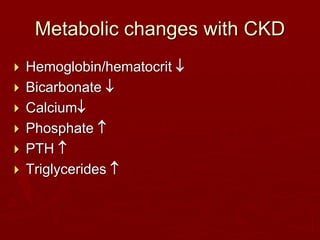
This document describes a case of chronic kidney disease in a 21-year old man. Over 5 years, his serum creatinine level gradually increased from 0.5 mg/dL to 1.81 mg/dL, indicating progressive loss of kidney function. He was treated with steroids and immunosuppressants but continued to experience relapses of nephrotic syndrome. On his latest examination, lab tests showed further kidney dysfunction with a serum creatinine of 1.29 mg/dL. Despite refusing dialysis, he died shortly after from complications of his kidney disease. The document outlines factors related to managing chronic kidney disease, including monitoring for anemia, acidosis, mineral abnormalities, and nutrition.