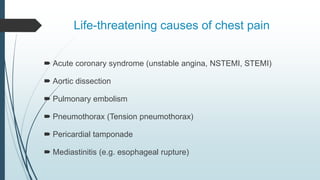
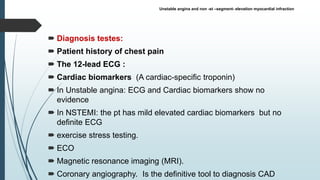
The document provides a comprehensive overview of acute chest pain, detailing its potential causes, assessments, and diagnosis methods. It categorizes causes into cardiac and non-cardiac events, highlights life-threatening conditions like acute coronary syndrome and pulmonary embolism, and outlines treatment protocols including oxygen therapy and antiplatelet medications. Additionally, it discusses differential diagnoses and various related conditions, including pericarditis and pleurisy, alongside nursing roles for managing patients with chest pain.