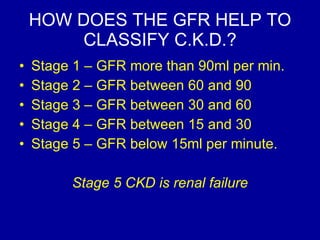
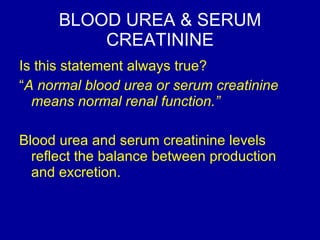
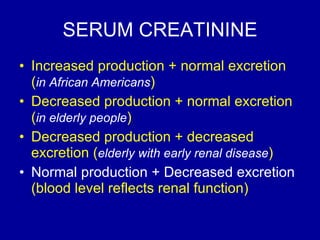
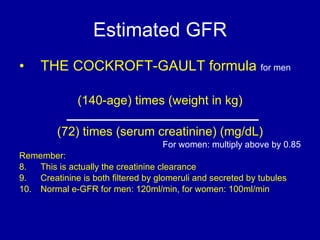
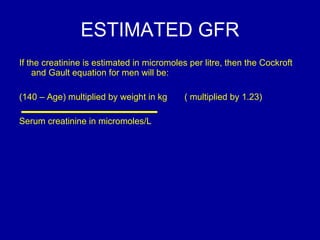
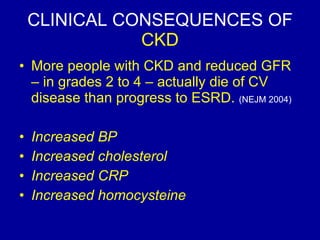
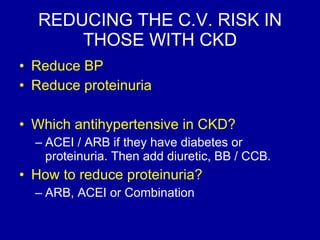
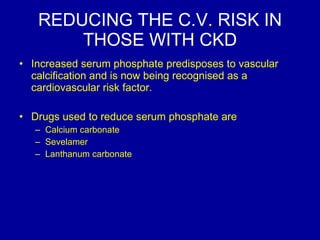
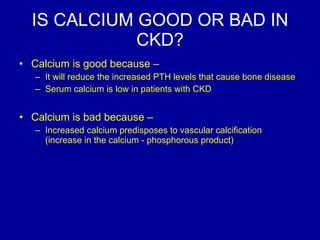
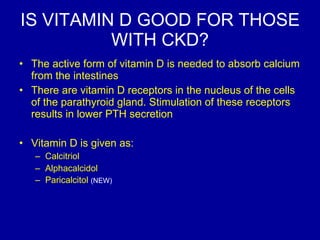
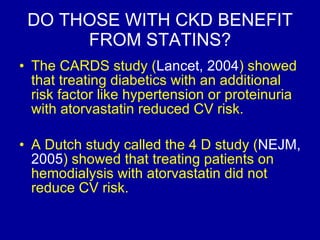
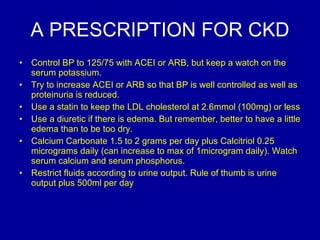
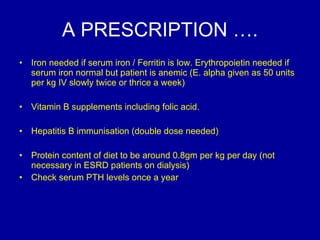
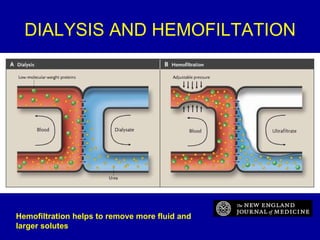
This document summarizes key topics about chronic kidney disease (CKD), including definitions, classification stages based on glomerular filtration rate (GFR), clinical consequences such as increased cardiovascular risk, and treatment goals like blood pressure and proteinuria control. It discusses markers of renal function like serum creatinine and estimated GFR, as well as complications of CKD like anemia and how they are treated. Target hemoglobin levels with erythropoietin therapy and outcomes of hemodialysis are also summarized.