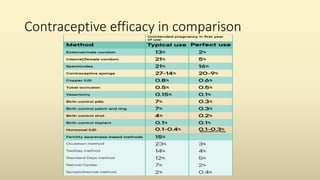
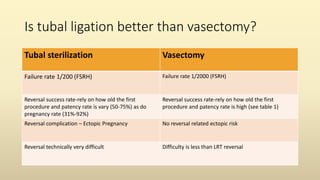
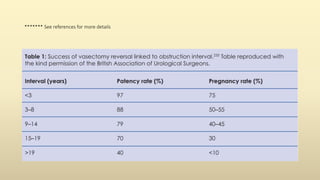
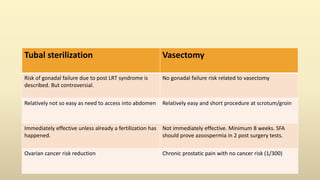
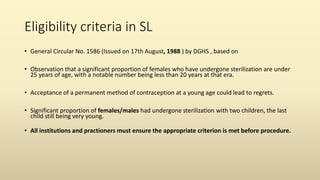
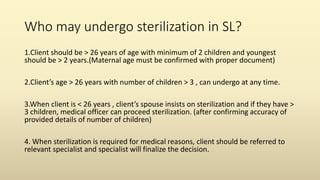
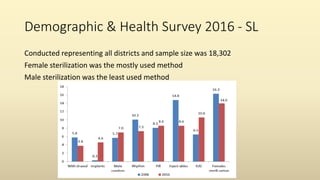
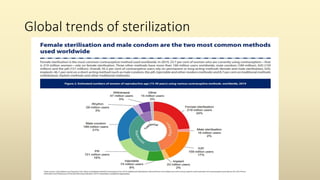
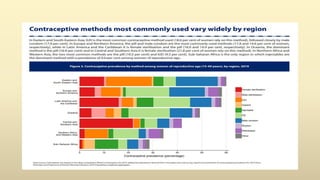
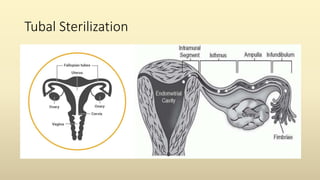
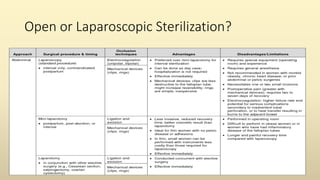
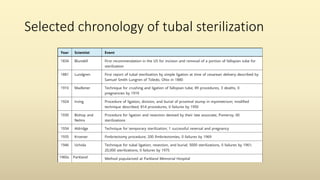
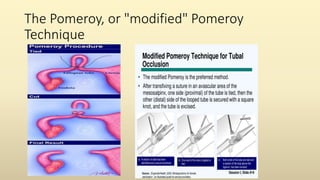
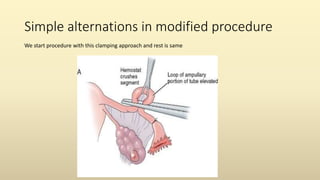
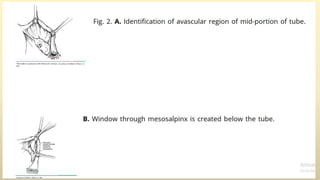
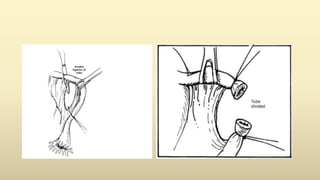
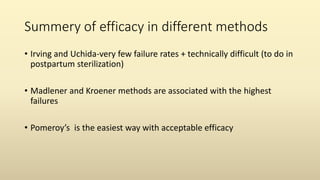
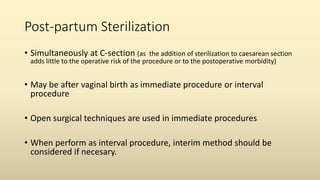
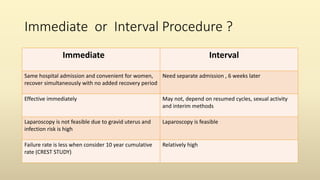
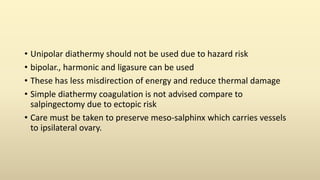
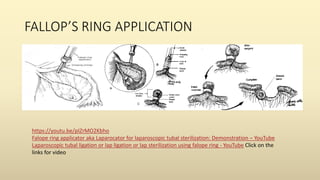
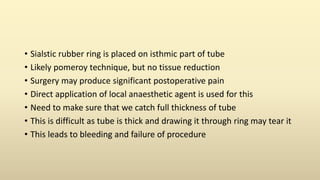
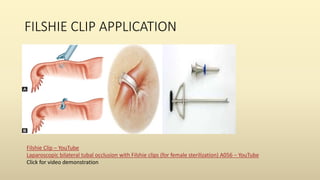
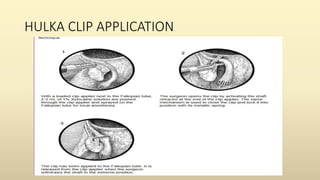
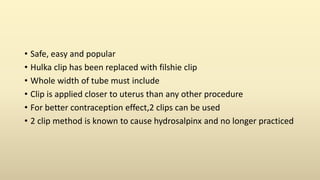
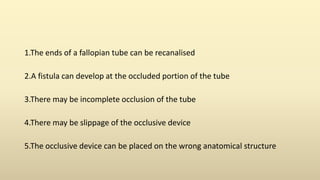
