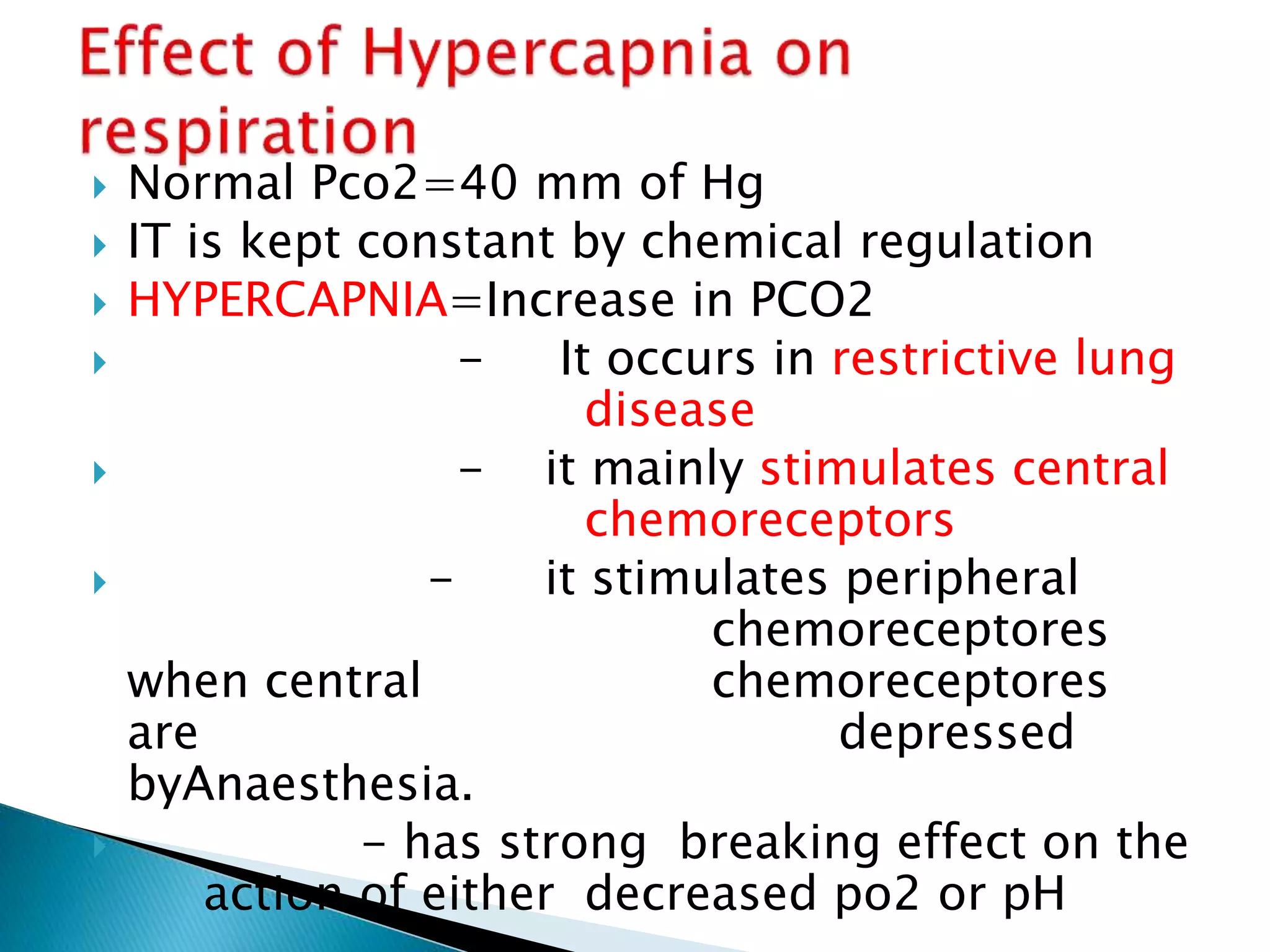
This document discusses various types of chemoreceptors that regulate respiration in response to changes in oxygen, carbon dioxide, and hydrogen ion levels in the blood. It describes peripheral chemoreceptors located in the carotid bodies and aortic bodies that are sensitive to low oxygen levels. Central chemoreceptors located in the brainstem are mainly sensitive to increased carbon dioxide levels, which cause increased hydrogen ion concentrations and stimulate breathing. Pulmonary and myocardial chemoreceptors are also discussed.