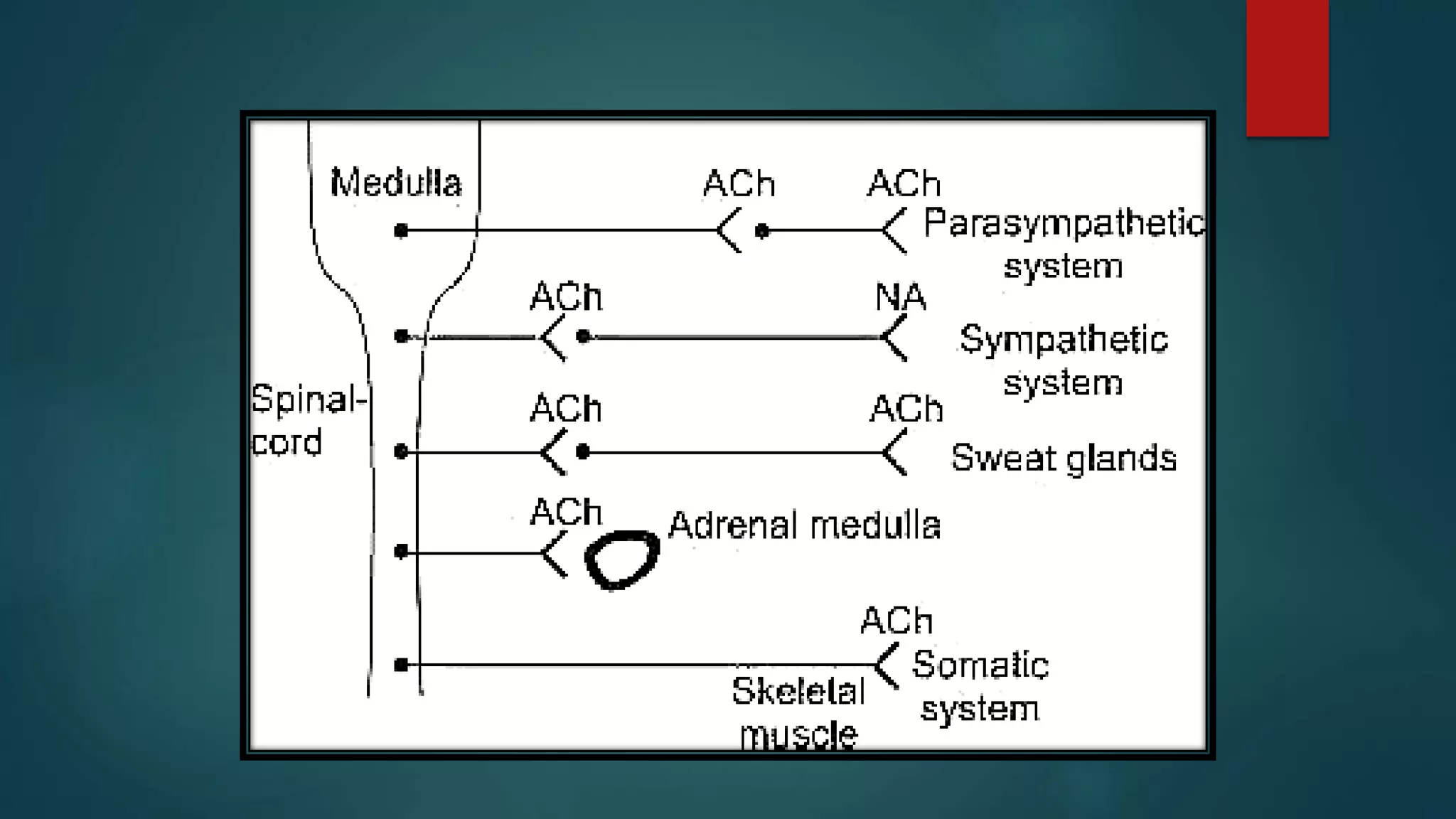
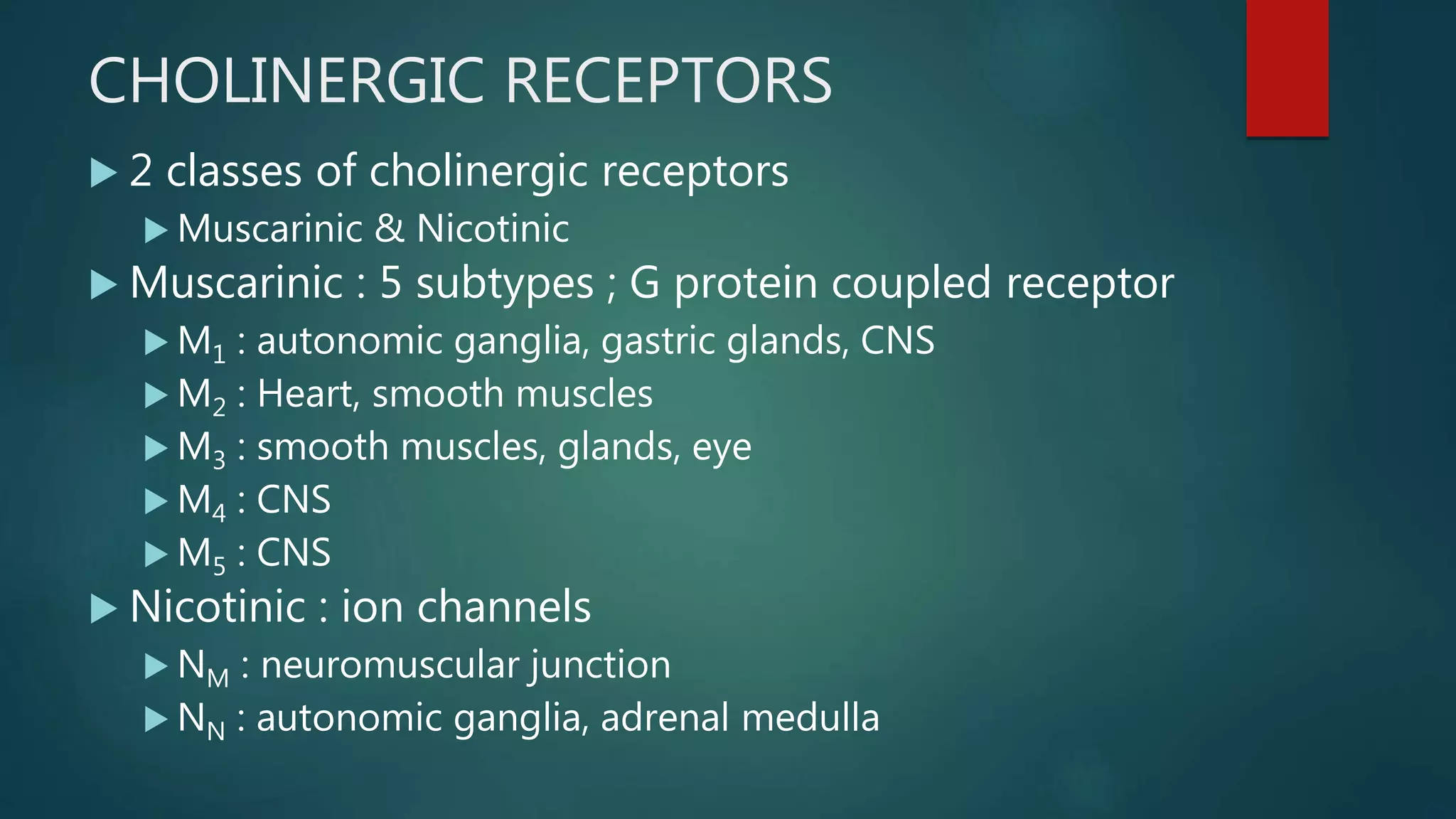
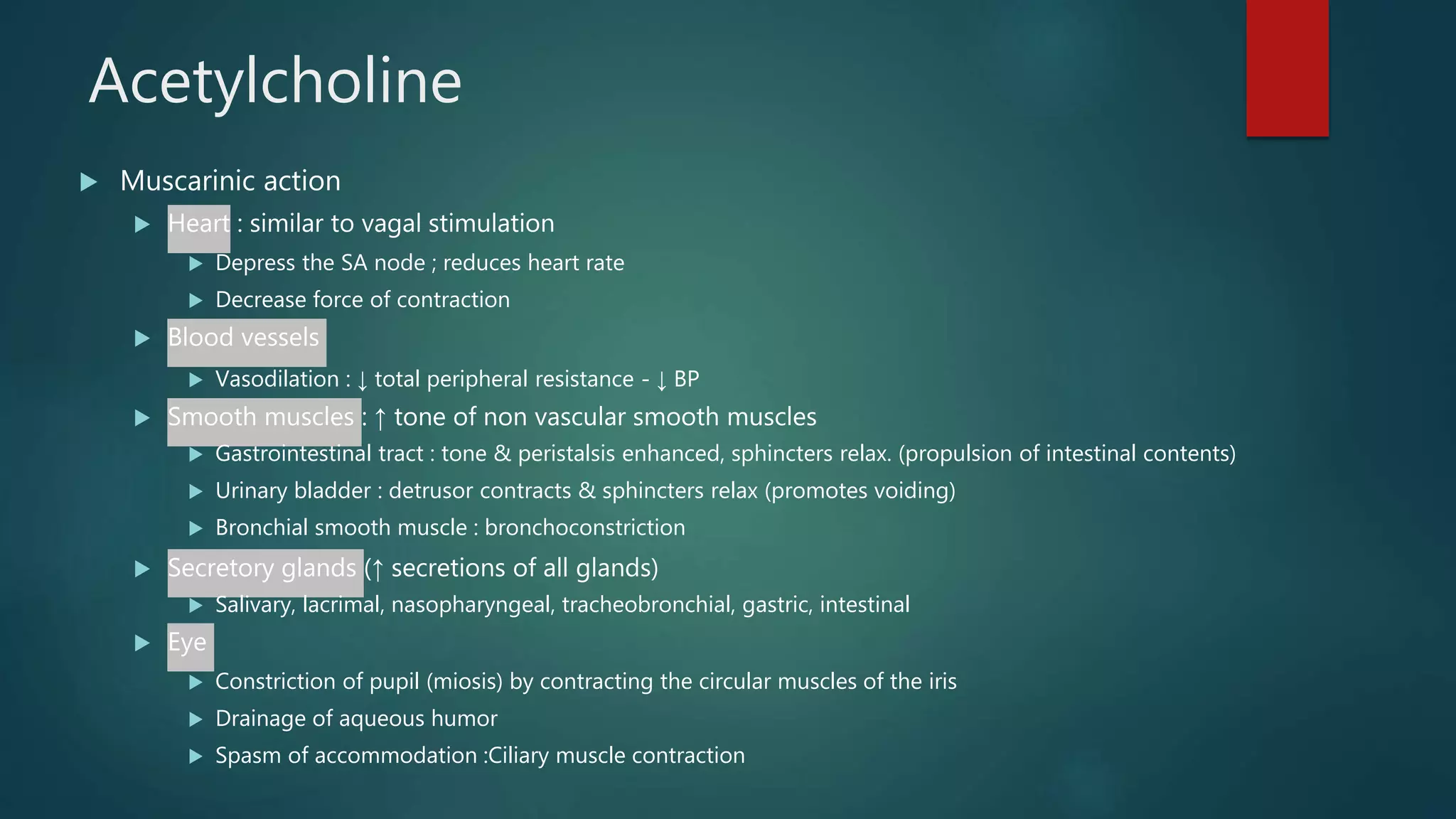
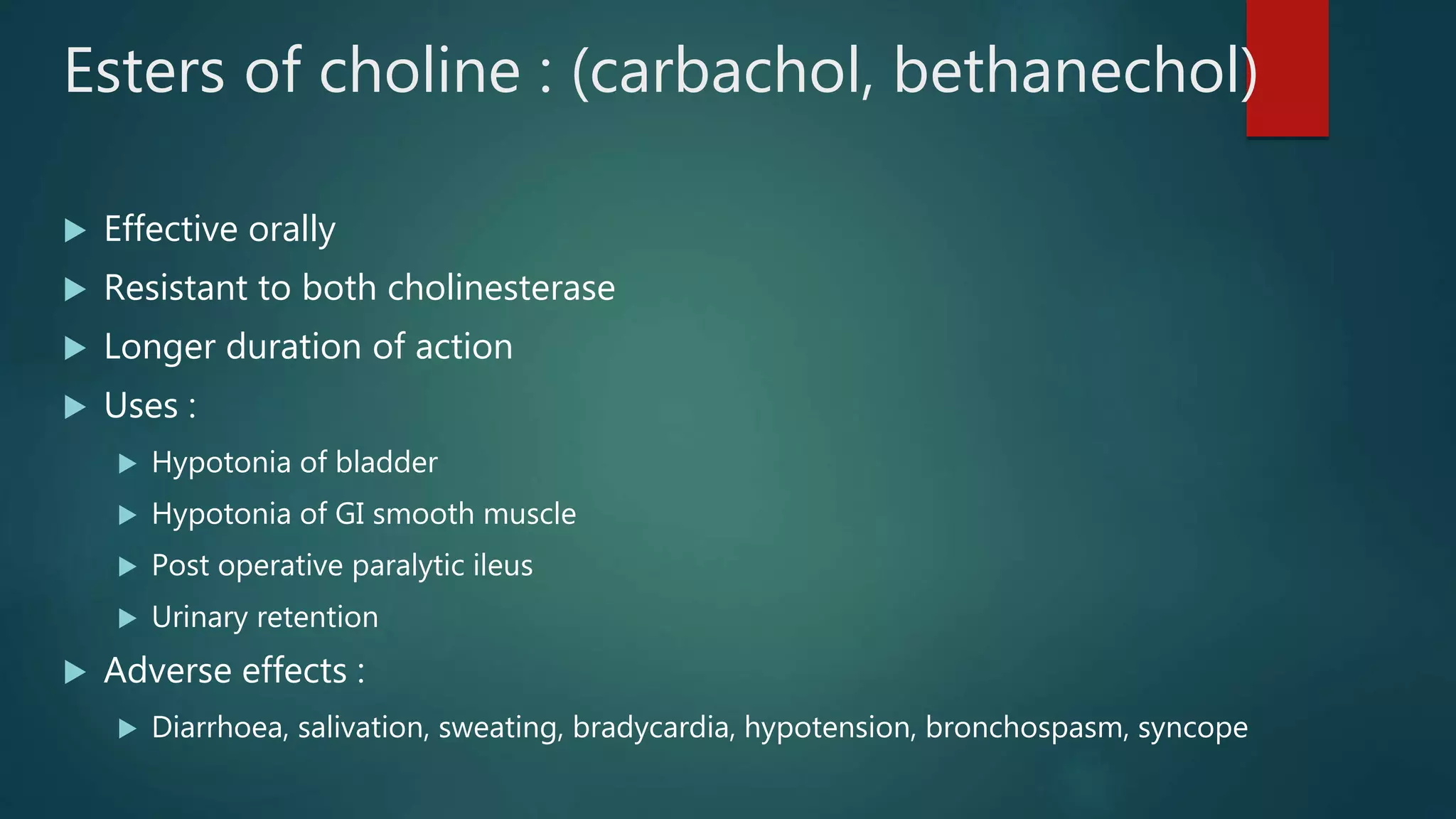
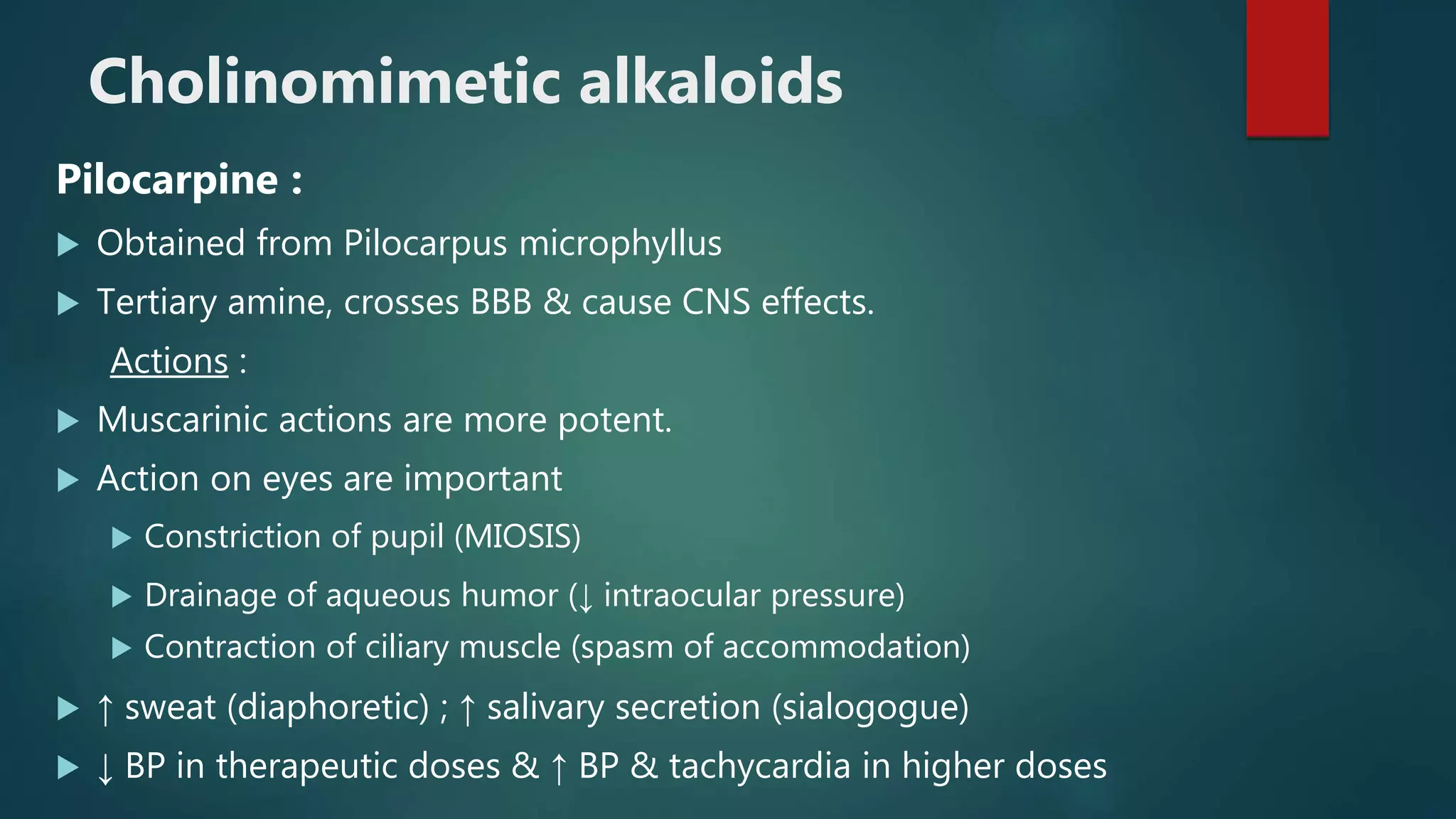
The document provides an overview of the autonomic nervous system and cholinergic system. It discusses how acetylcholine is the neurotransmitter of the parasympathetic nervous system and cholinergic fibers. It describes the two classes of cholinergic receptors - muscarinic and nicotinic receptors. It also summarizes several cholinergic drugs, including direct-acting cholinergic drugs like acetylcholine, and indirect-acting anticholinesterase drugs.

![ Autonomic nervous system innervates the heart, smooth muscle,
the glands & the viscera.
Centres for the autonomic reflexes are present in the
hypothalamus, medulla & spinal cord.
Hypothalamus coordinates the autonomic activity.
Two major division : sympathetic & parasympathetic.
These 2 divisions have opposing effects & normally their effects
are in a state of equilibrium.
Sympathetic : flight & fight
Parasympathetic : tissue building [rest & digest / feed & breed]](https://image.slidesharecdn.com/cholinergicsystem-200624095634/75/Cholinergic-system-3-2048.jpg)