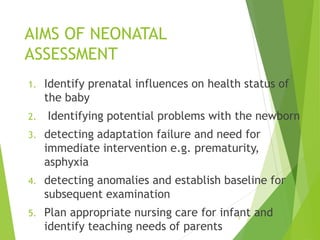
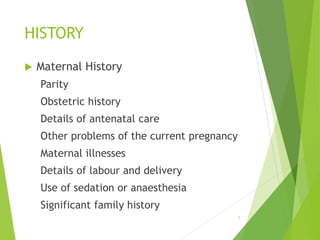
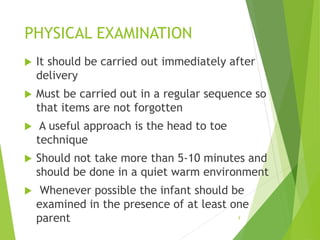
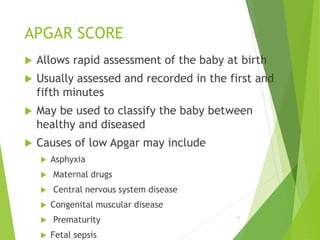
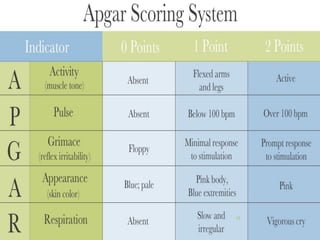
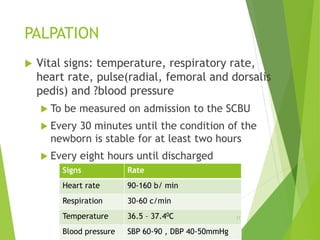
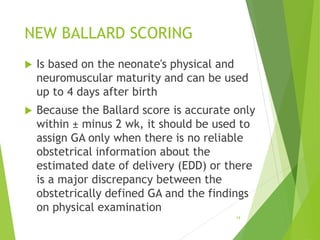
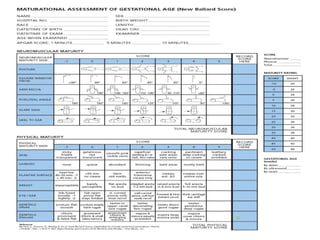
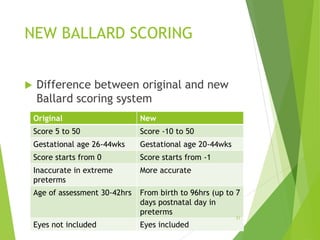
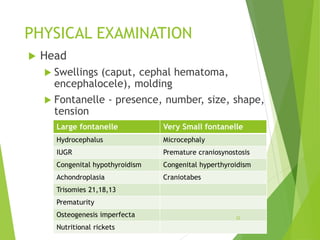
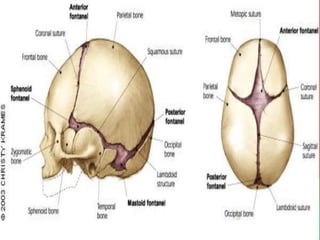
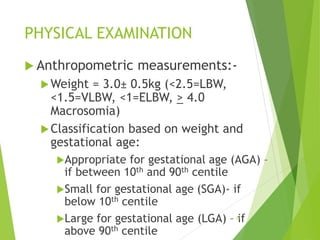
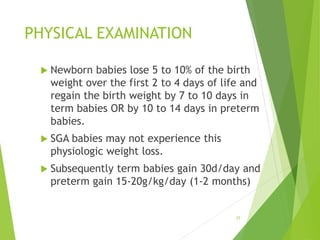
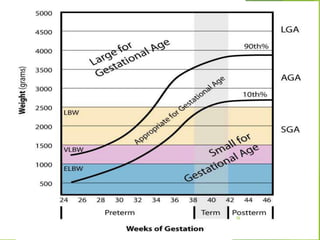
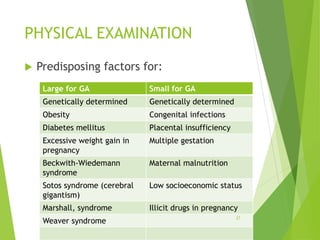
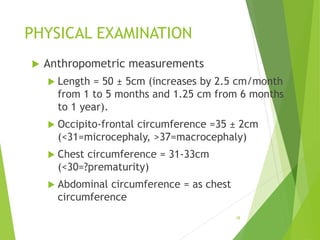
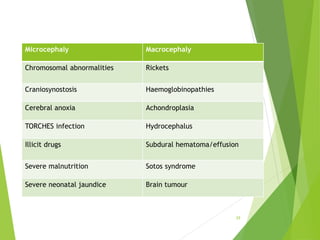
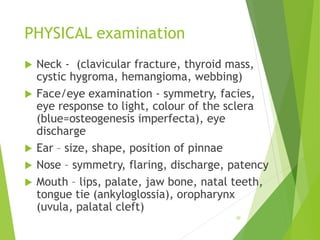
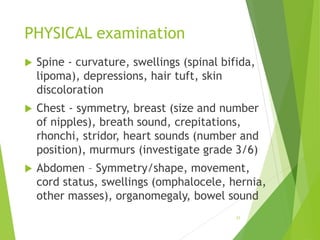
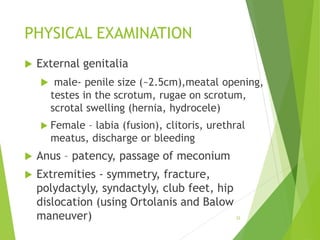
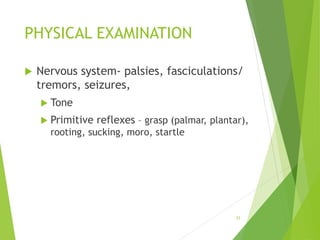
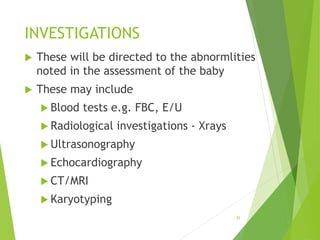
This document outlines the components and process of neonatal assessment. It discusses the aims of assessment including identifying prenatal influences, potential problems, and needs for intervention. The components include history of the mother and baby, physical examination from head to toe, and potential investigations. The physical examination involves assessing vital signs, appearance, measurements, and neurological and physical systems. The goal is to detect any issues that may impact health and develop appropriate care plans.