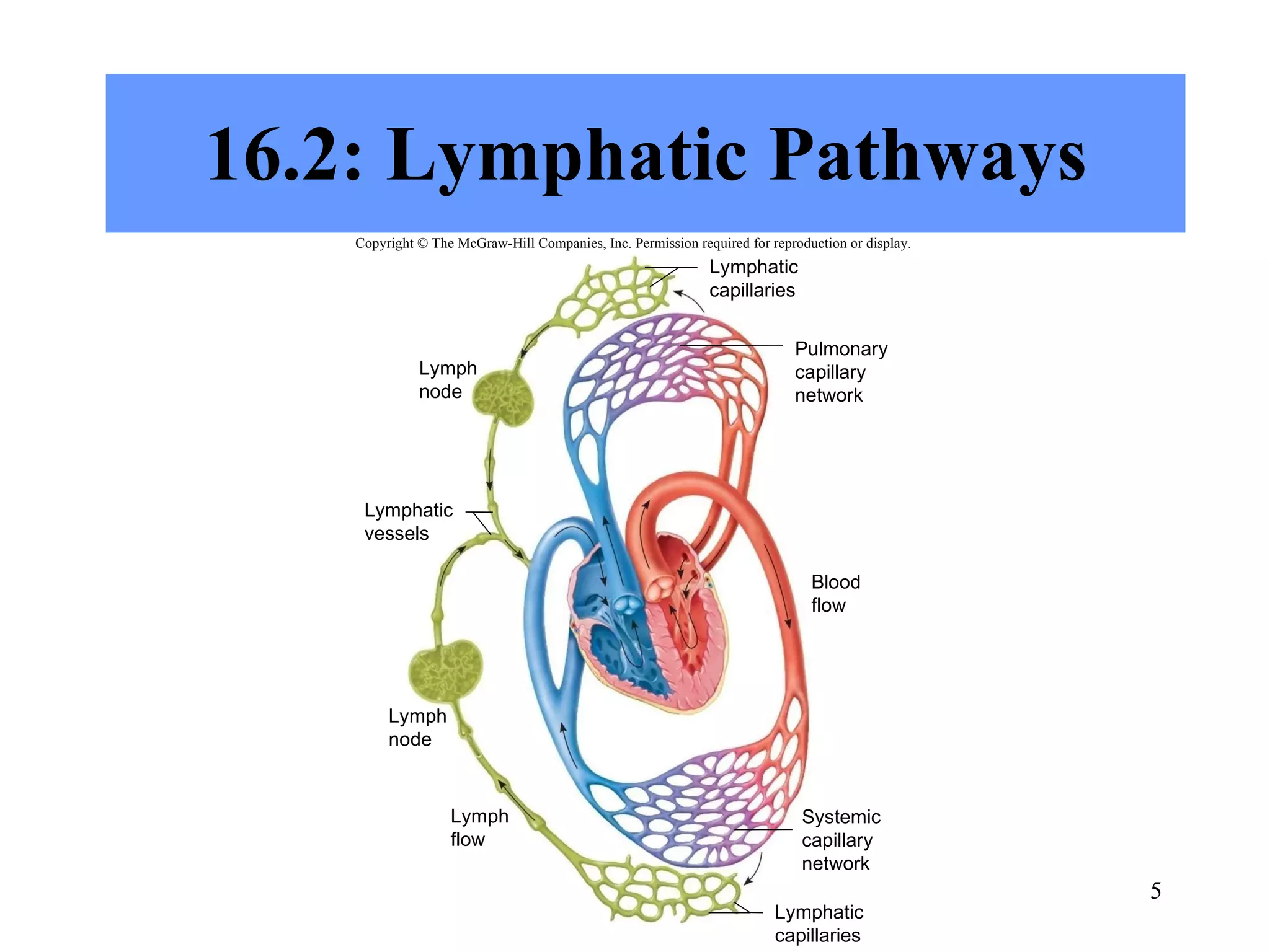
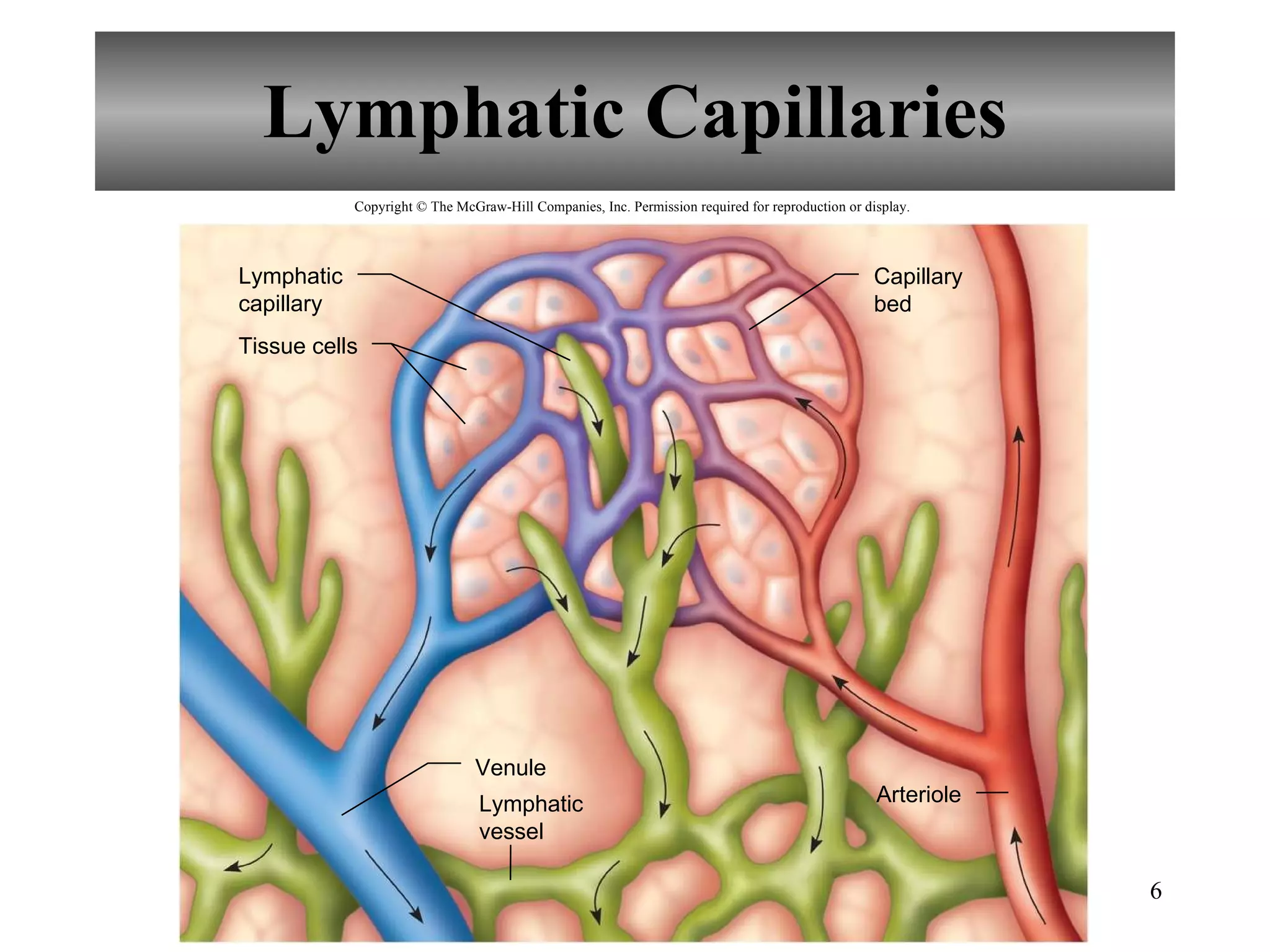
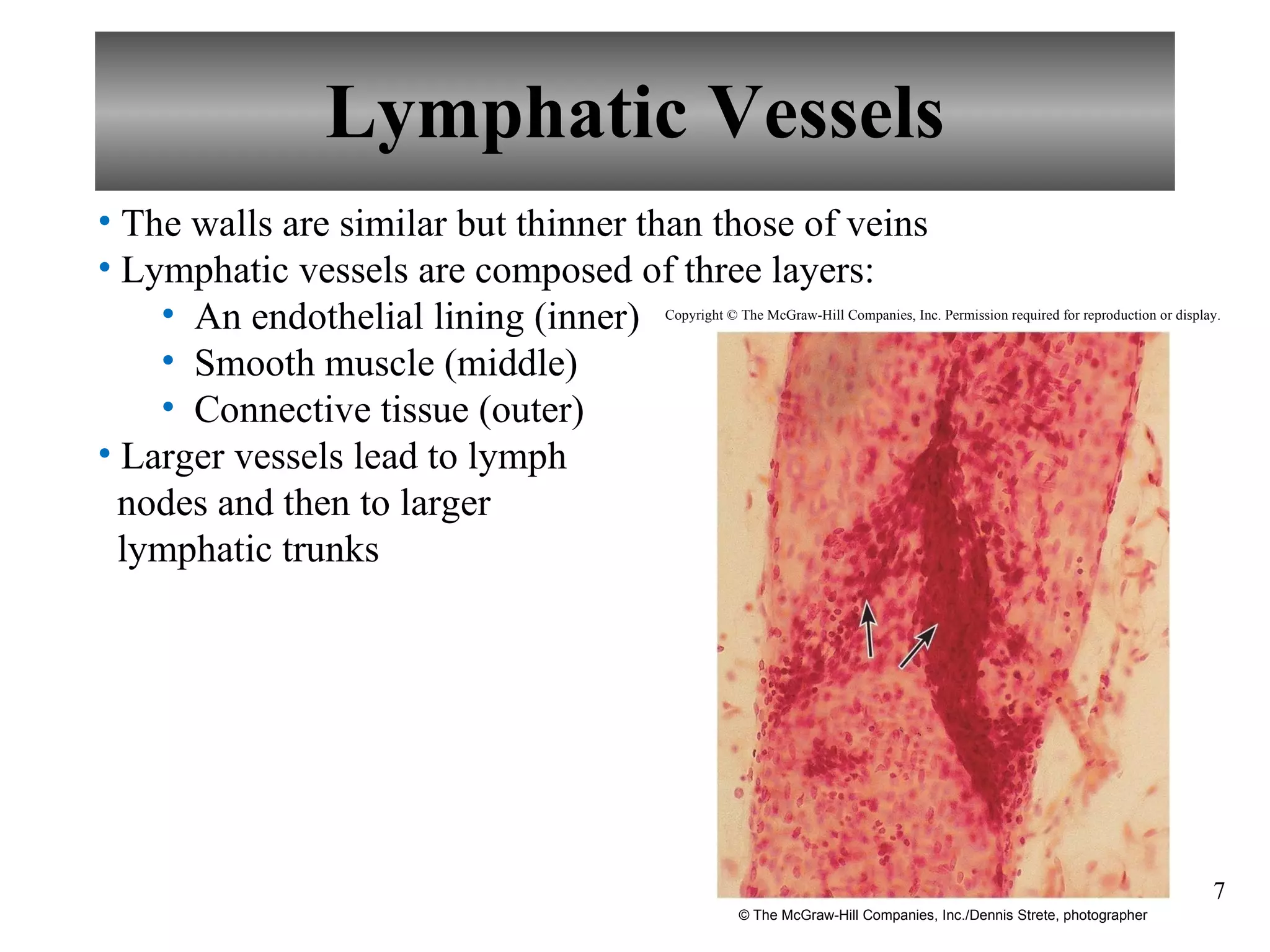
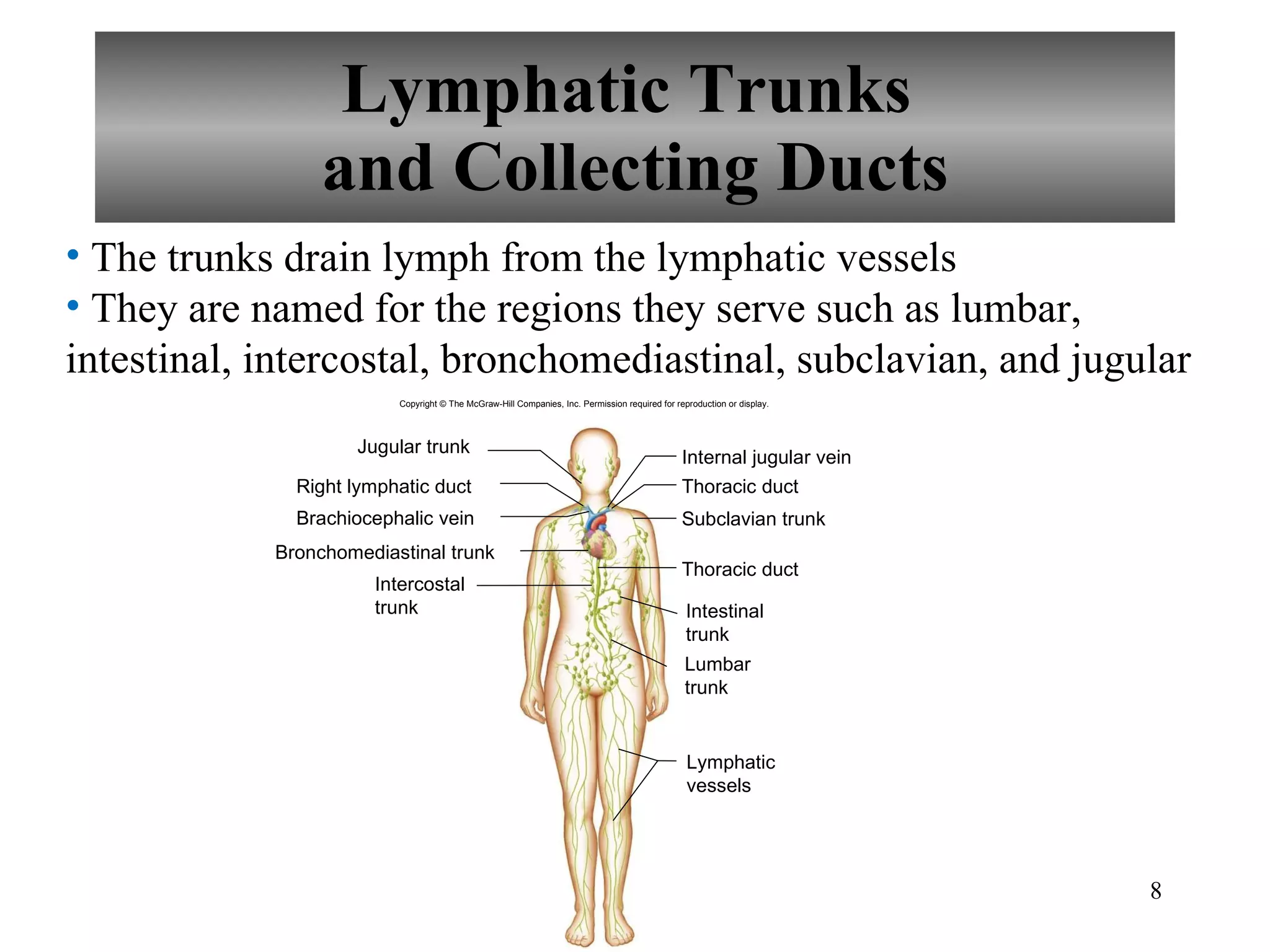
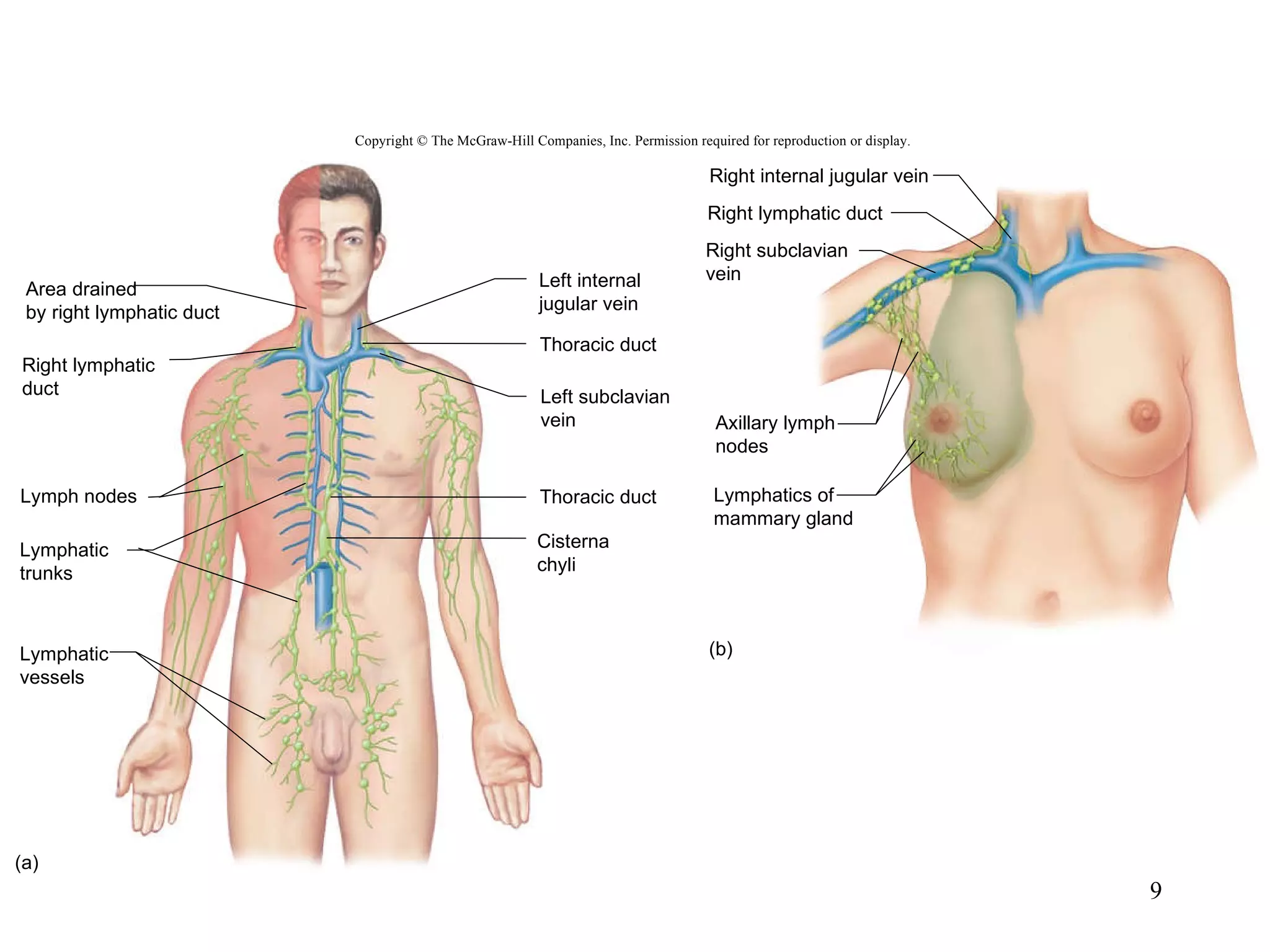
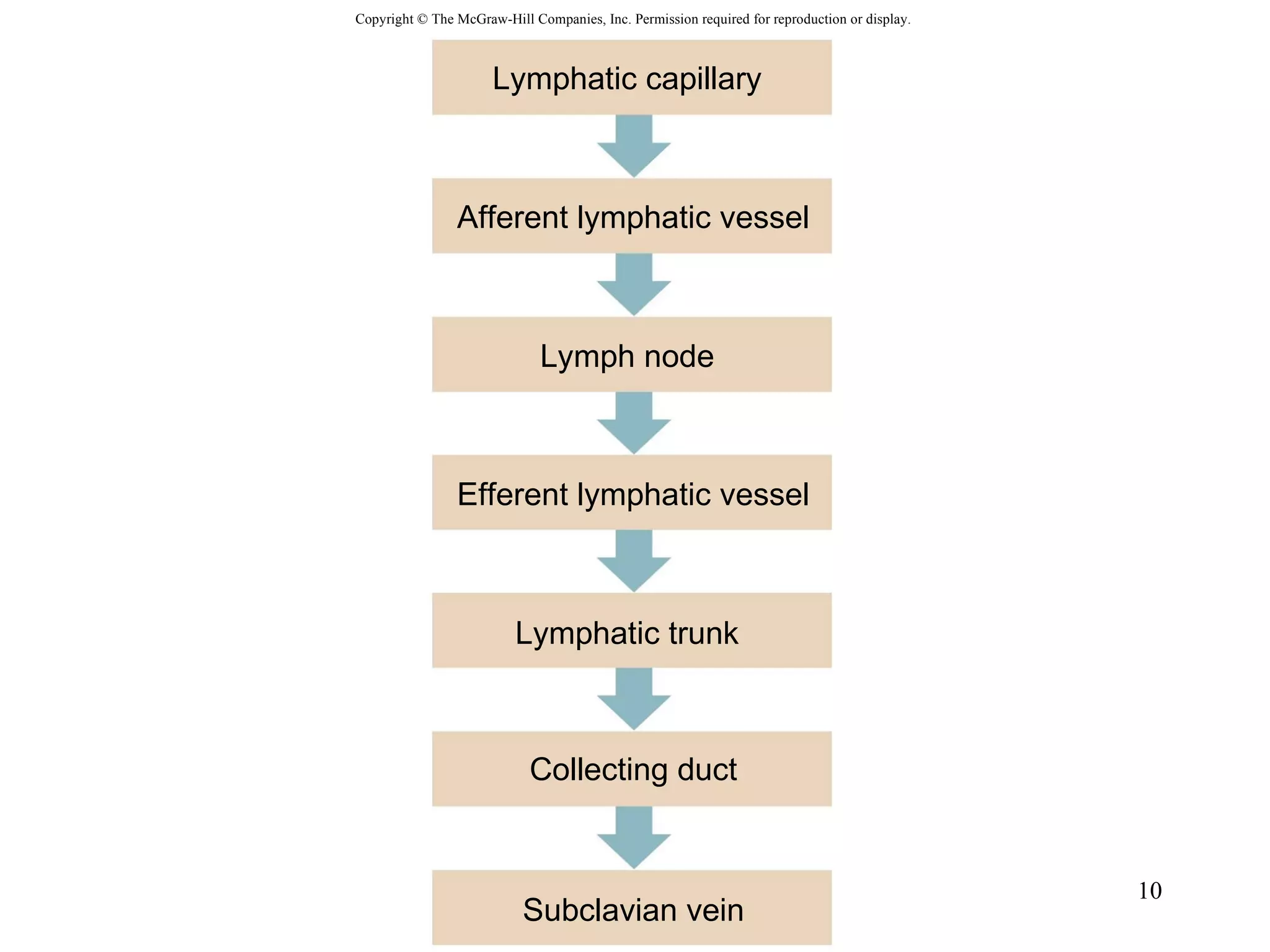
