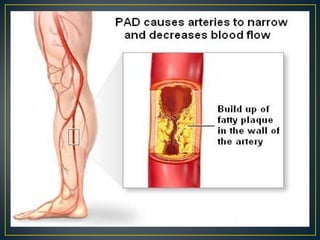
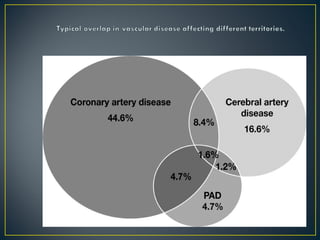
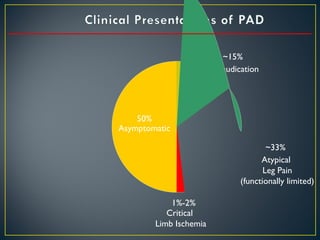
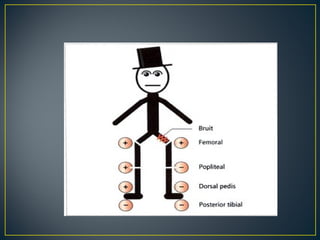
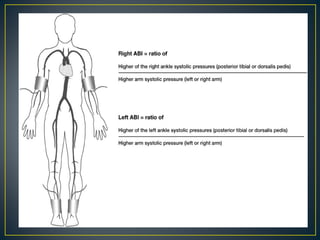
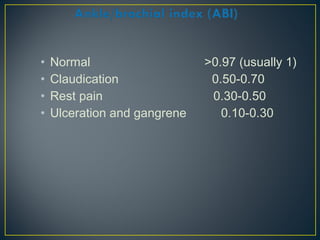
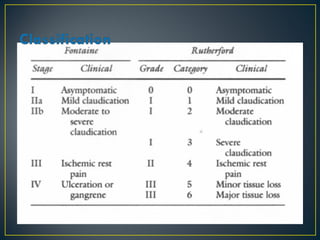
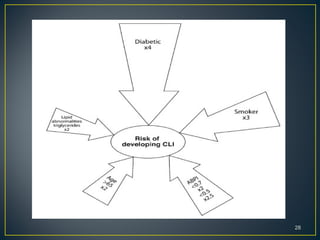
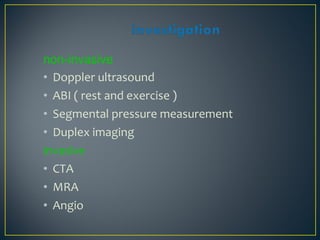
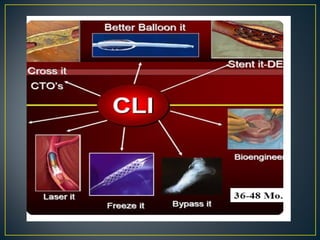
The document discusses peripheral artery disease (PAD), specifically critical limb ischemia (CLI). It defines CLI as a severe form of PAD involving ischemic rest pain, ulcers, or gangrene lasting over 2 weeks due to reduced blood flow. CLI is diagnosed using ankle-brachial pressure index testing or angiography and treated through risk factor modification, pharmacotherapy, and revascularization to relieve pain, heal ulcers, and prevent limb loss. The primary goals of CLI treatment are to improve symptoms, function, and survival.