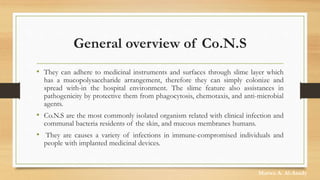
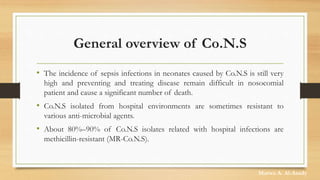
Coagulase-negative staphylococci (co.n.s) are a diverse group of Gram-positive bacteria known for their role as opportunistic pathogens associated with nosocomial and community-acquired infections, particularly in immunocompromised patients and those with implanted medical devices. They exhibit resistance to various antimicrobial agents, with a significant percentage being methicillin-resistant (MR-co.n.s), and their pathogenicity is enhanced by the ability to form biofilms. Co.n.s are implicated in a variety of infections, including skin infections, endocarditis, and bloodstream infections, making their prevention and control critical in healthcare settings.