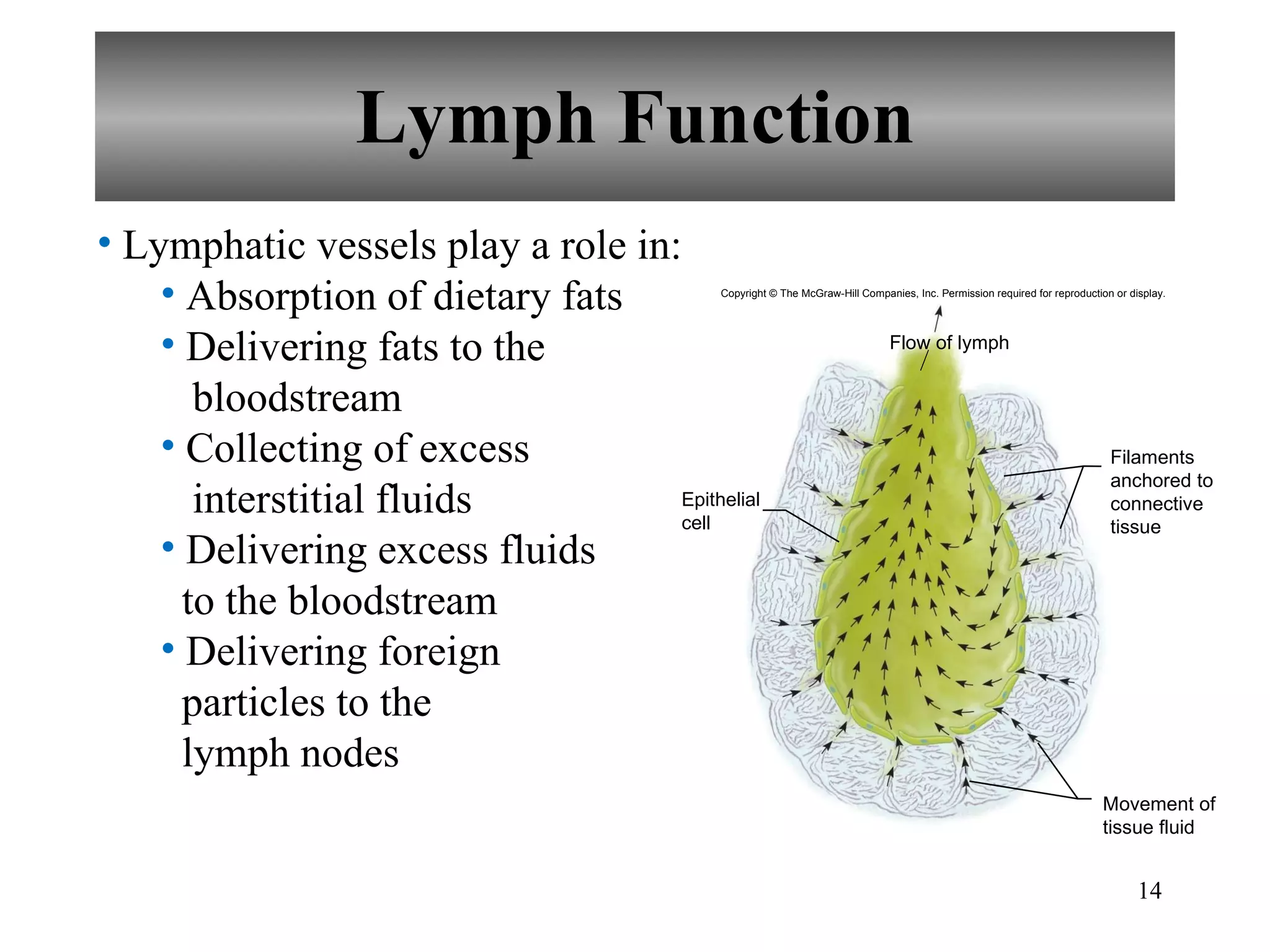
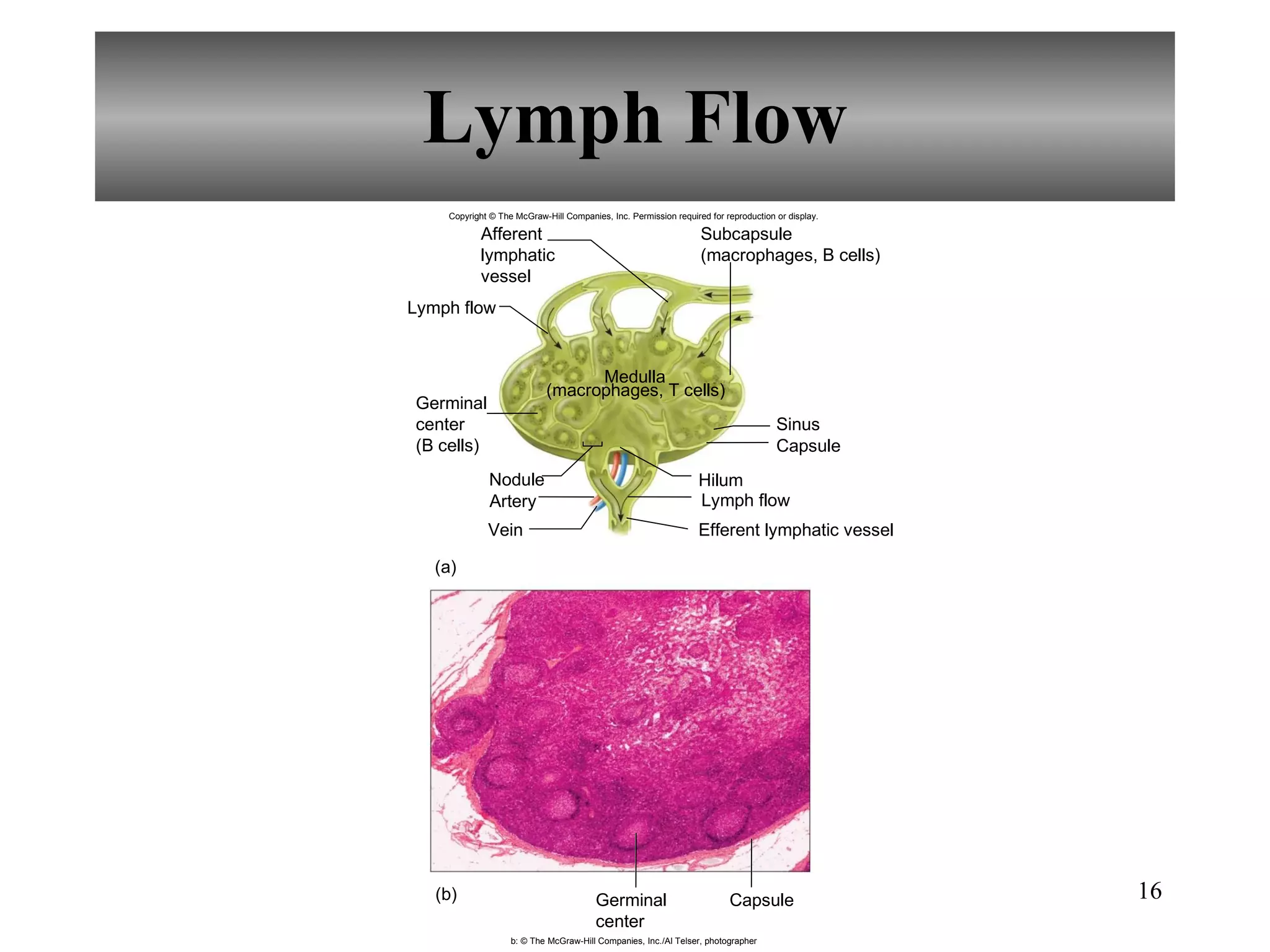
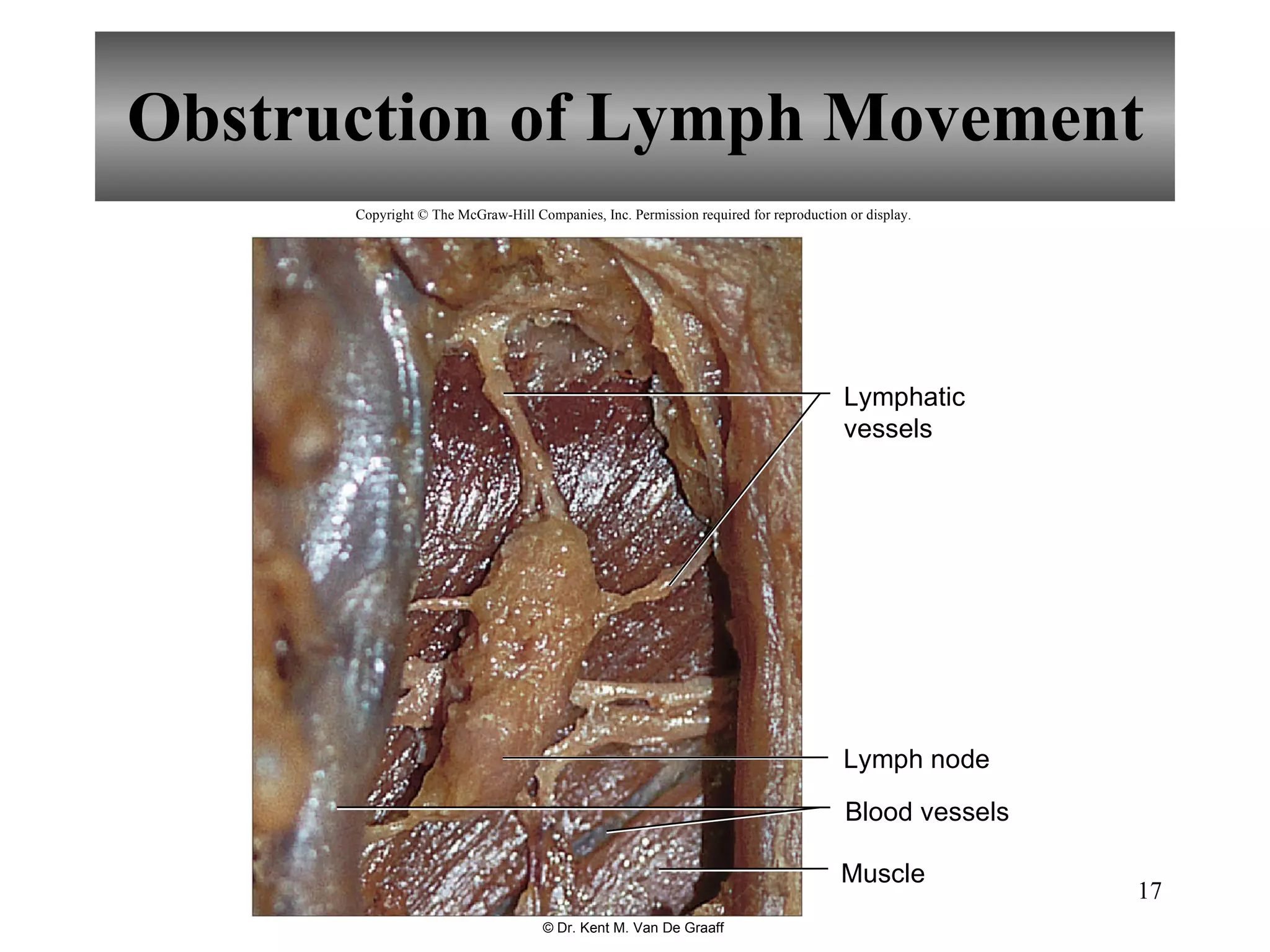
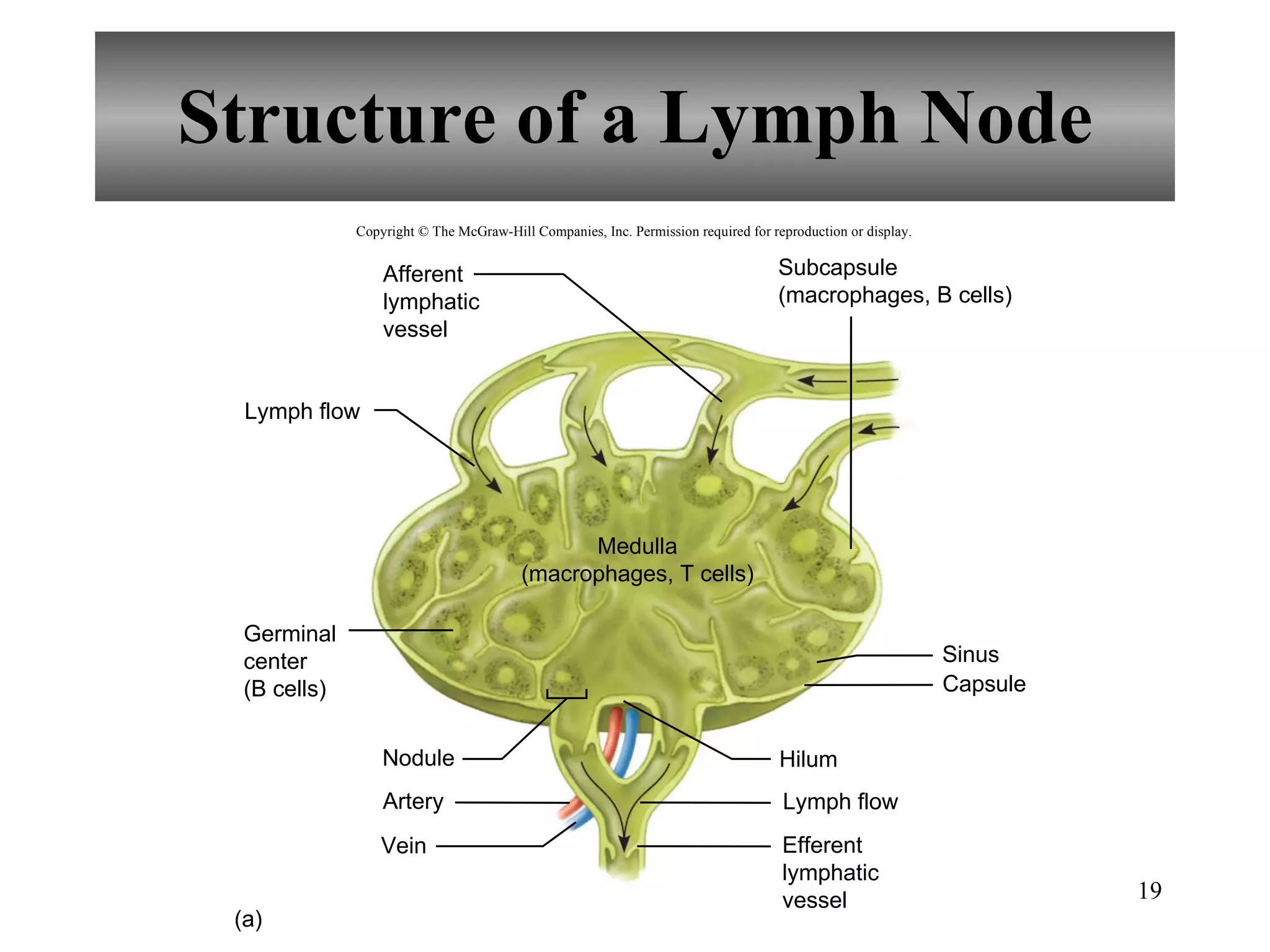
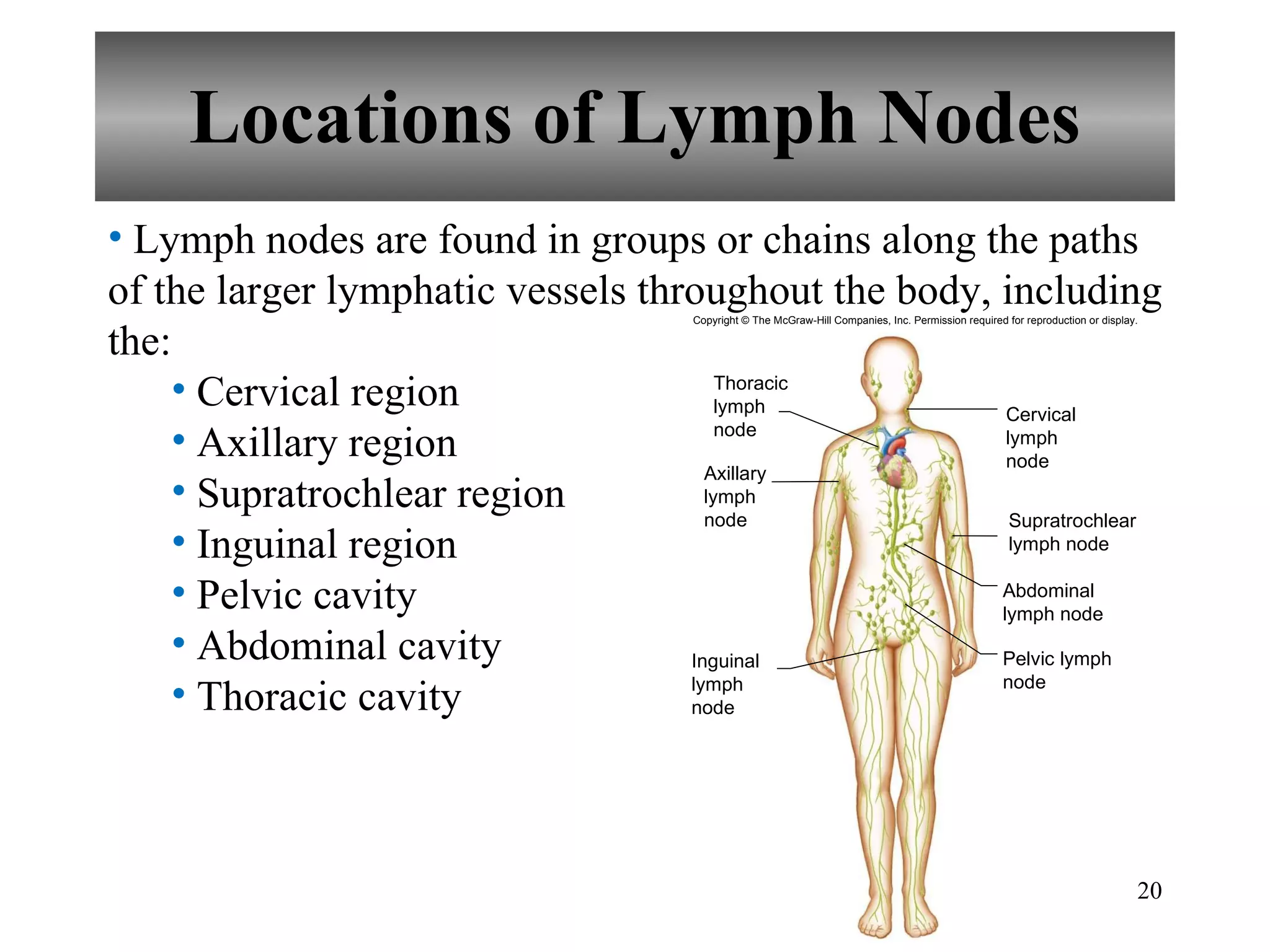
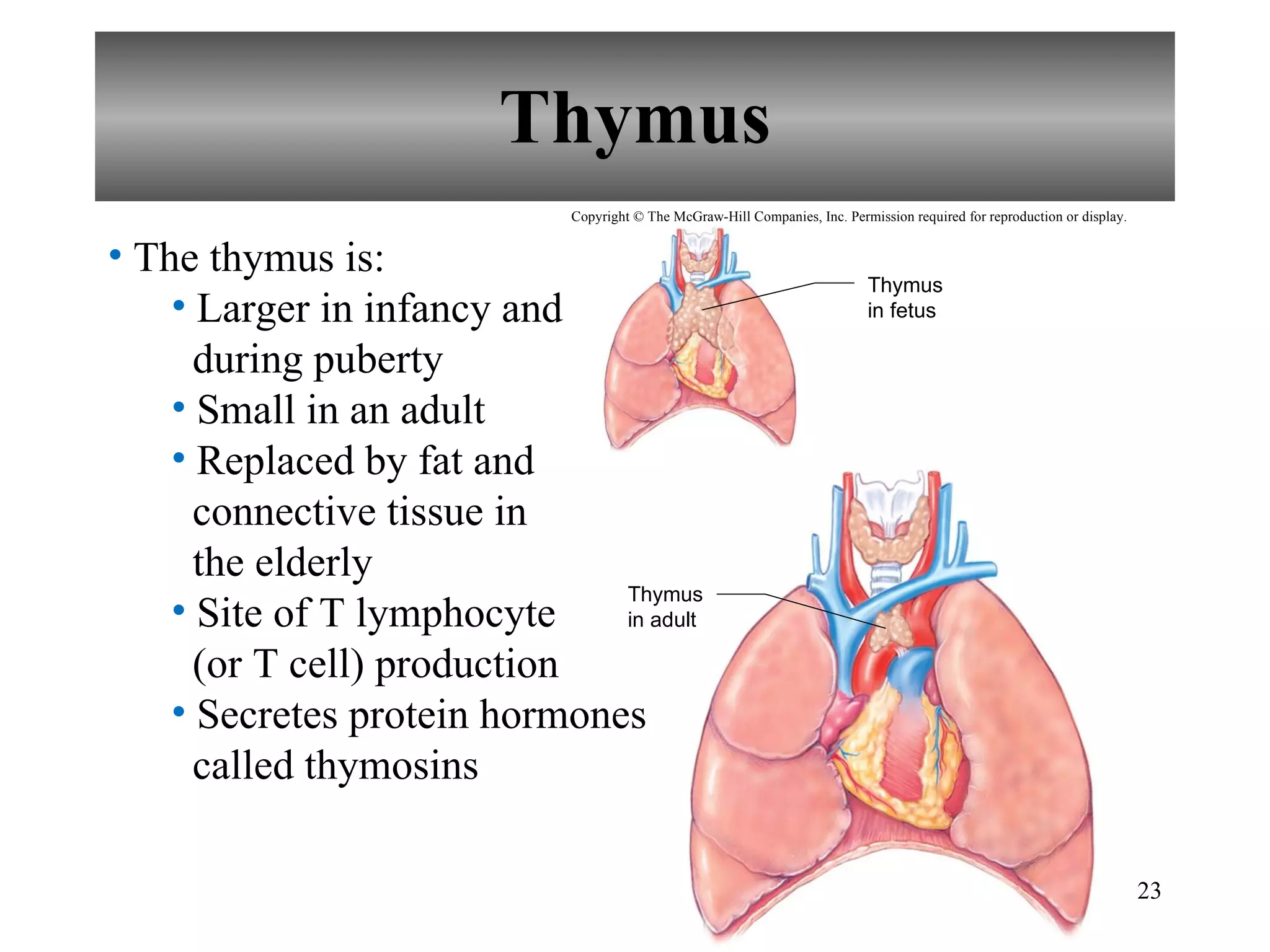
