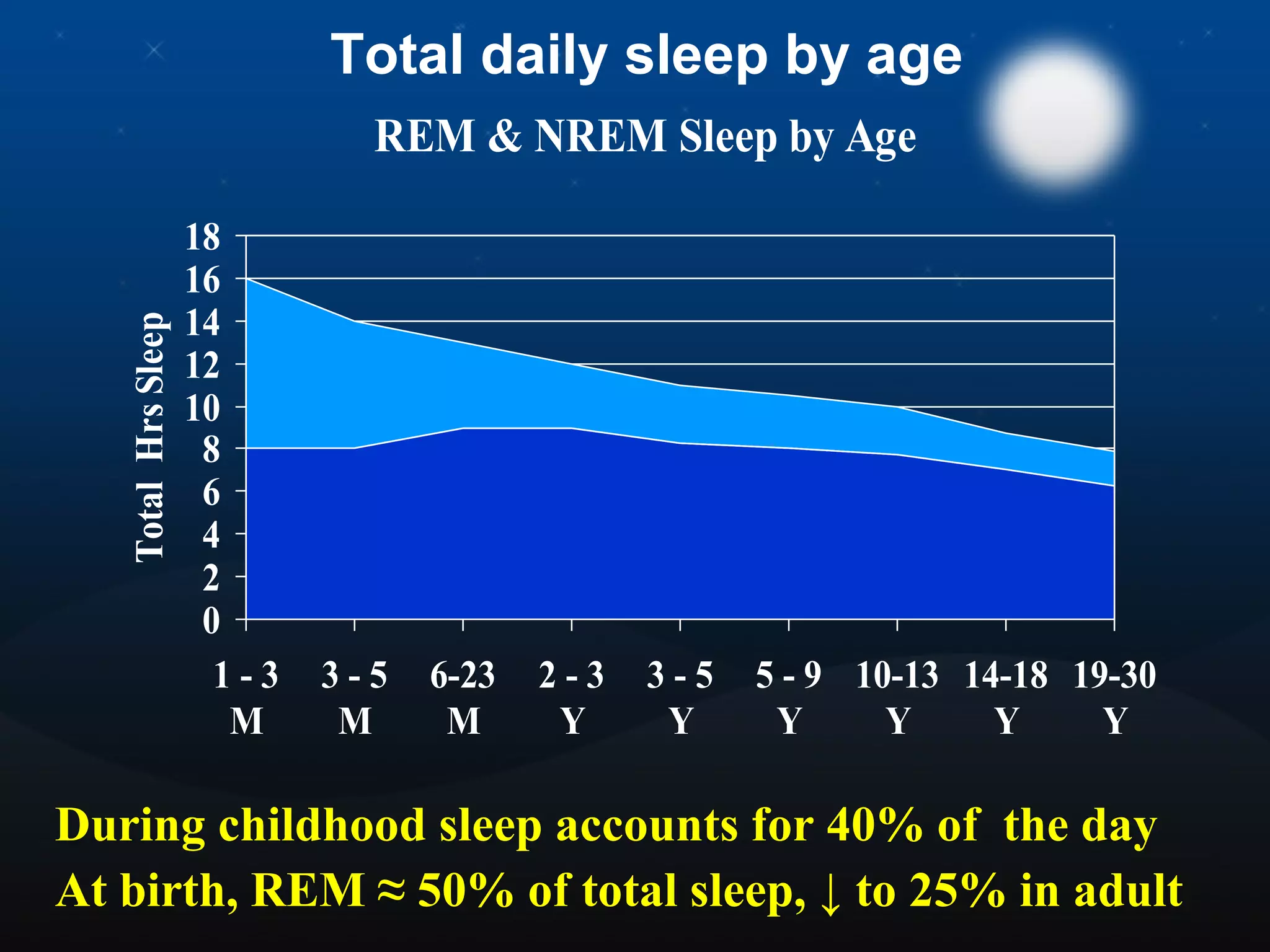
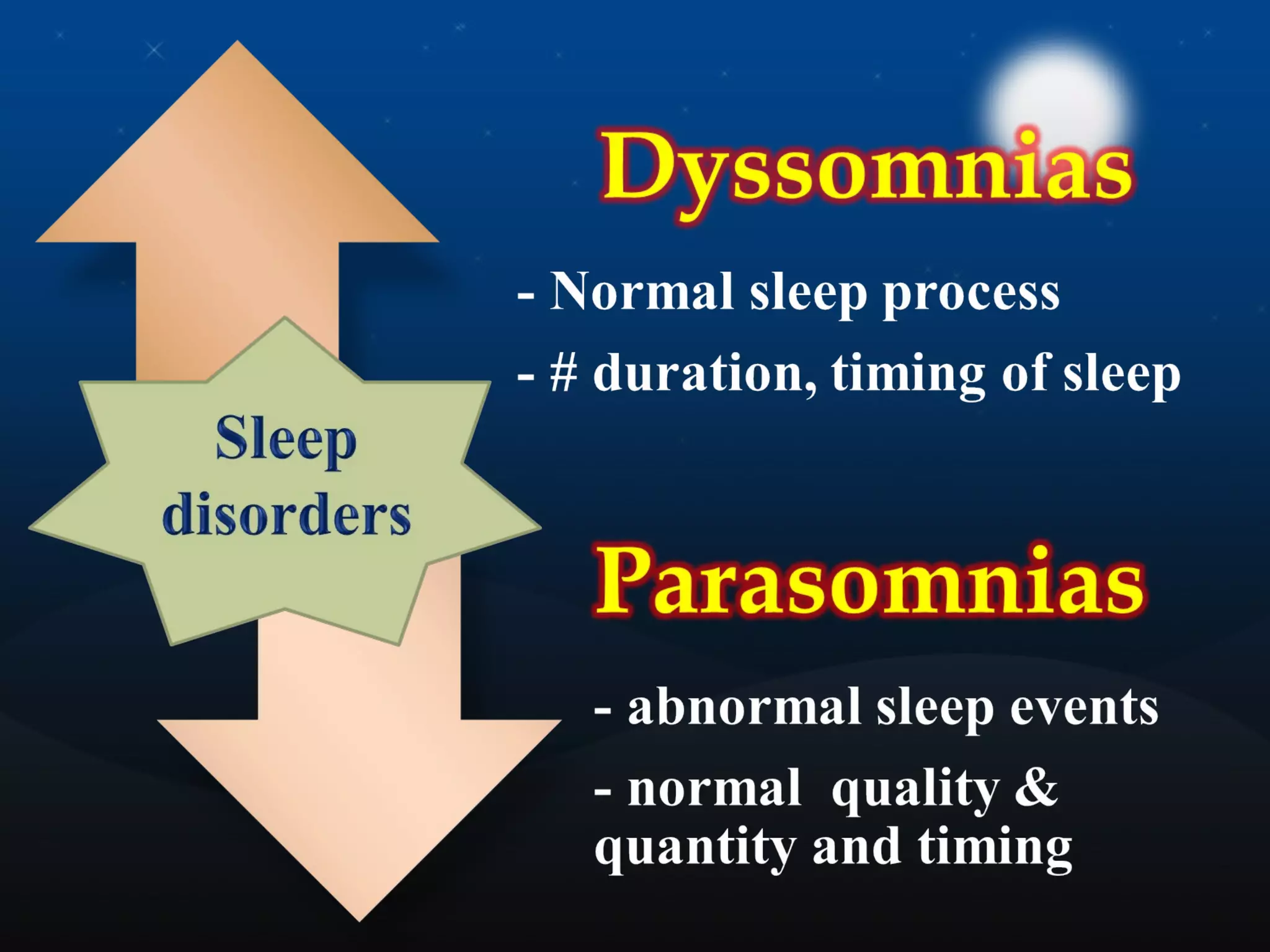
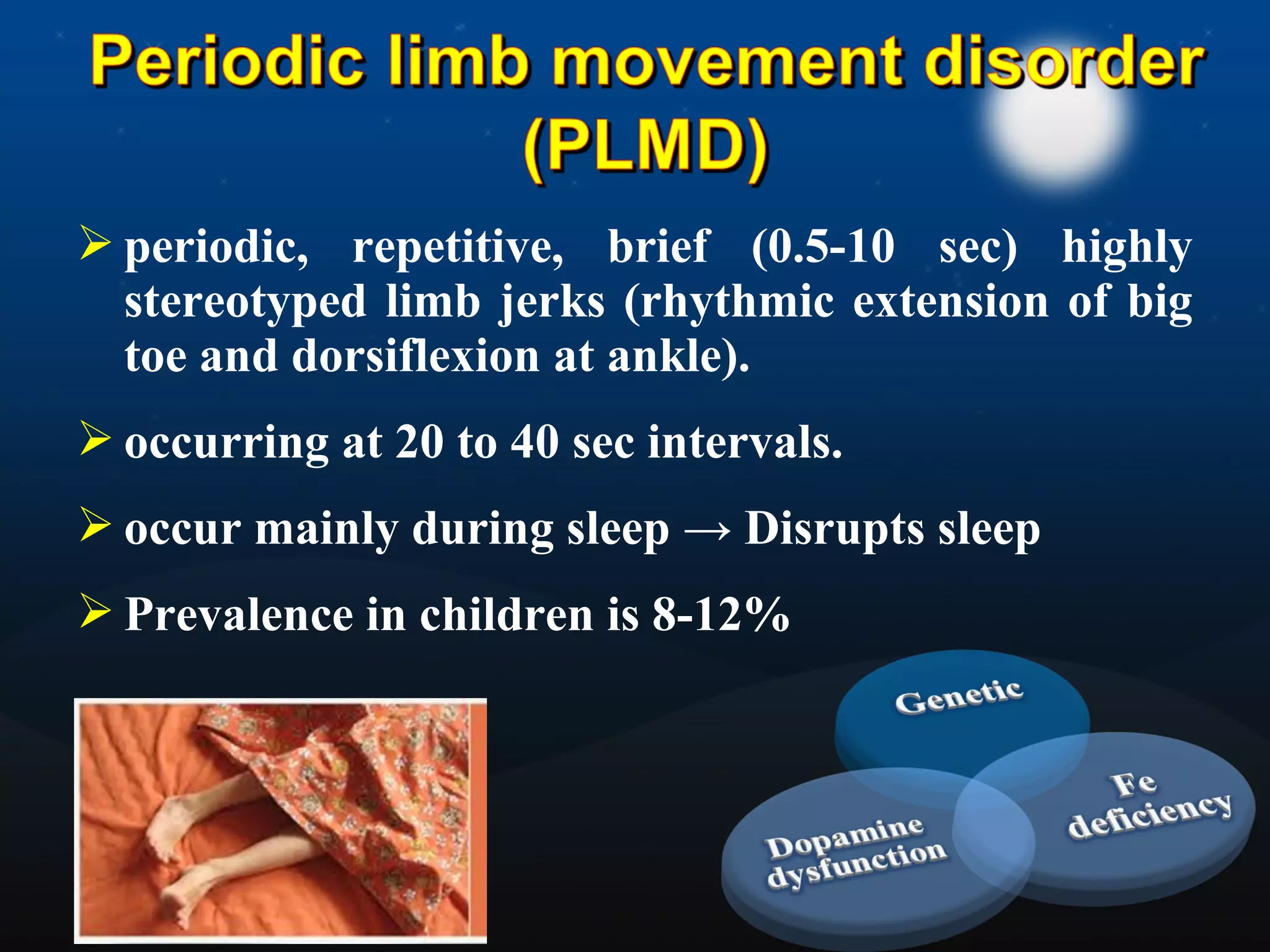
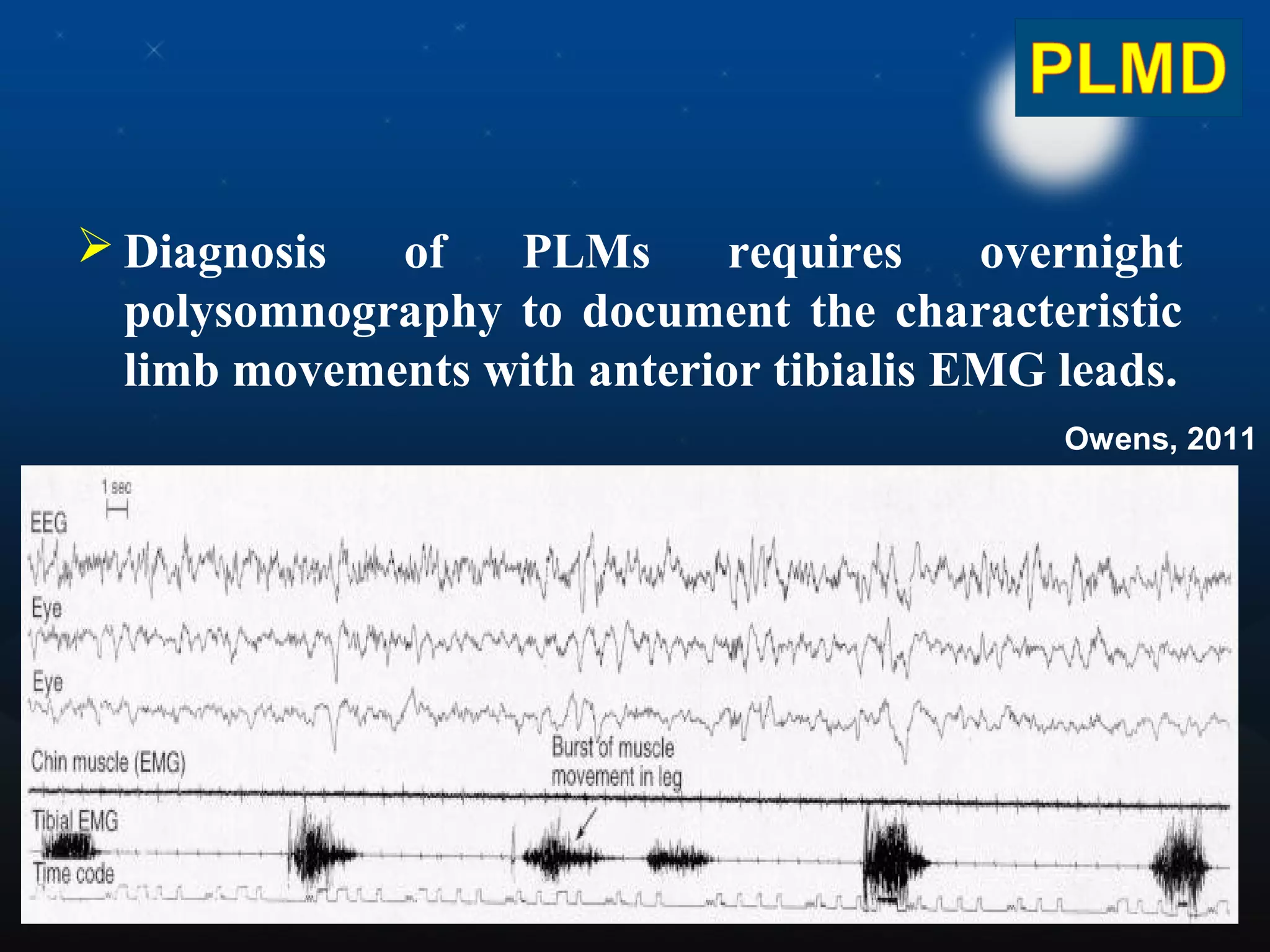
