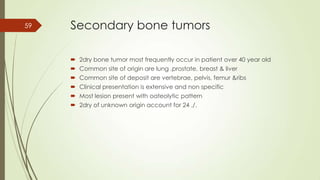
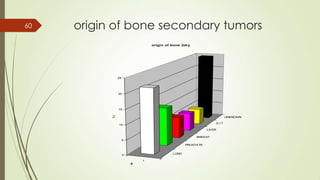
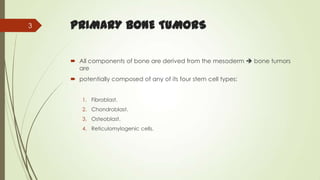
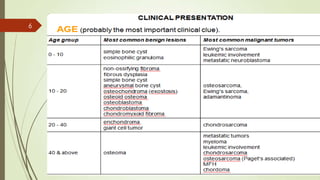
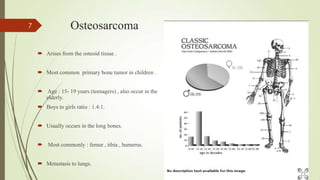
Primary bone tumors can arise from bone or cartilage cells and are either benign or malignant. The most common primary malignant bone tumors are osteosarcoma, chondrosarcoma, Ewing's sarcoma, and fibrosarcoma. Osteosarcoma typically affects teenagers and presents as pain in the long bones. Chondrosarcoma is usually slow growing and affects older adults, most commonly in the pelvis or shoulder. Ewing's sarcoma affects bone or soft tissue in teenagers and young adults. Fibrosarcoma can occur as a soft tissue or bone tumor, usually in the femur or tibia. Secondary bone tumors most commonly spread from the lung, prostate, breast, or liver and deposit in








![Chondrosarcoma Grades
Grade I (low grade) – Cytologically similar to enchondroma[2] ; cellularity is
higher, with occasional plump nuclei with open chromatin structure
Grade II (intermediate grade) – Characterized by a definite and increased
cellularity; distinct nucleoli are present in most cells, and foci of myxoid
change may be seen
Grade III (high grade) – Characterized by high cellularity, prominent
nuclear atypia, and the presence of mitosis
21](https://image.slidesharecdn.com/bonetumors-140324143116-phpapp01/85/Bone-tumors-21-320.jpg)