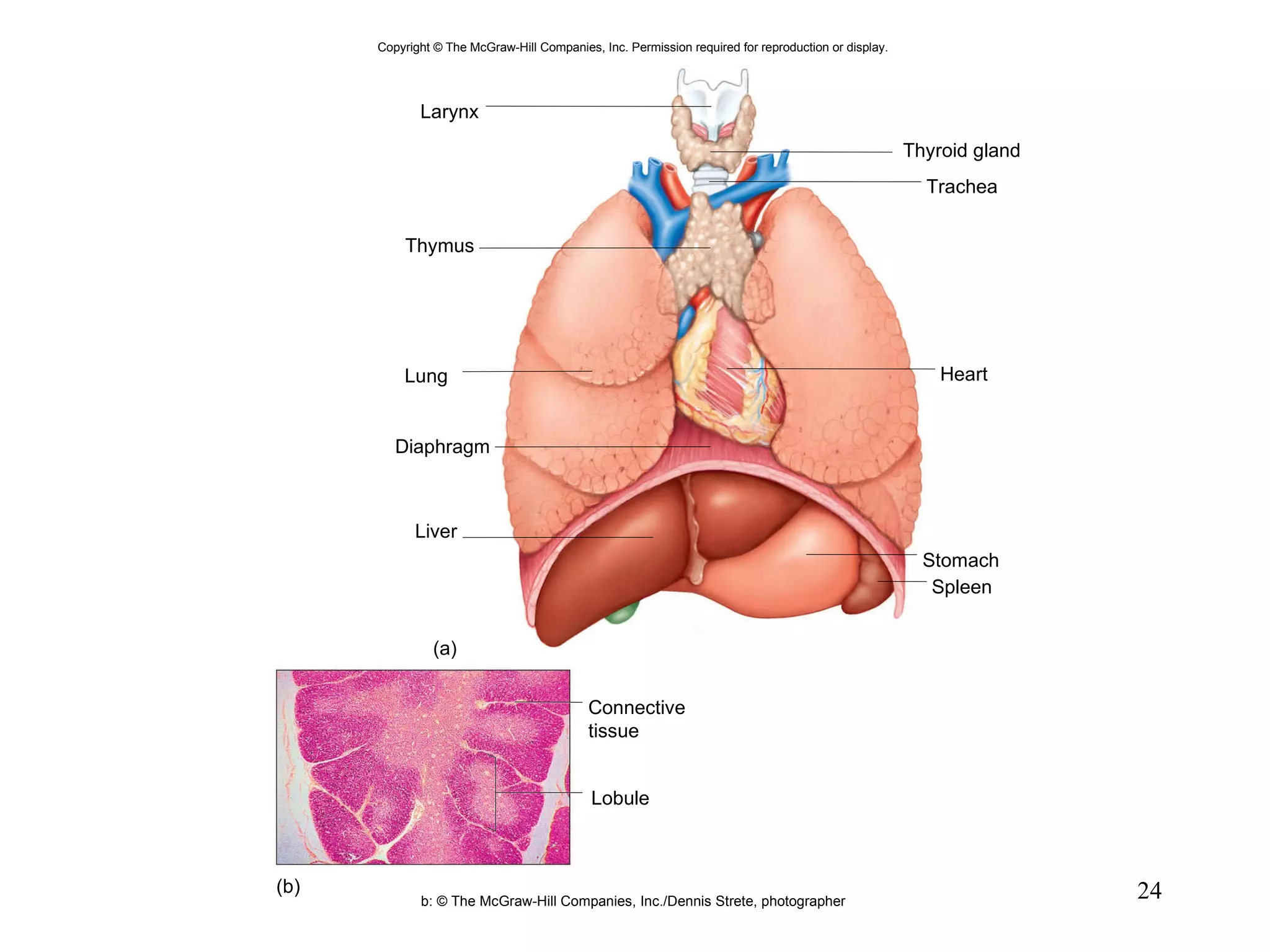
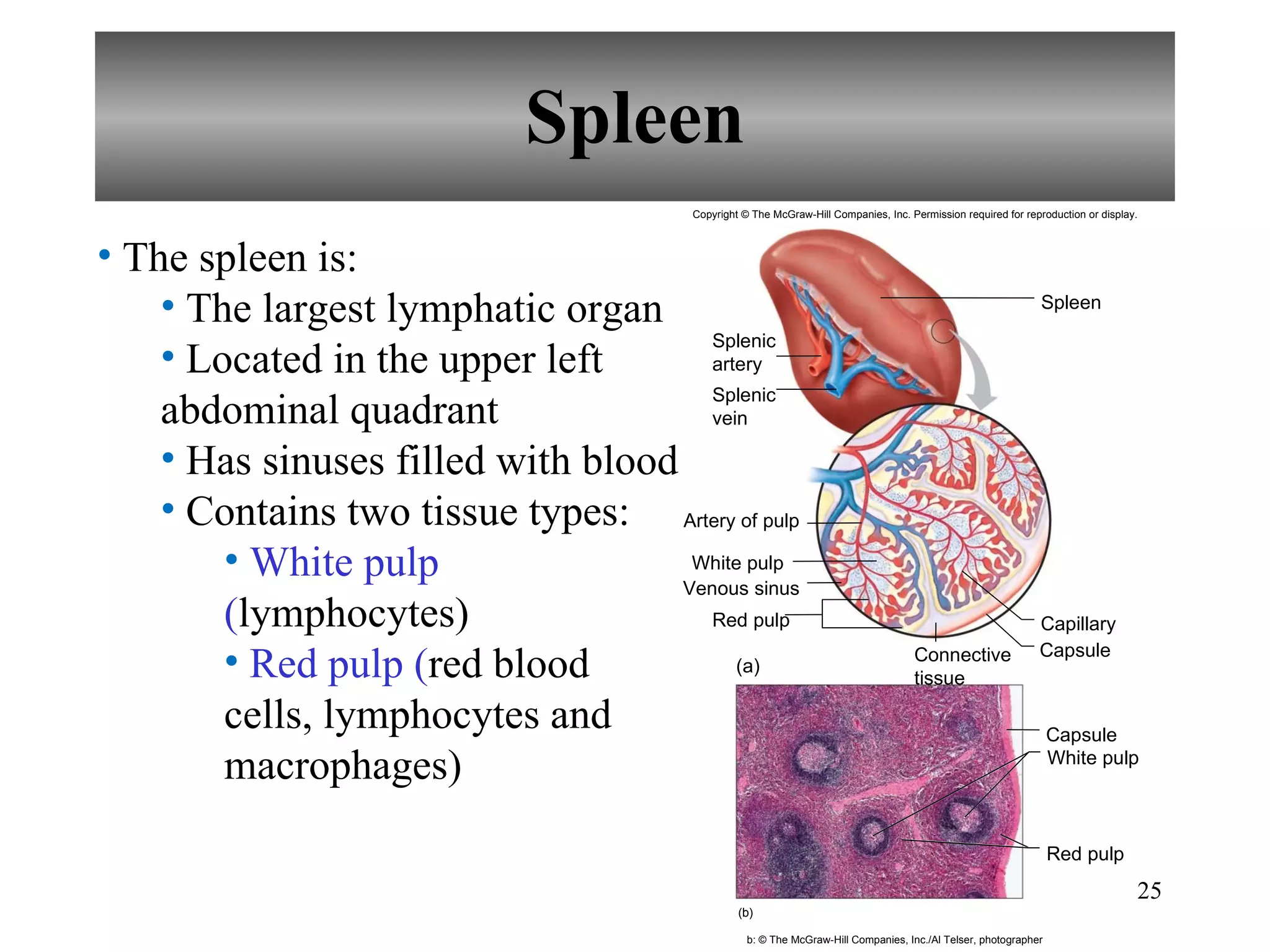
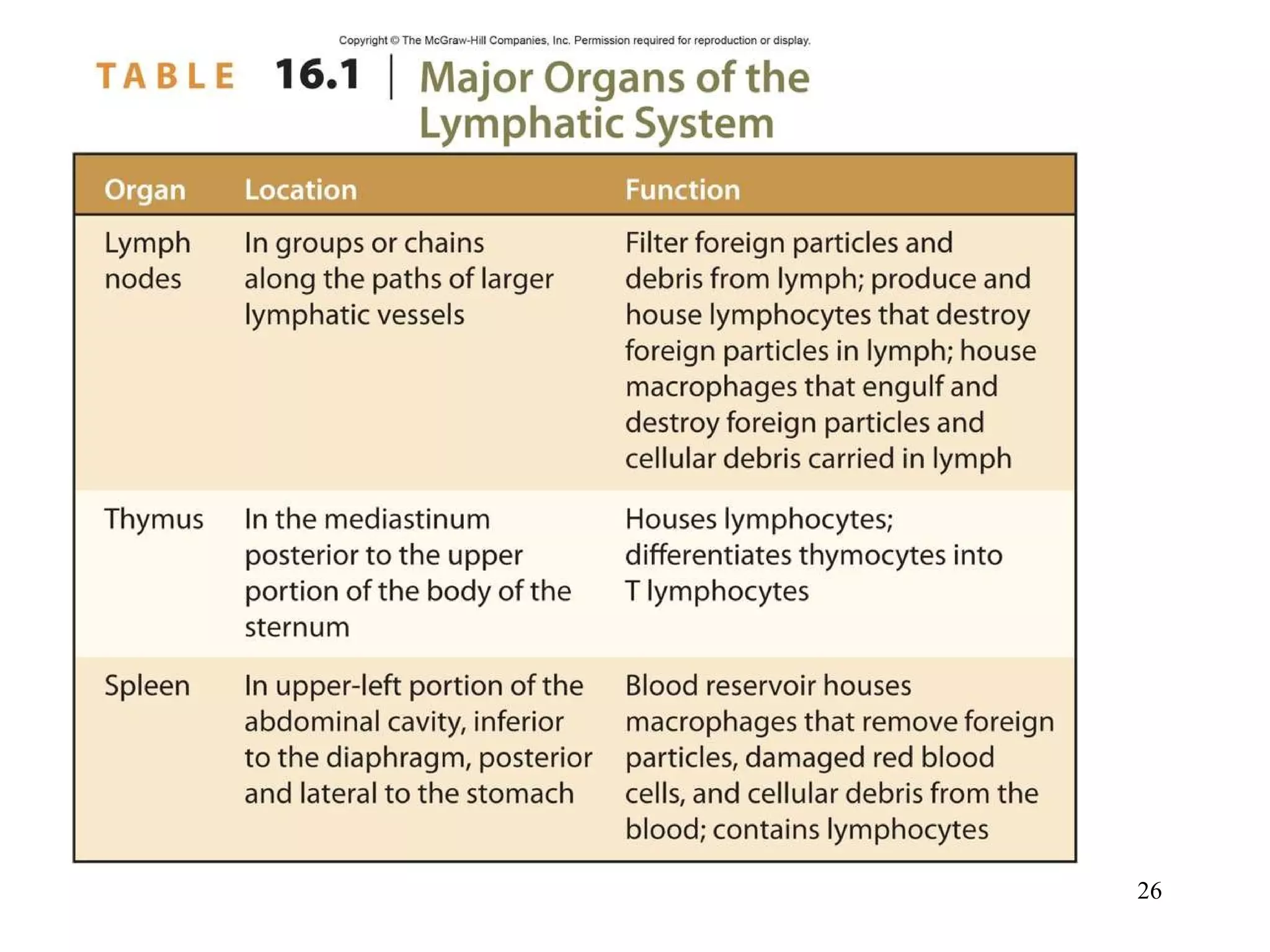
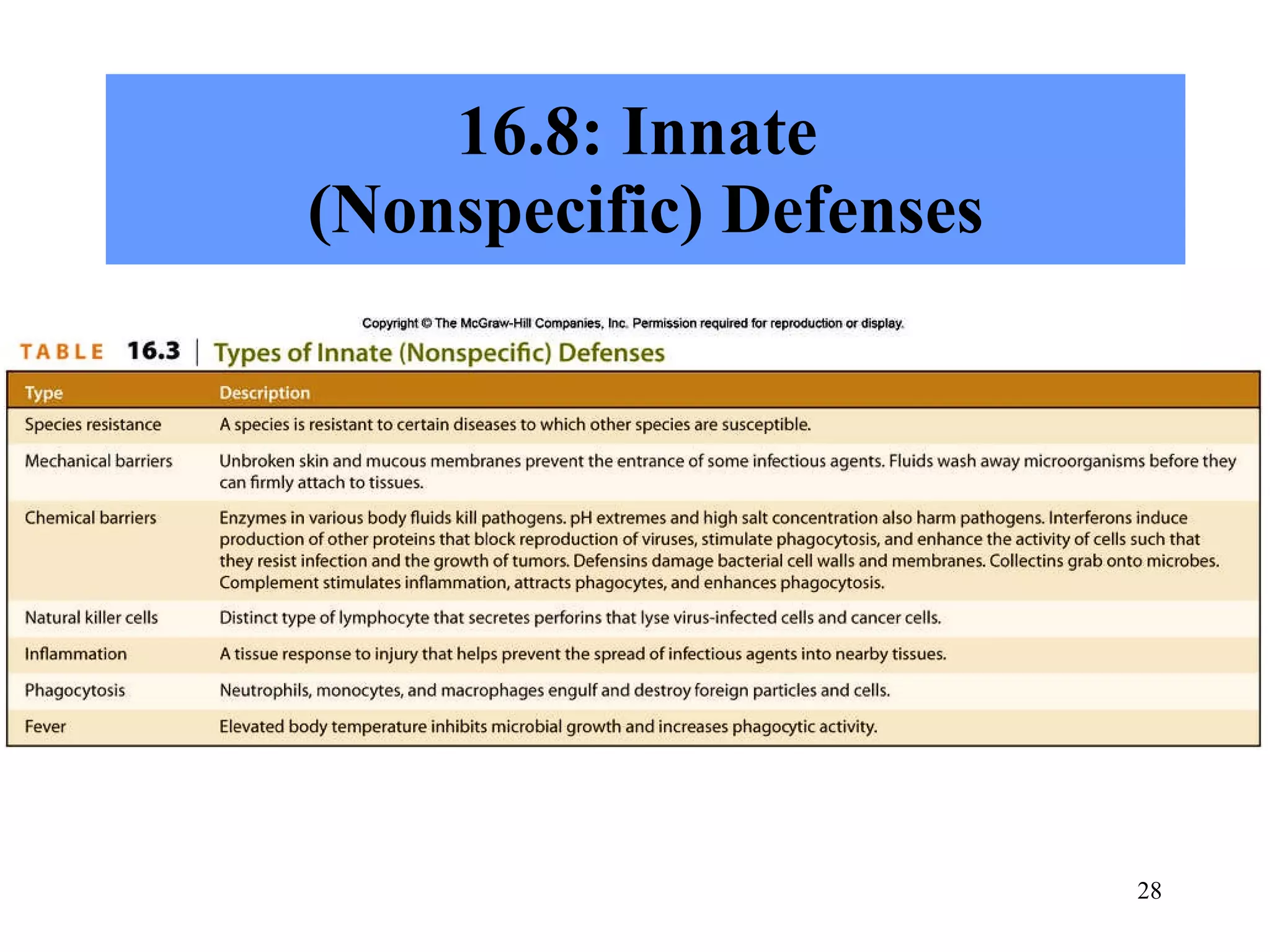
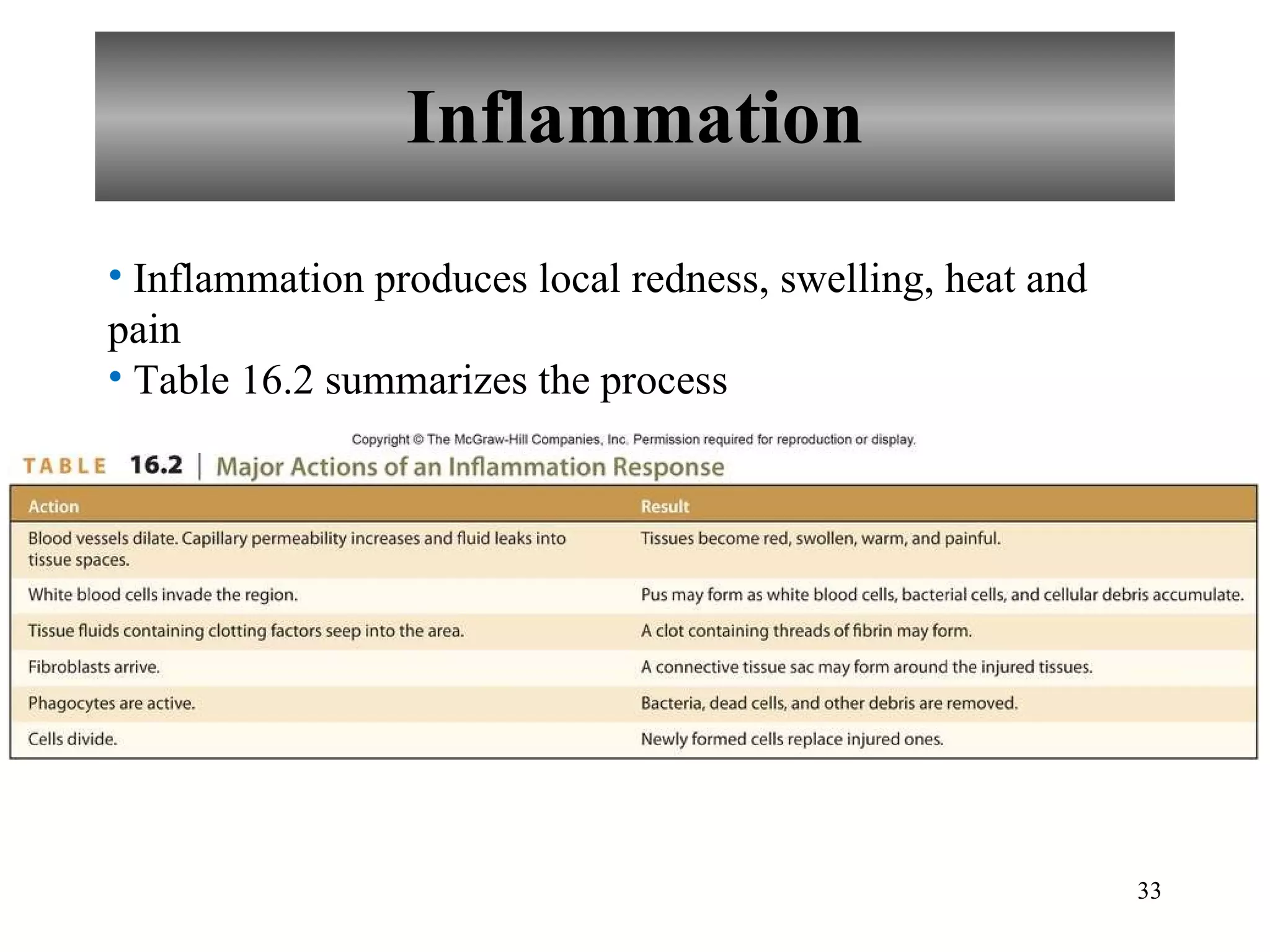
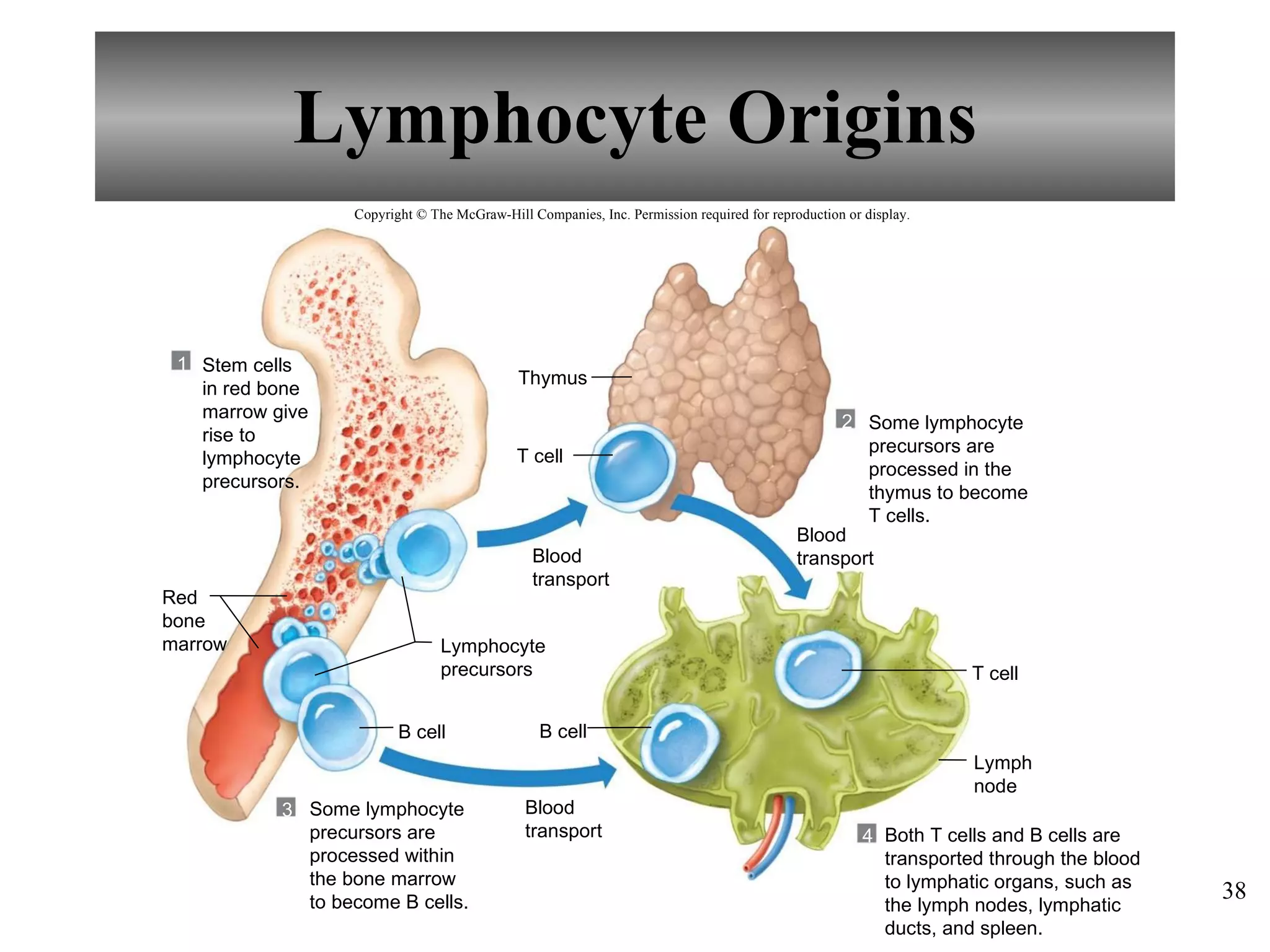