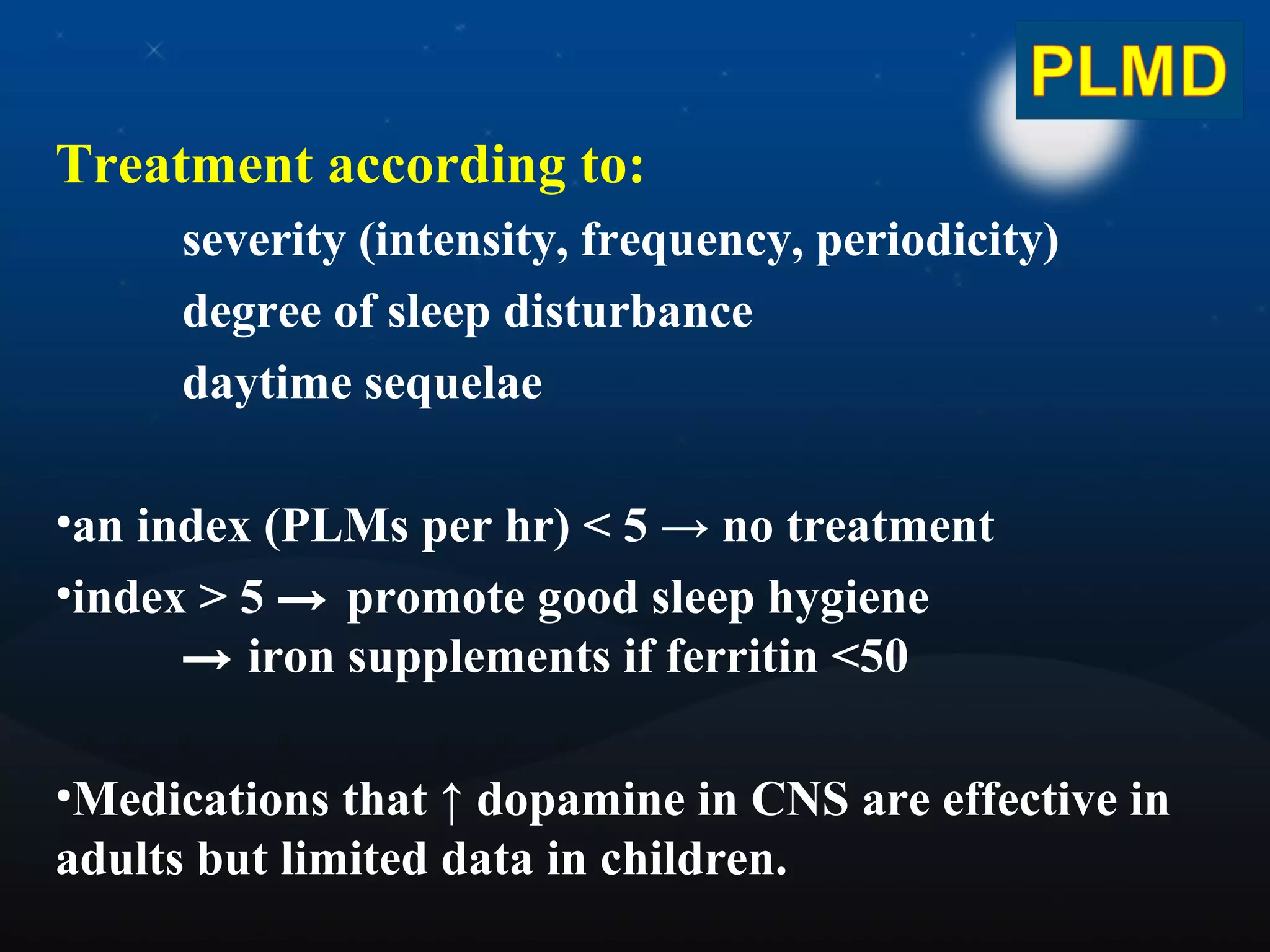
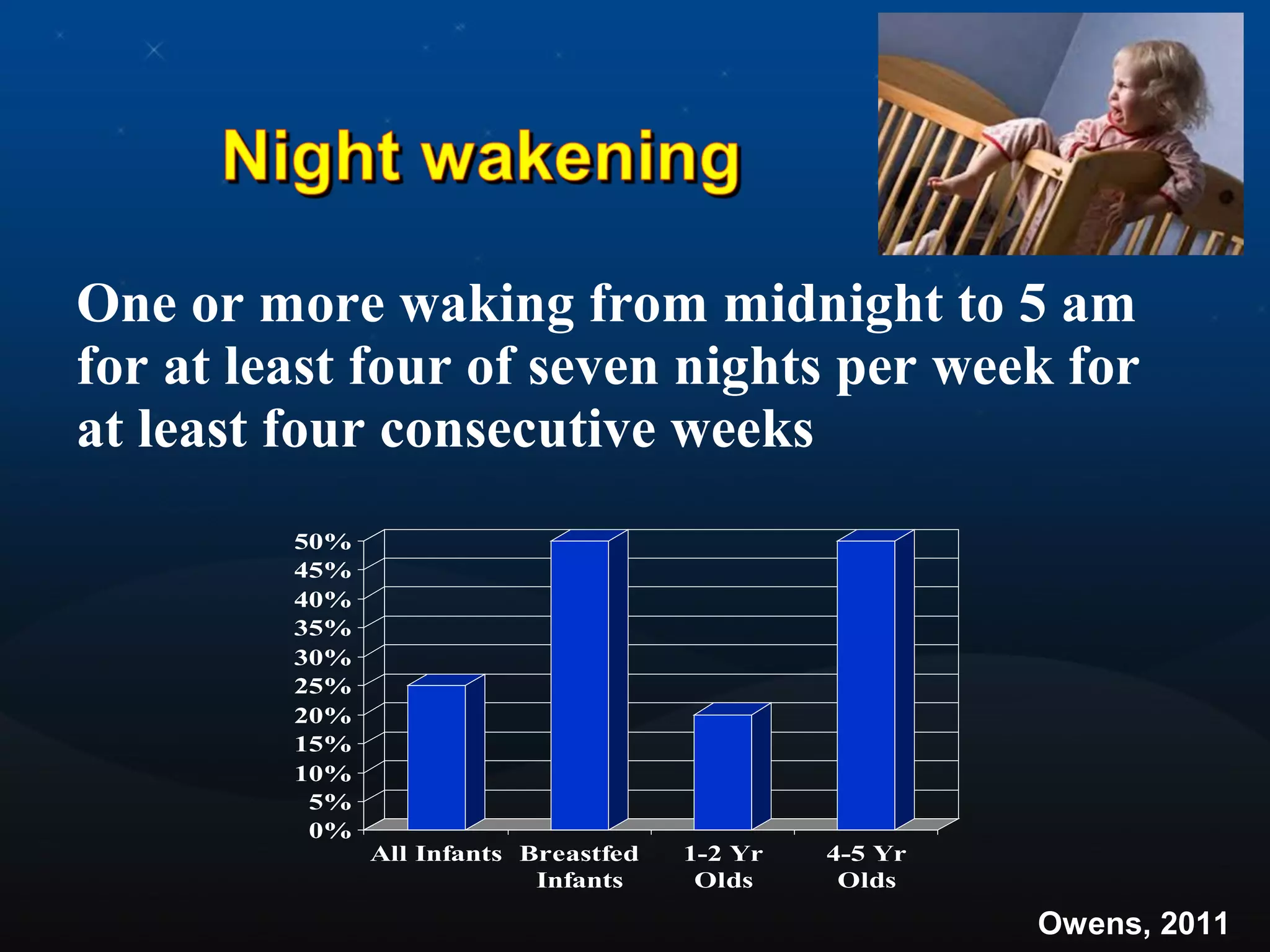
This document discusses pediatric sleep disorders. It begins by outlining the objectives of understanding normal sleep patterns in children, reviewing common sleep disorders, and discussing treatment options. It then covers topics like sleep cycles, how children's sleep differs from adults, prevalence of various sleep disorders in children, and classification of sleep disorders into dyssomnias, parasomnias, and medical/psychiatric disorders. Specific disorders like insomnia, hypersomnia, sleep apnea, narcolepsy, restless leg syndrome, and parasomnias are explained. Treatment options for each disorder focus on behavioral interventions and medication if needed. Proper sleep hygiene practices to promote healthy sleep in children are also outlined.