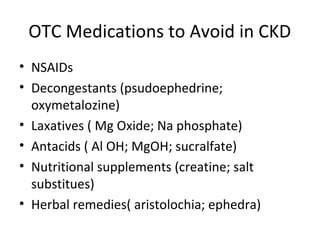
This document discusses the screening, management, and treatment of chronic kidney disease. It notes that chronic kidney disease affects over 10% of US adults and risk increases with age. Diabetes and hypertension are the most common causes of end-stage renal disease. It recommends referring patients with decreased eGFR and increased albuminuria to a nephrologist. The management of complications such as hypertension, dyslipidemia, anemia, acidosis, and bone mineral disorders is also covered.