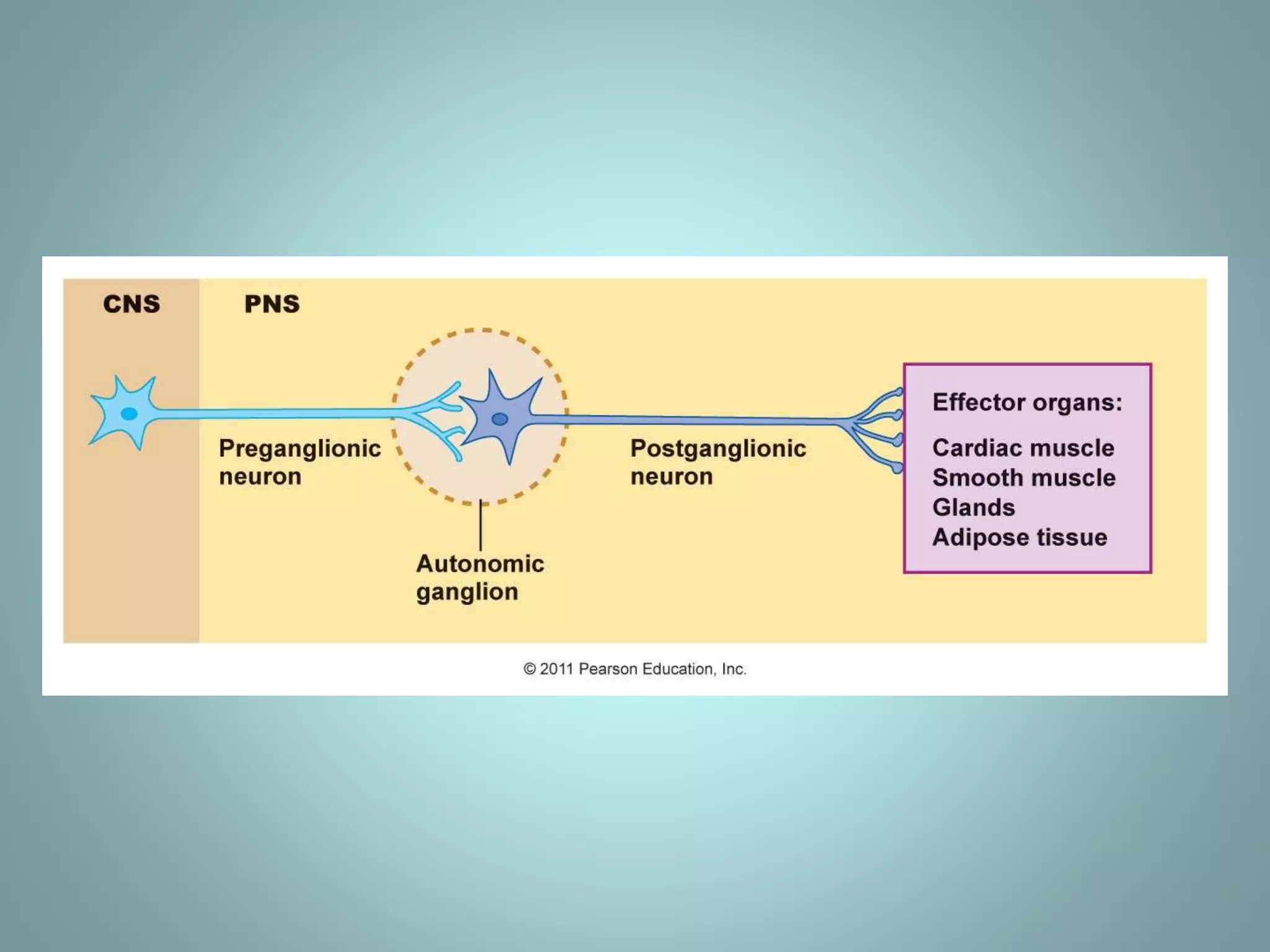
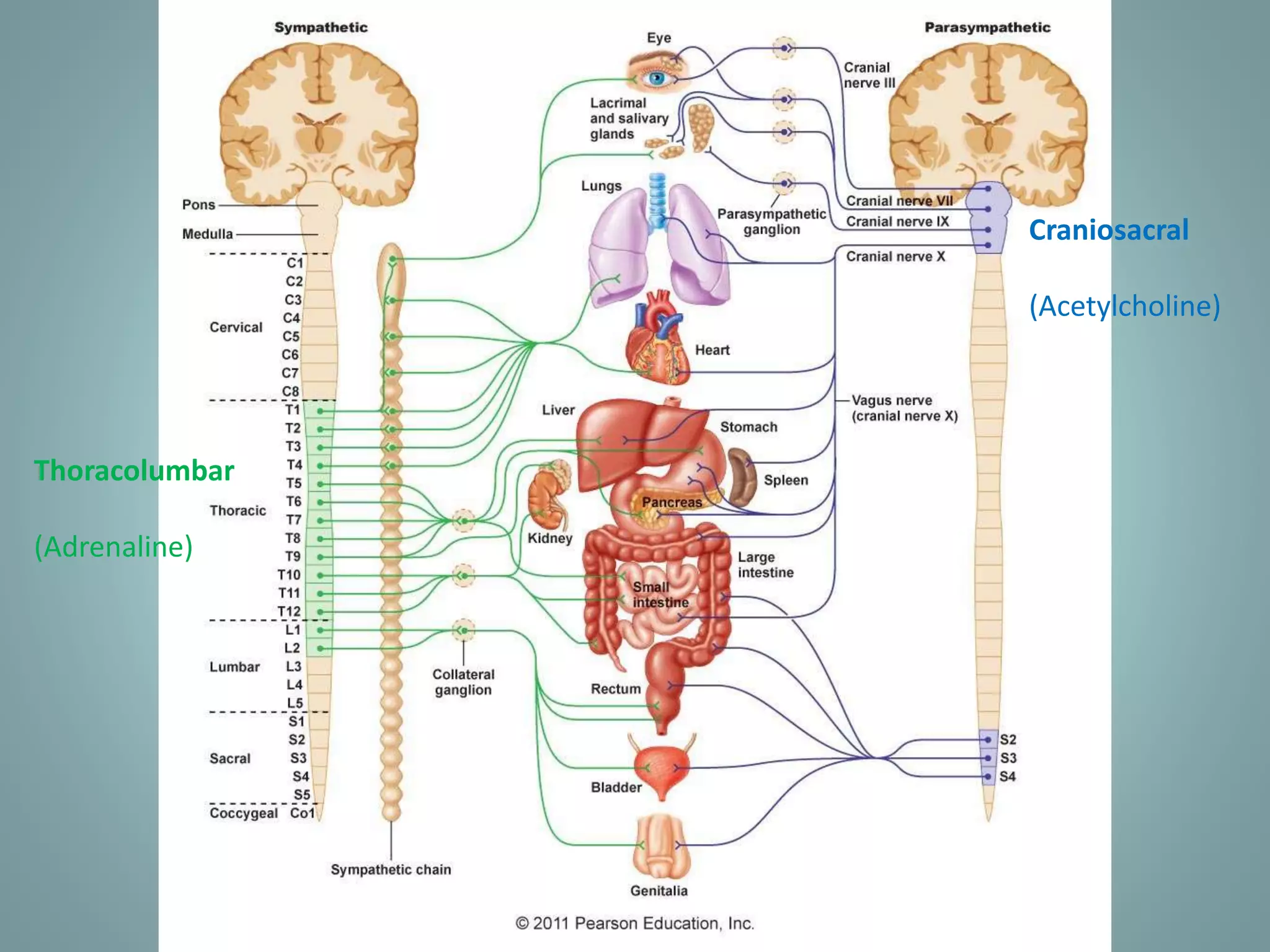
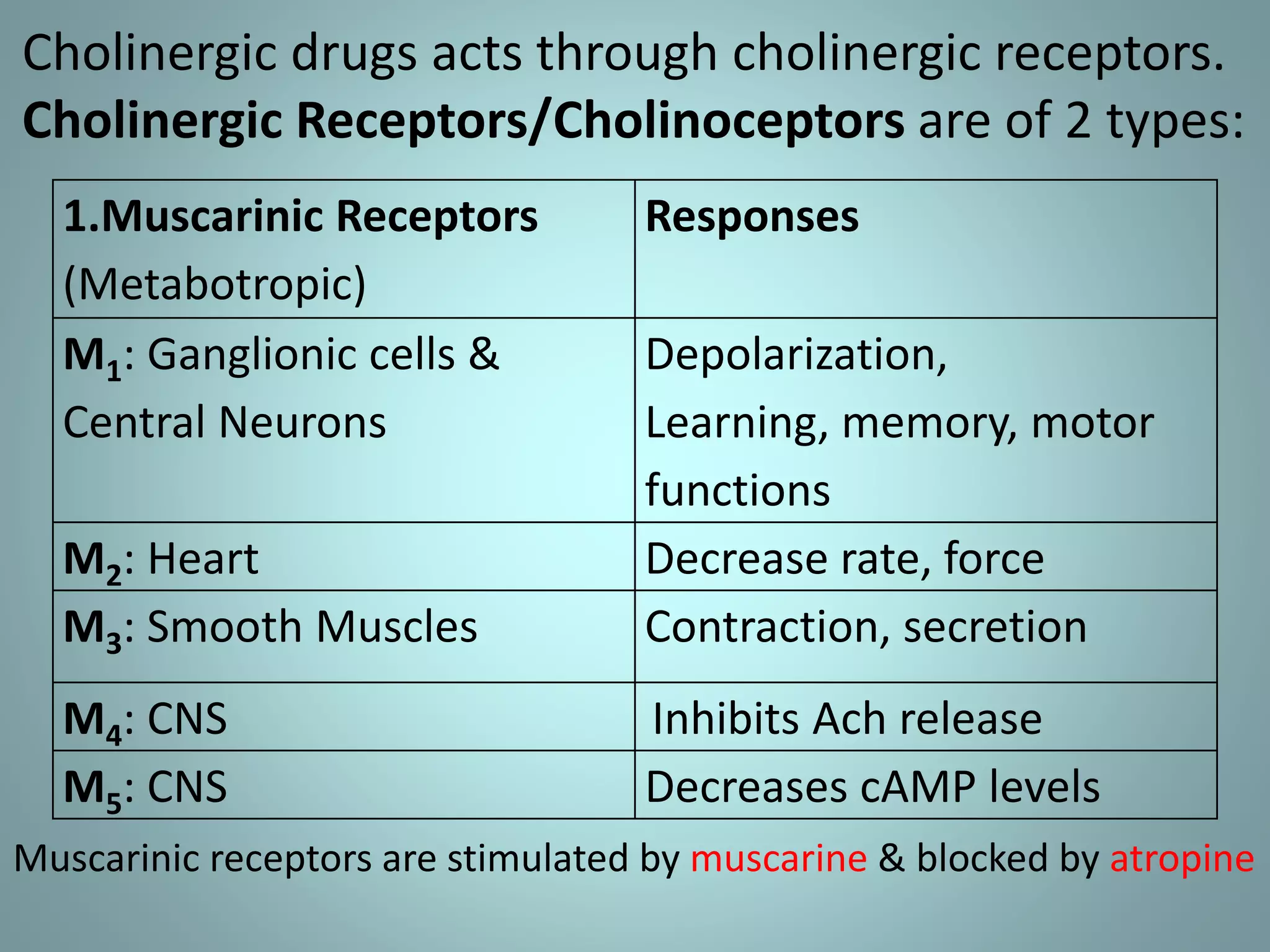
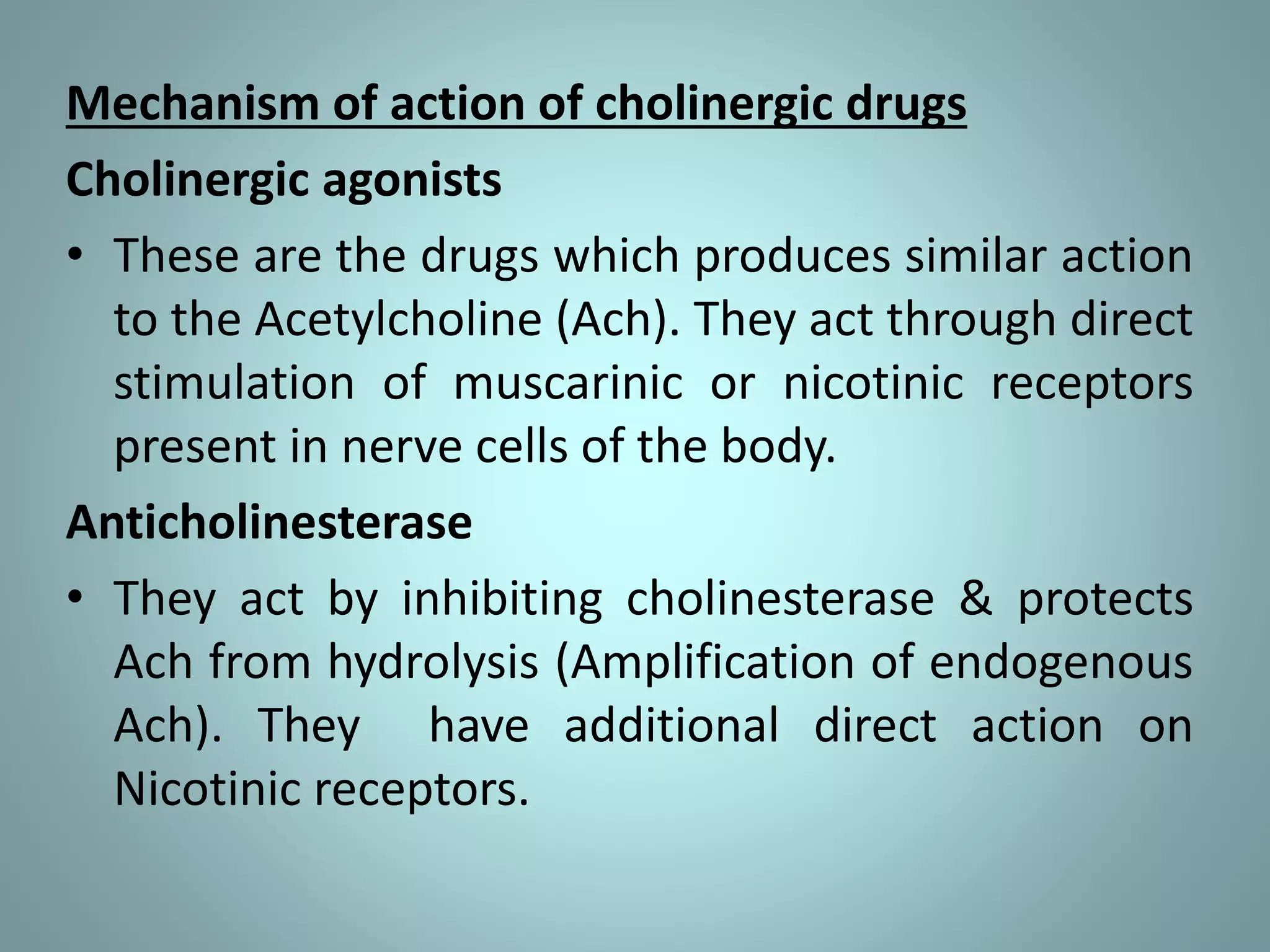