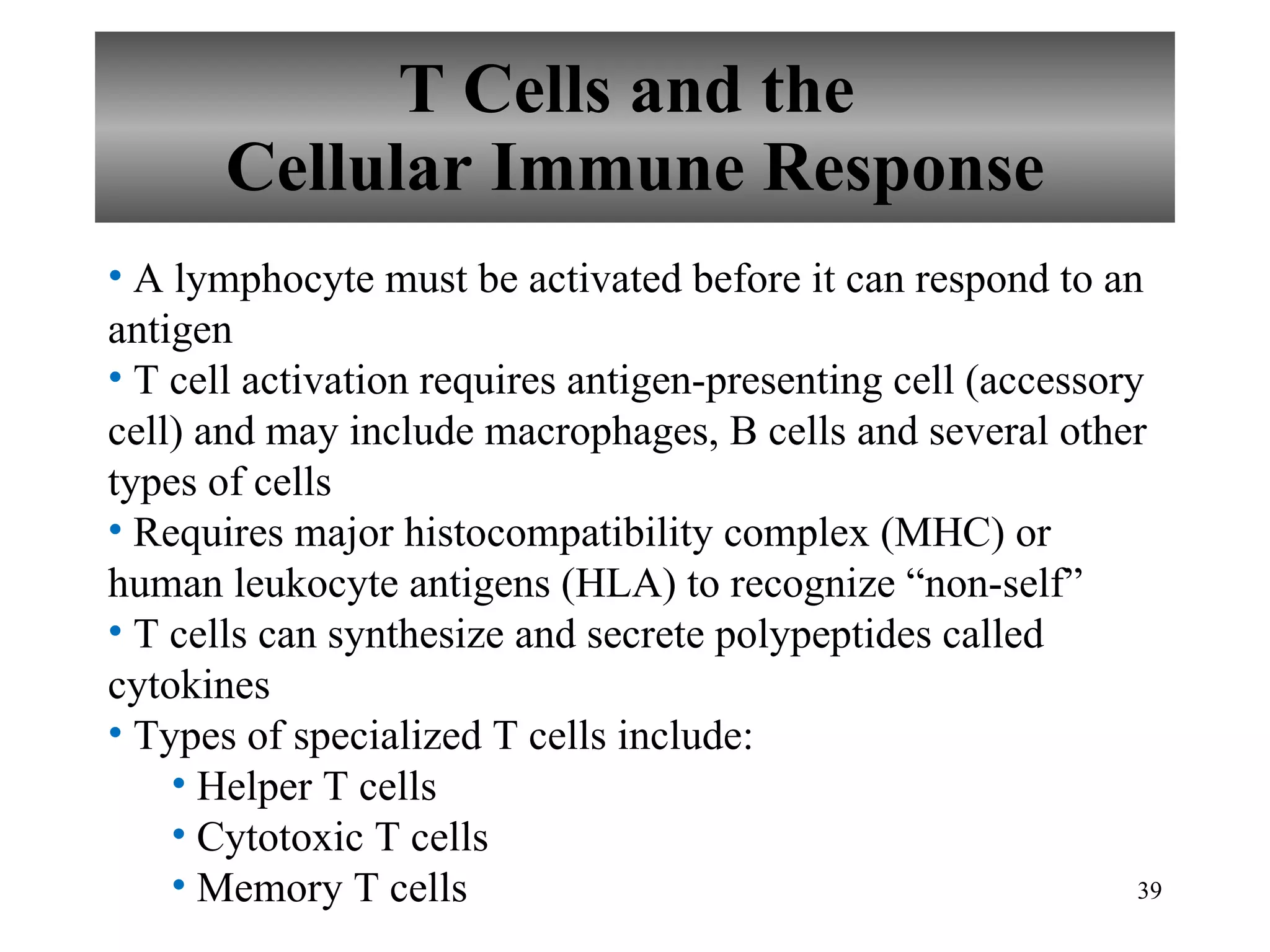
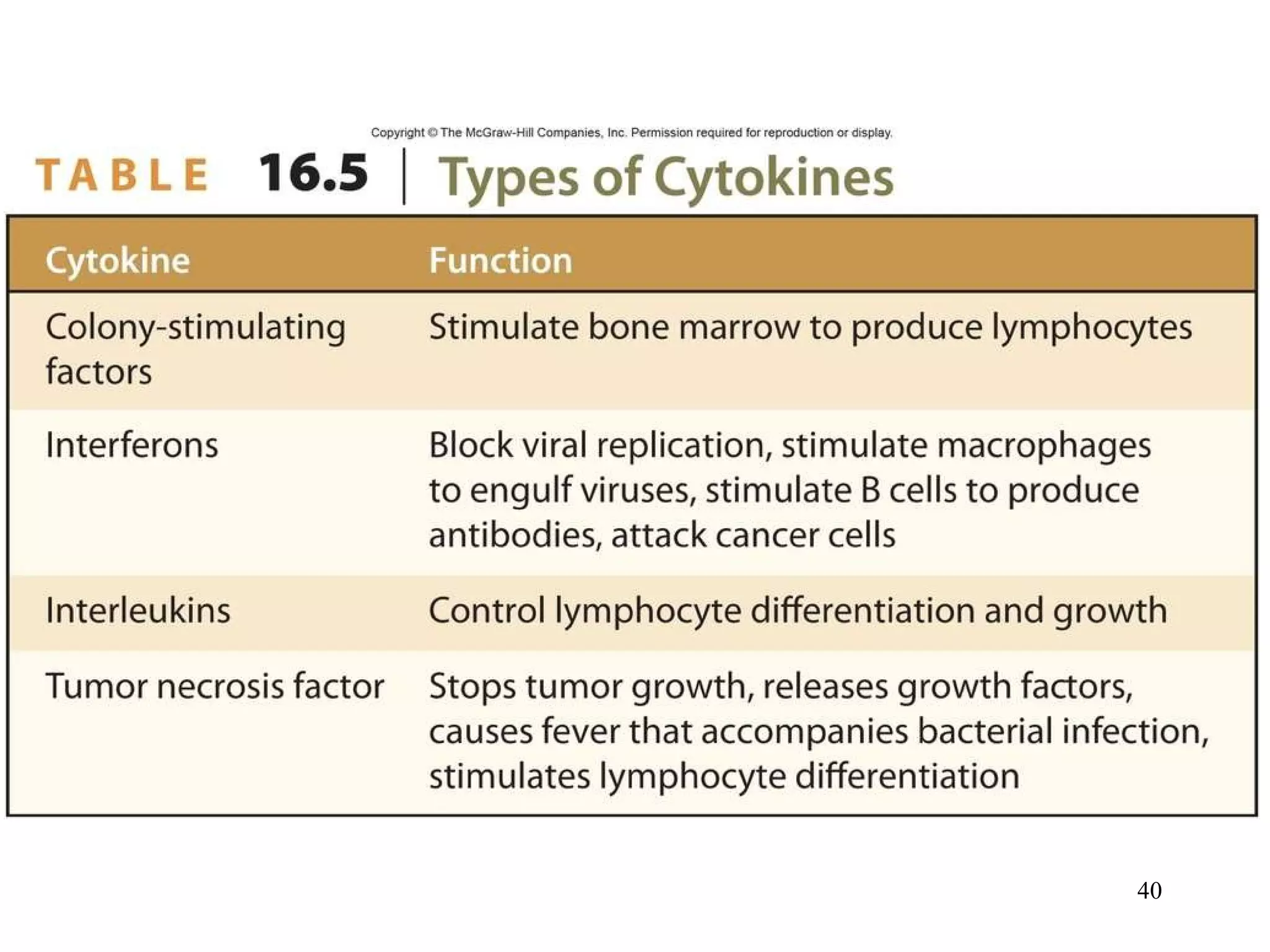
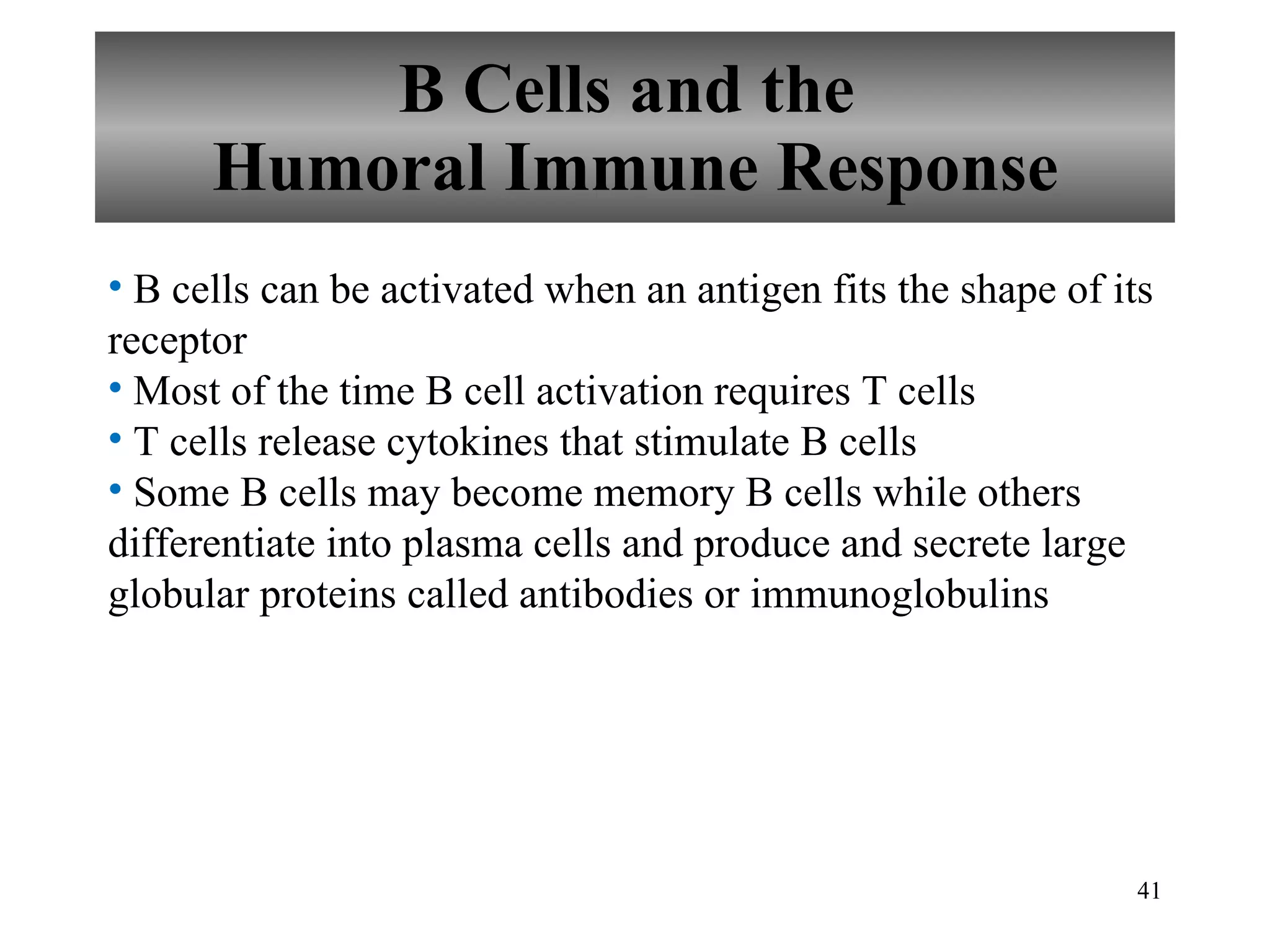
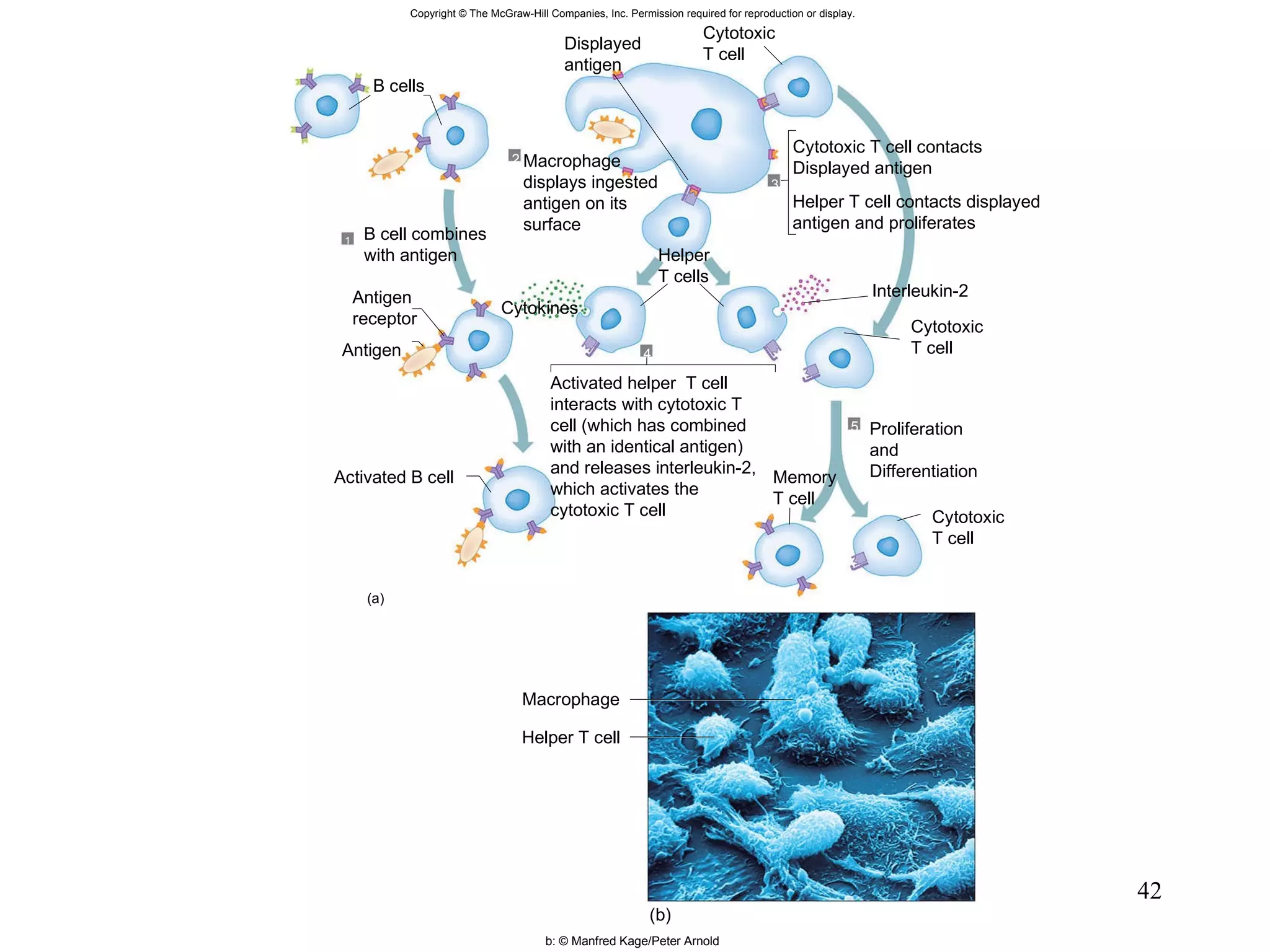
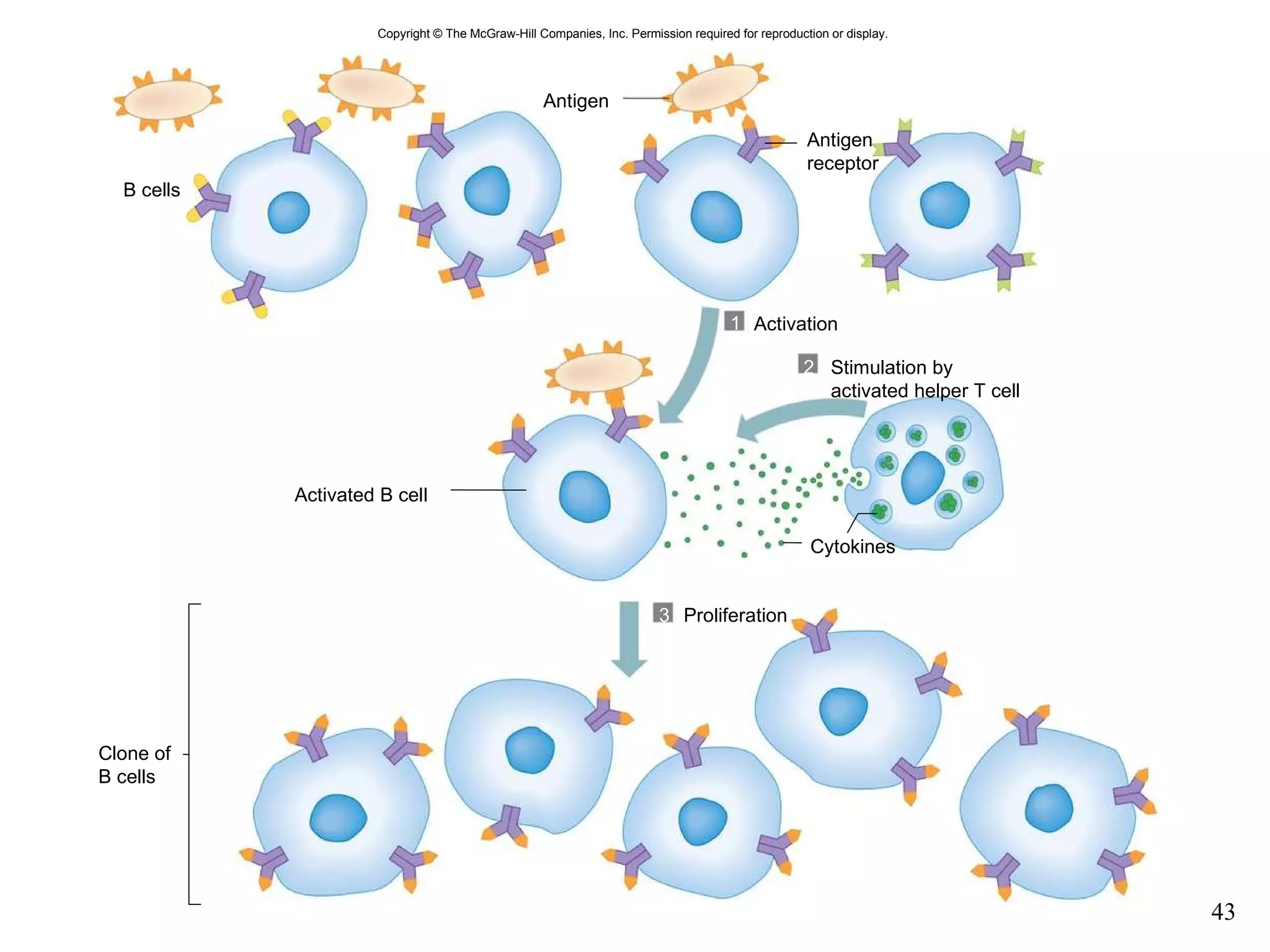
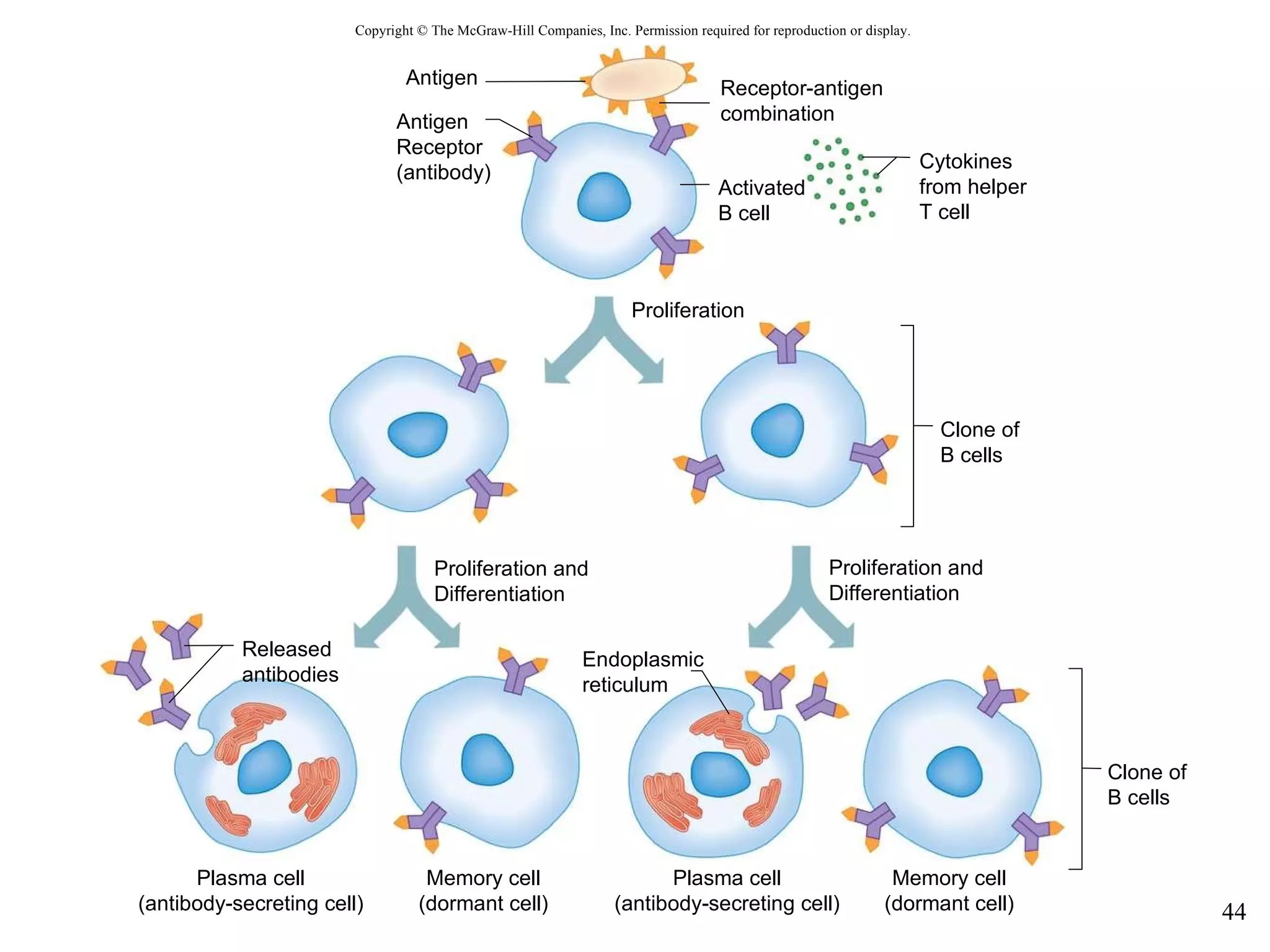
