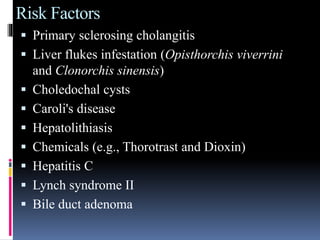
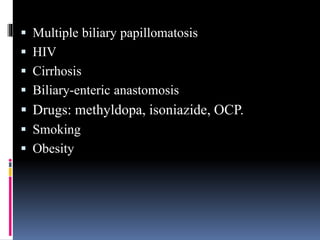
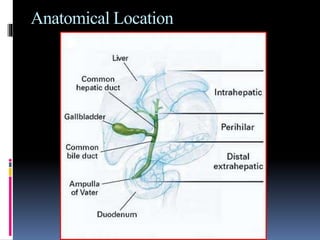
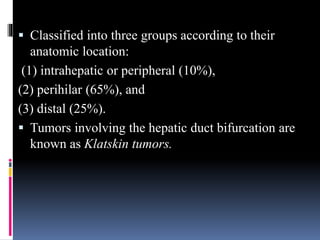
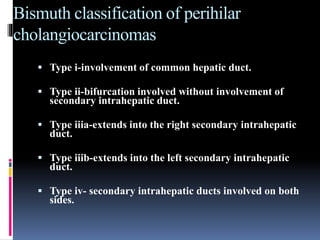
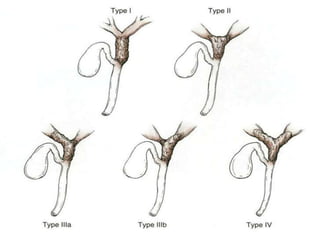
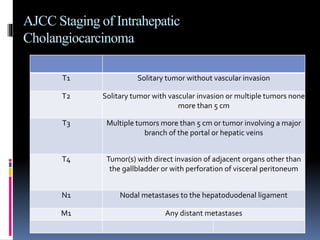
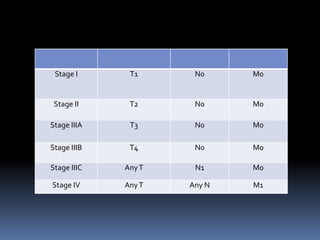
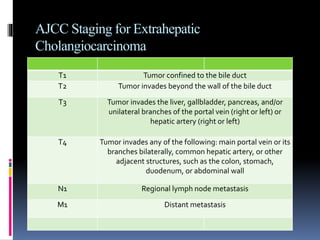
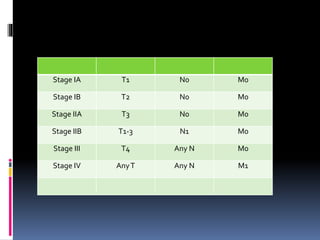
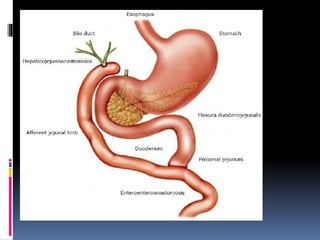
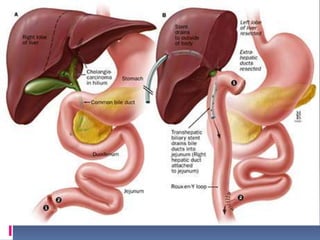
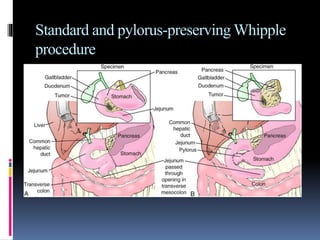
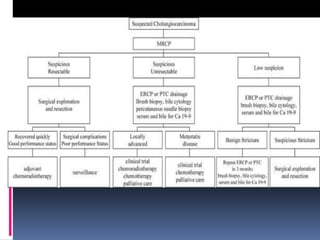
Cholangiocarcinoma is a rare cancer that affects the bile ducts. It occurs most often in older adults and risk factors include primary sclerosing cholangitis and liver flukes. The cancer is classified based on location and can be intrahepatic, perihilar, or distal. Surgical resection is the main treatment if the cancer is resectable, while palliative options are used for unresectable cases to relieve symptoms of biliary obstruction. Prognosis is generally poor due to late diagnosis but resection provides the best chance for survival.