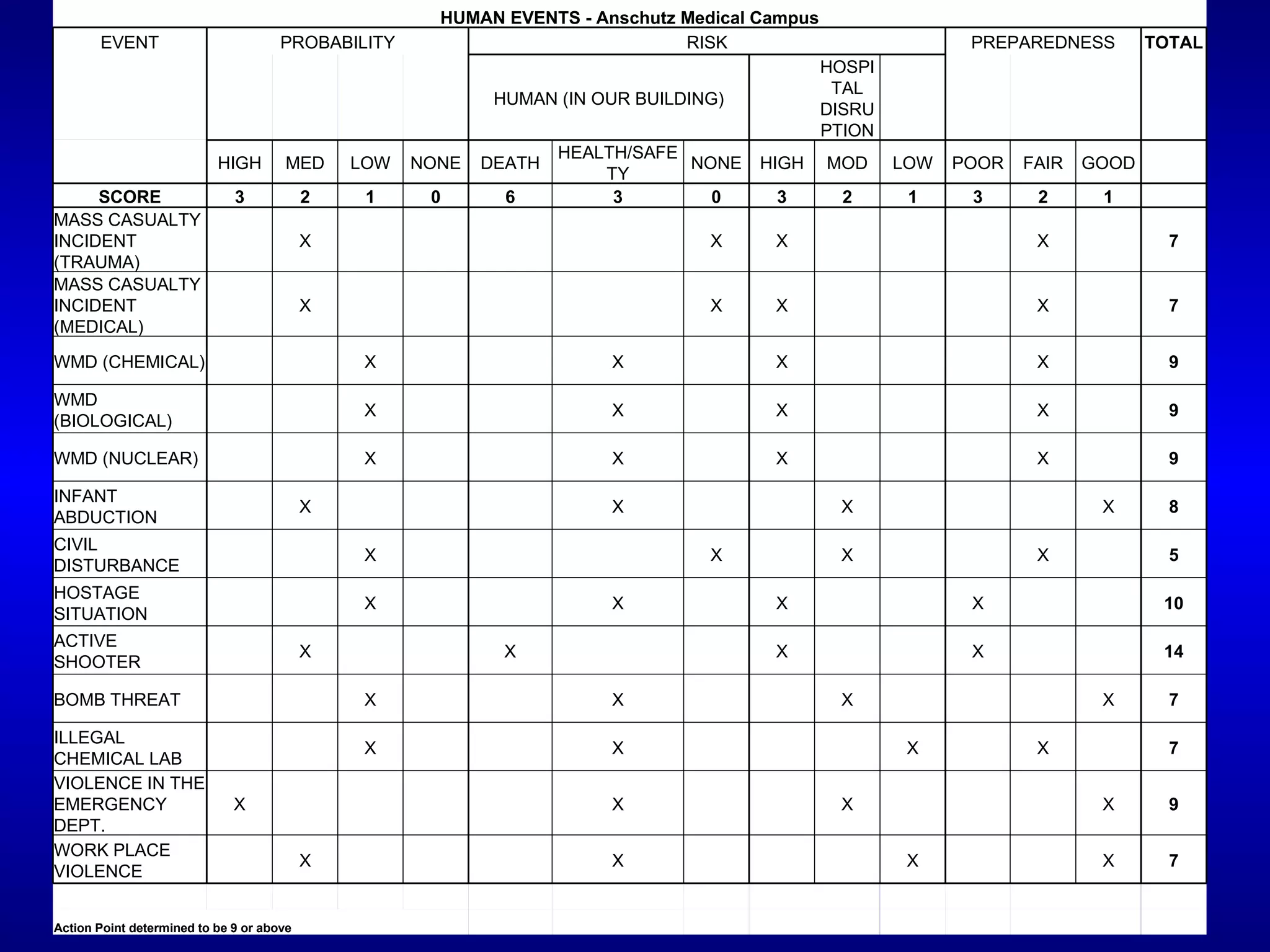
The document outlines the administrative structure and emergency preparedness activities for hospitals responding to disasters. It describes the federal disaster response system and how hospitals fit within the incident command system (ICS). The key points are that hospitals should have an emergency operations plan (EOP) that delineates the six critical function areas of response, as well as annexes for specific hazards. The EOP and training staff in ICS roles are vital for ensuring an effective response.