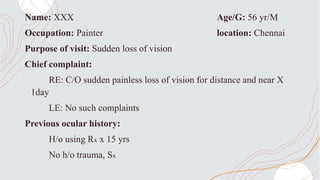
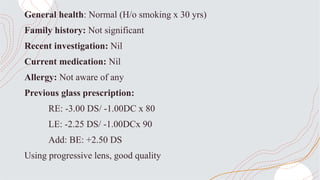
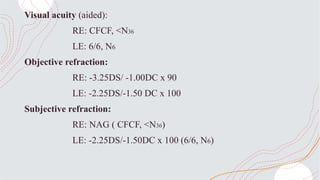
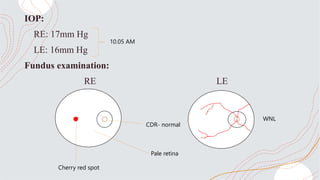
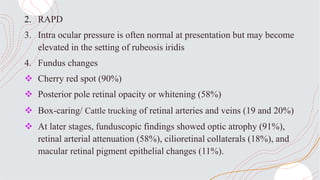
1. A 56-year-old male painter presented with sudden painless loss of vision in the right eye for 1 day. Examination found right eye visual acuity of counting fingers close to face and a cherry red spot on fundus examination, consistent with a diagnosis of central retinal artery occlusion.
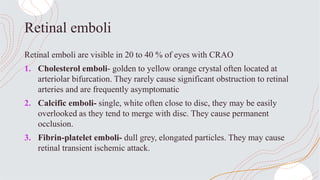
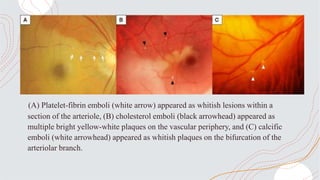
2. Central retinal artery occlusion is caused by an embolism or thrombosis blocking the central retinal artery, cutting off blood supply to the retina. It typically causes sudden monocular vision loss and is more common in older males with risk factors like hypertension and smoking.
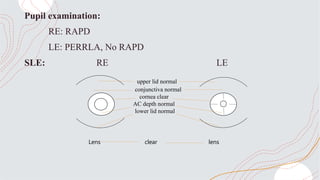
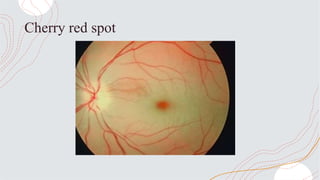
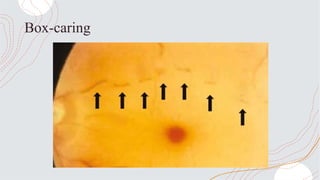
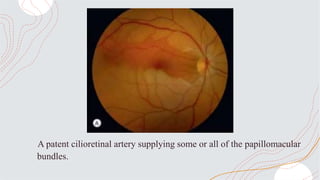
3. On examination, central retinal artery occlusion presents with right eye relative afferent pupillary defect, cherry red spot on the retina, and box