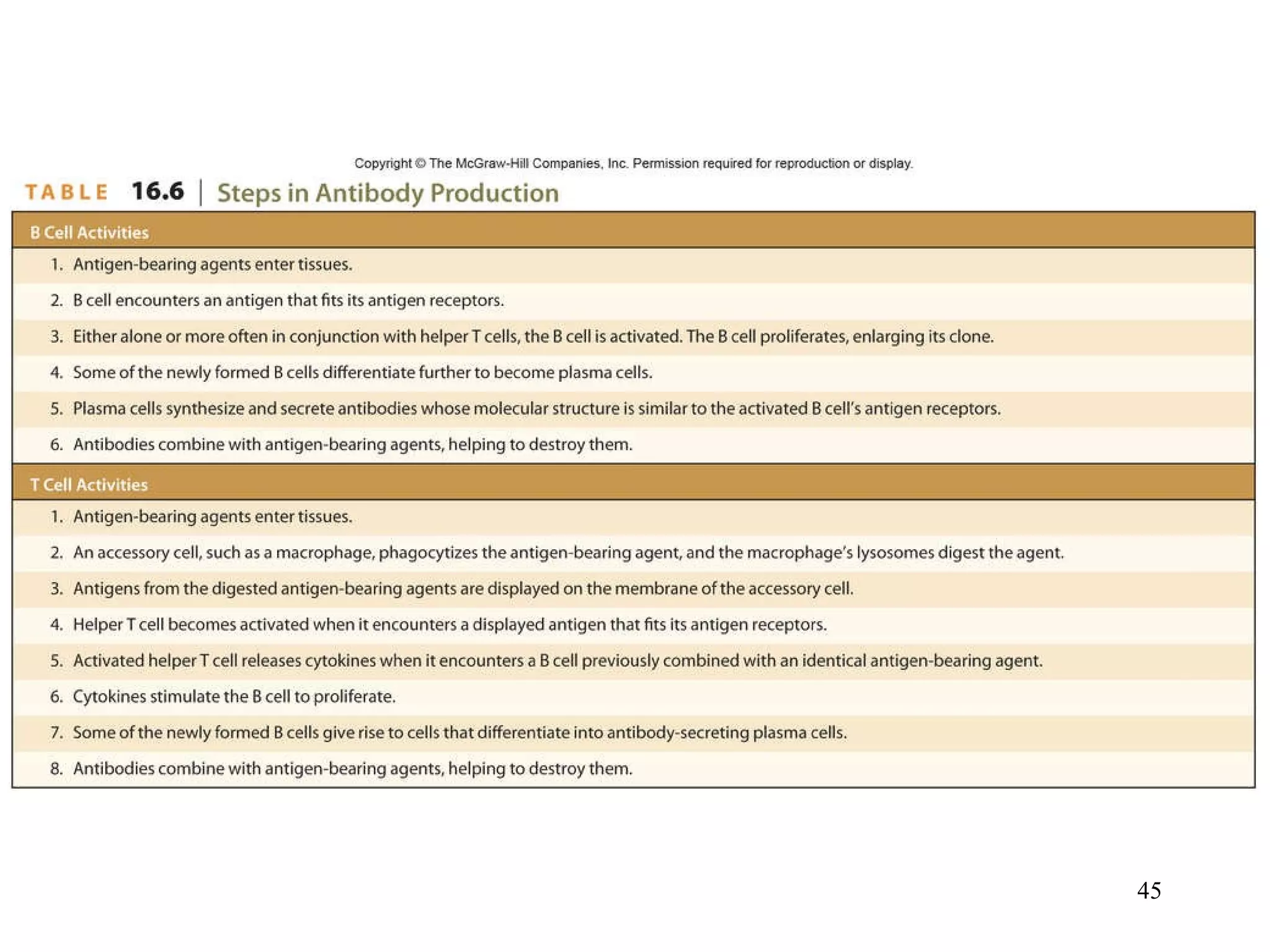
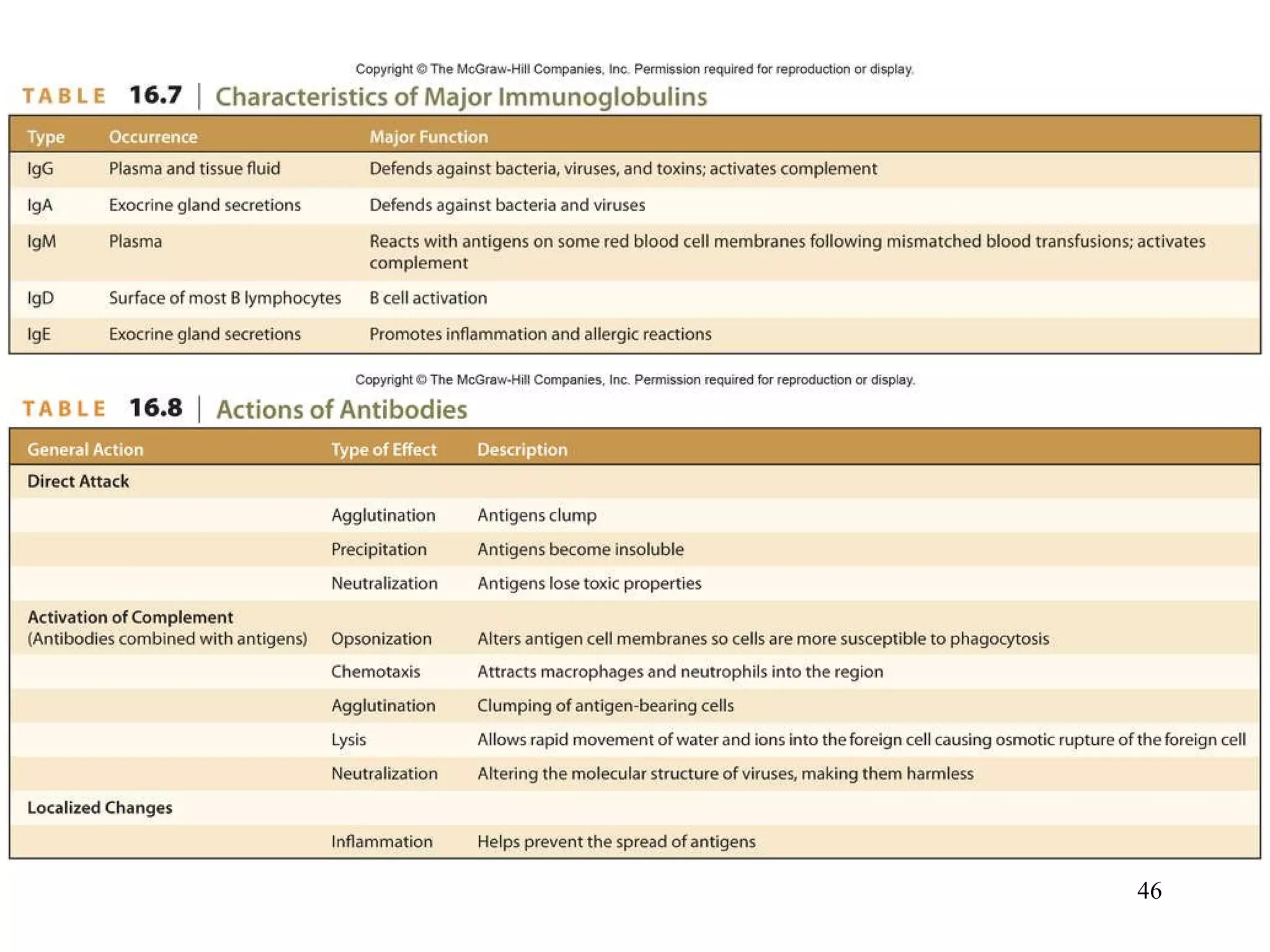
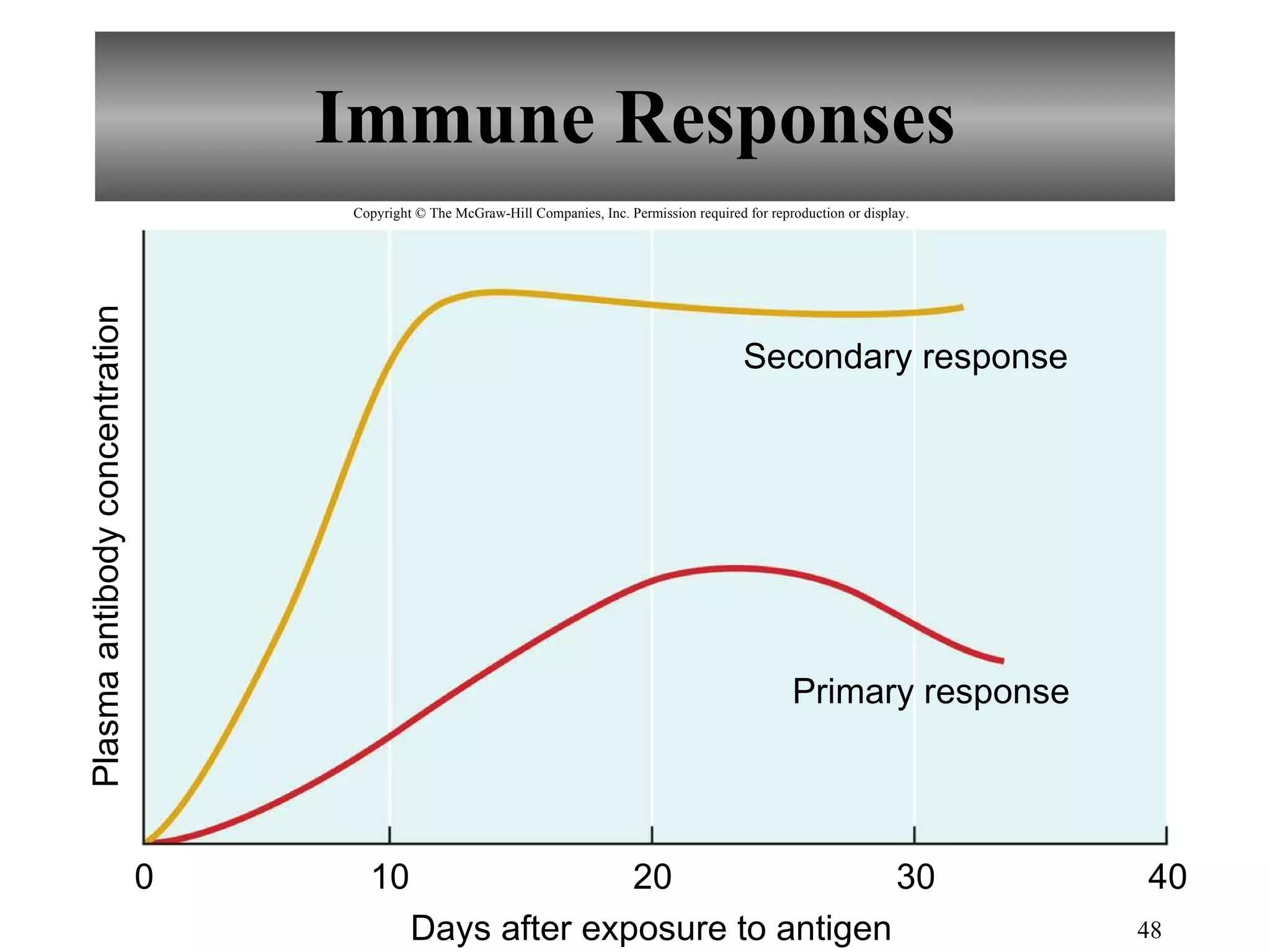
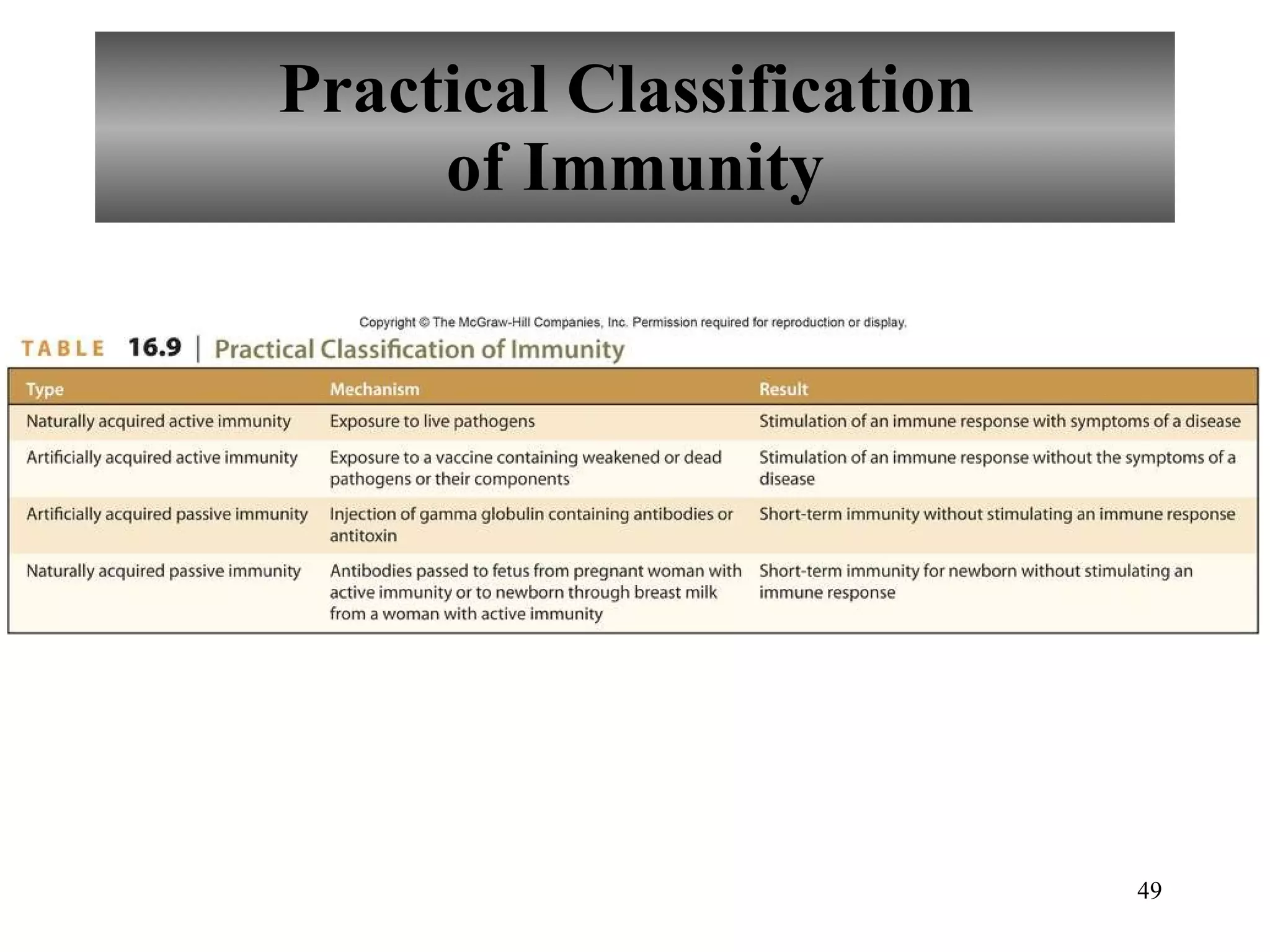
The document provides an overview of the lymphatic system and immunity from Chapter 16 of Hole's Human Anatomy and Physiology textbook. It discusses the key components and functions of the lymphatic system including lymphatic vessels, lymph nodes, lymph fluid formation and flow, and immune defenses. The summary highlights that the lymphatic system transports excess fluid, transports fats, and helps defend the body against disease. It also distinguishes between innate nonspecific defenses and adaptive specific defenses of the immune system.
![2402 Anatomy and Physiology II Chapter 16 Susan Gossett [email_address] Department of Biology Paris Junior College](https://image.slidesharecdn.com/chapter16-lymphaticsystemandimmunity-110728070145-phpapp01/75/Chapter-16-Lymphatic-System-and-Immunity-2-2048.jpg)