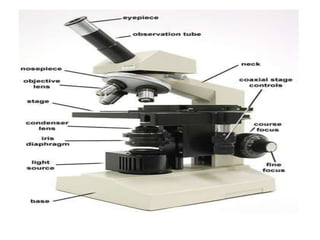
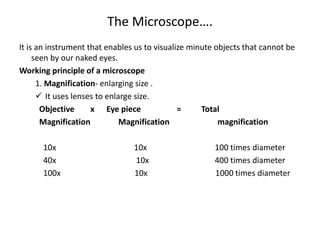
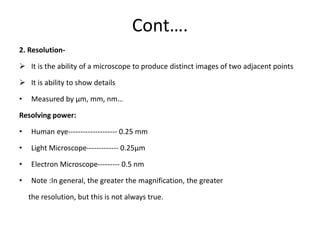
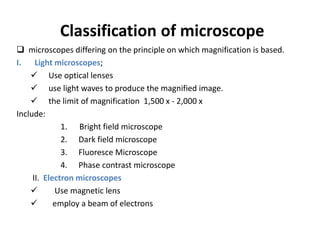
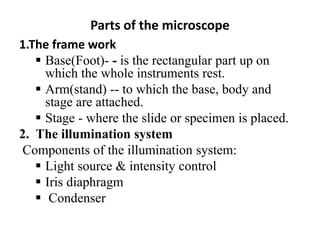
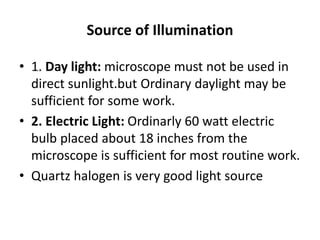
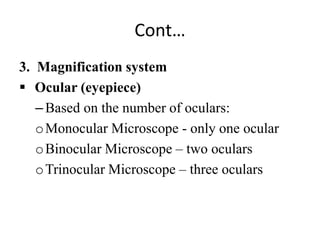
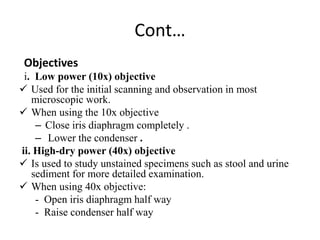
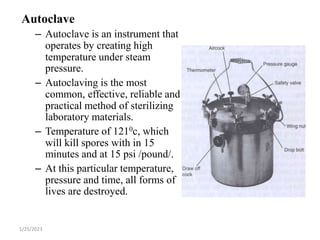
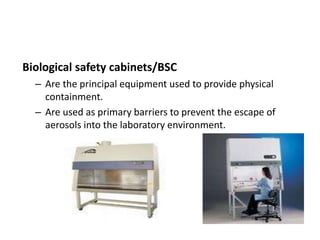
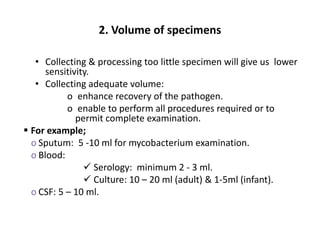
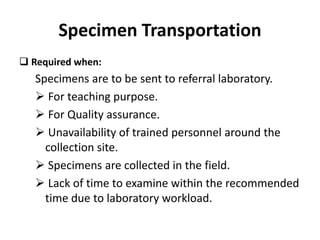
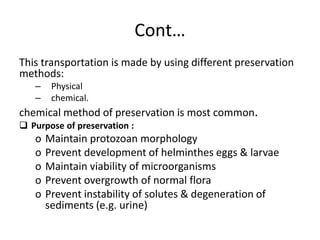
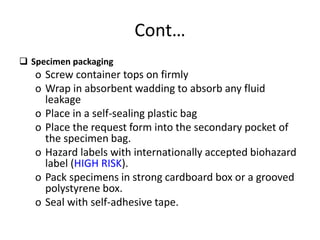
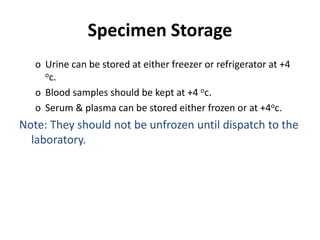
This document describes various basic laboratory equipment and their uses. It discusses the microscope in detail, including its parts, principles of magnification and resolution, and types. It also describes other common equipment like the centrifuge, glassware, incubator, autoclave, ovens, water bath, and biosafety cabinet. Finally, it covers specimen collection, transportation, storage, and rejection criteria.