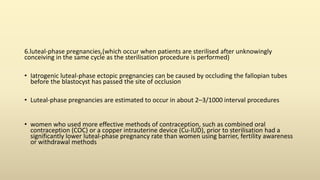
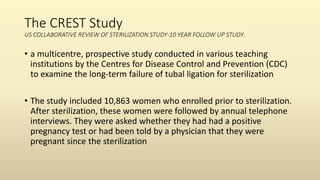
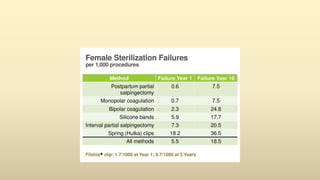
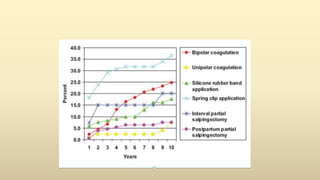
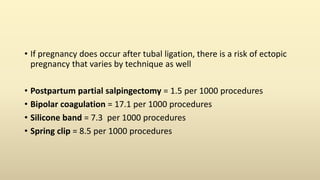
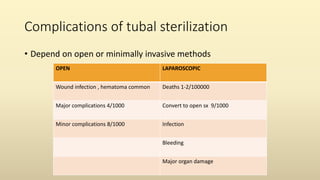
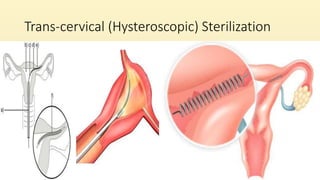
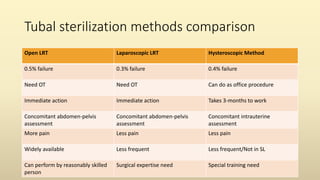
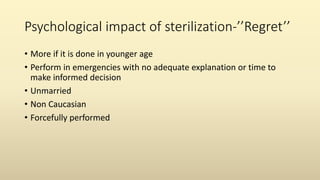
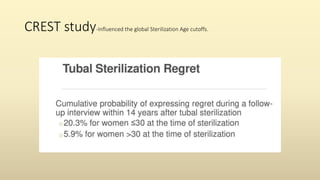
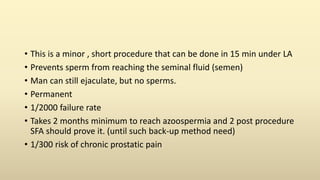
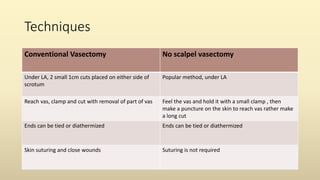
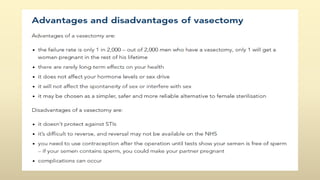
The document provides an in-depth discussion on permanent sterilization, particularly focusing on various surgical techniques for both male and female sterilization, their efficacy, and failure rates. It also highlights the eligibility criteria for sterilization in Sri Lanka, the psychological impacts of the procedures, and the comparative risks and benefits associated with different methods. Additionally, the document outlines the complications, demographic data, and current practices in the context of sterilization.