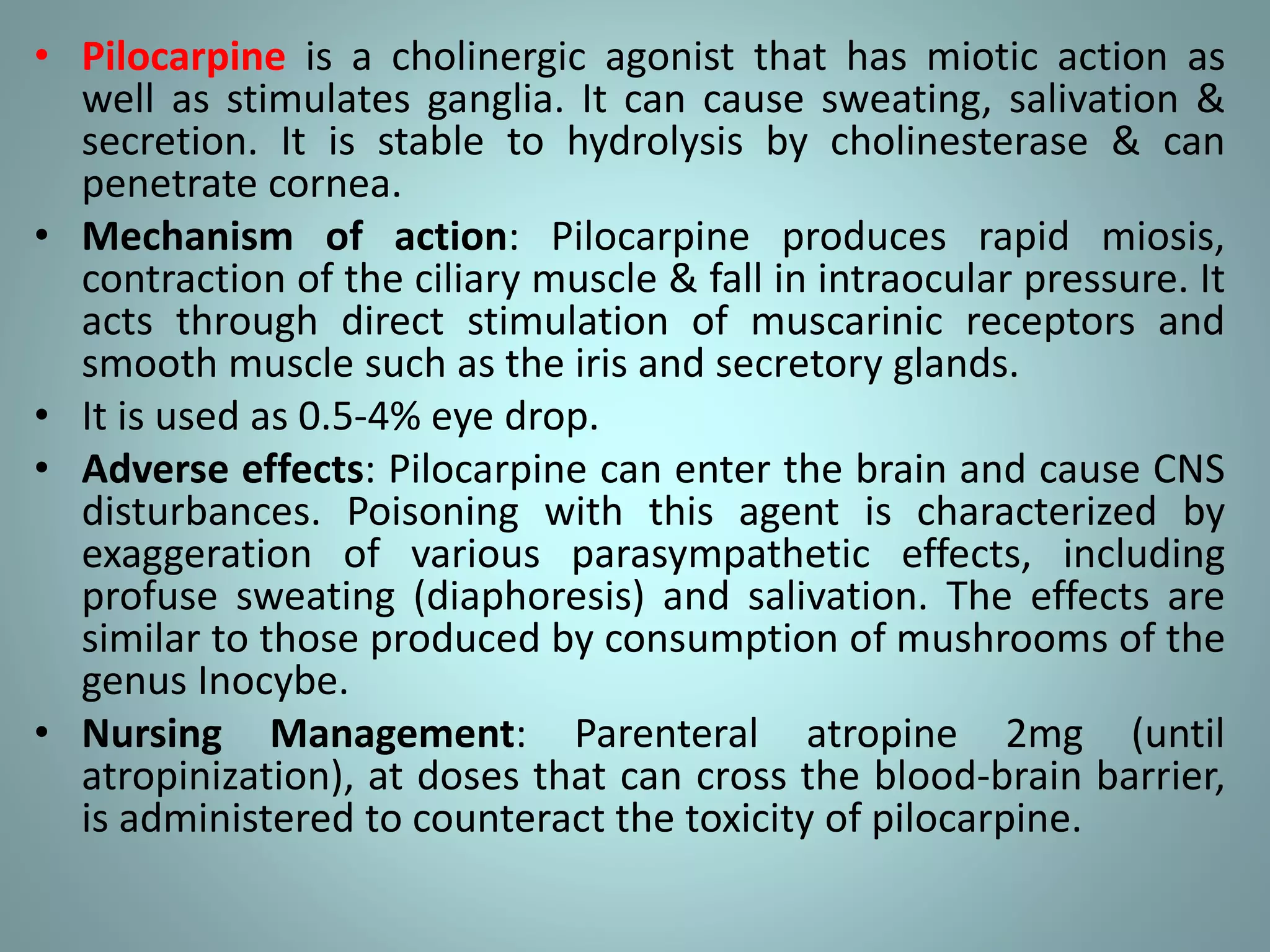
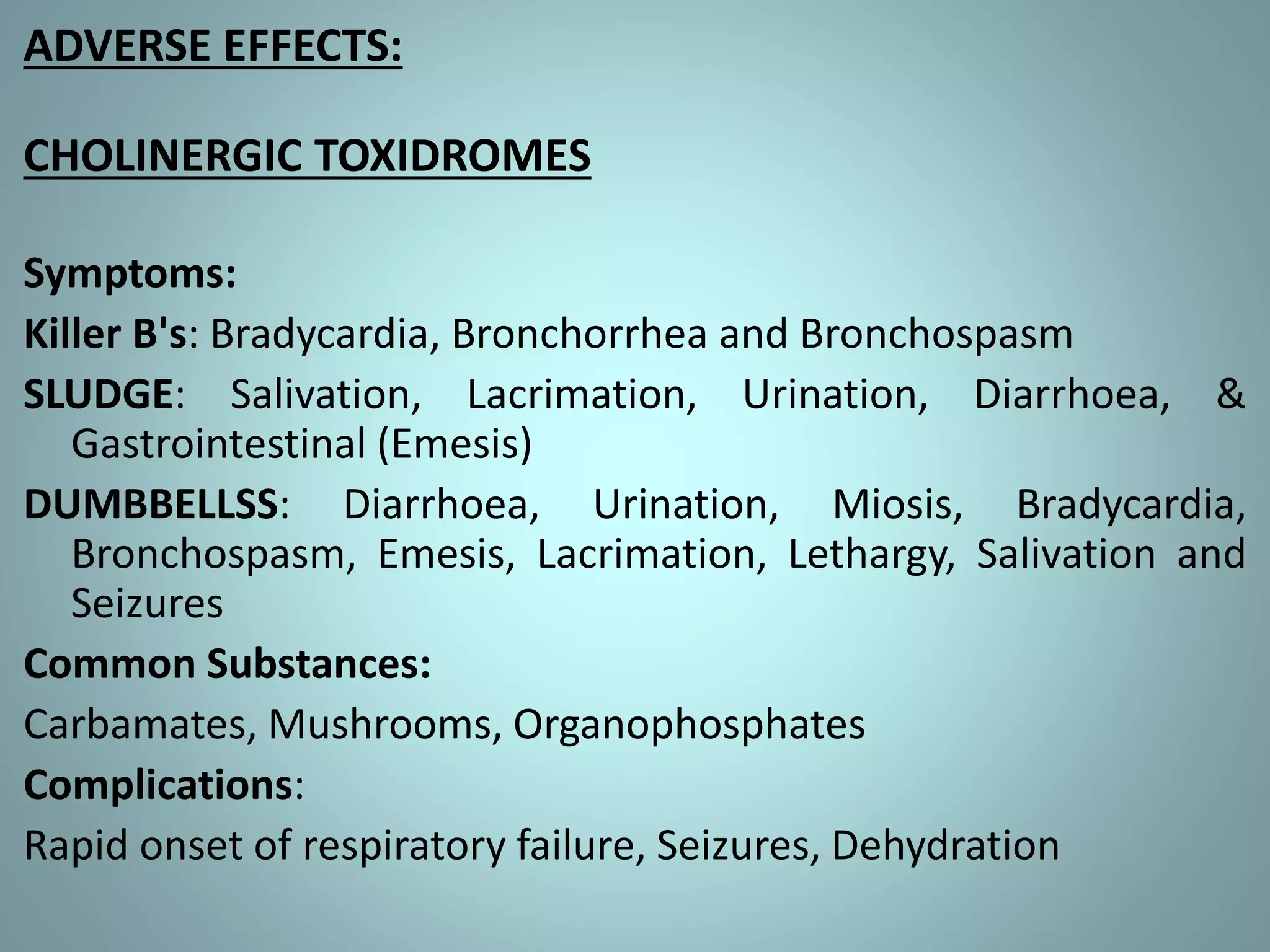
The document provides information about the autonomic nervous system (ANS). It discusses how the ANS controls involuntary functions and maintains homeostasis. It describes the two divisions of the ANS - the sympathetic and parasympathetic nervous systems. The sympathetic system is responsible for the fight or flight response while the parasympathetic system promotes rest and digestion. Cholinergic drugs such as pilocarpine act on muscarinic receptors to cause miosis and are used to treat glaucoma. Anticholinesterase drugs inhibit the breakdown of acetylcholine and are used for myasthenia gravis and organophosphate poisoning.