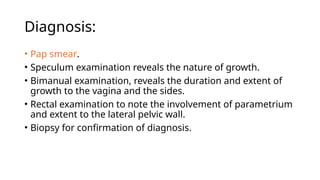
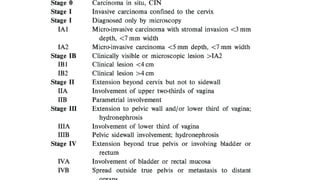
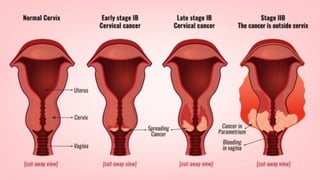
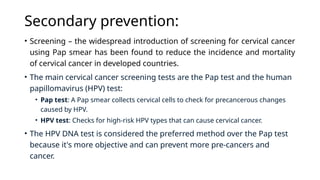
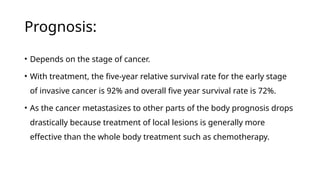
Cervical cancer develops in the cervix and is the fourth most common cancer among women, with about 660,000 diagnosed and 350,000 deaths globally in 2022, primarily linked to HPV infection. It is prevalent in developing countries, with various risk factors and symptoms including irregular bleeding and pelvic pain. Diagnosis relies on Pap smears and biopsies, while management includes primary prevention strategies, screening, and treatments like surgery and chemotherapy, with prognosis significantly depending on the cancer stage.