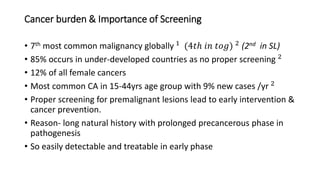
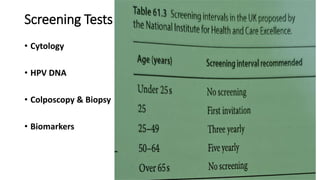
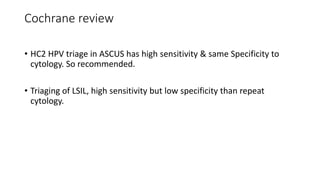
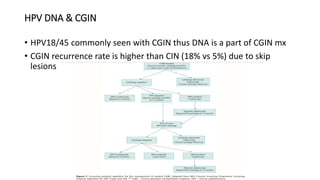
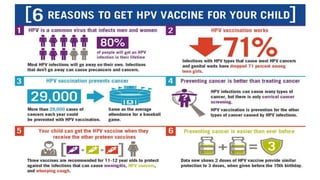
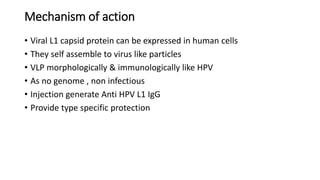
Persistent infection with certain high-risk HPV types is the main risk factor for cervical cancer. Screening through cervical smears and HPV testing can detect pre-cancerous lesions early, leading to treatment and prevention of invasive cancer. The HPV vaccine protects against HPV types 16 and 18, which cause approximately 75% of cervical cancers. While HPV infection is common, only a small portion progresses to cancer, so screening remains important to detect the minority of cases that may develop despite vaccination.