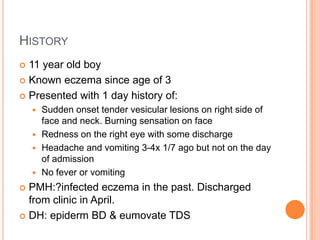
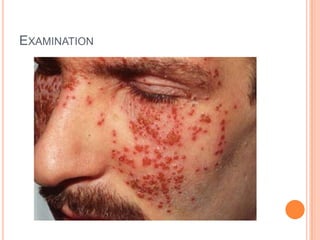
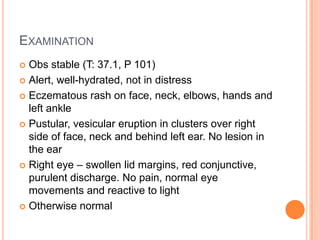
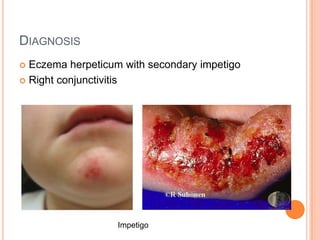
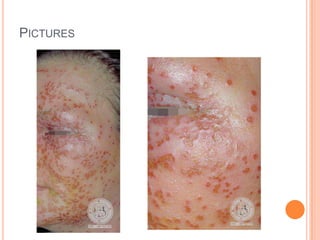
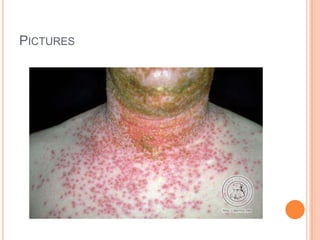
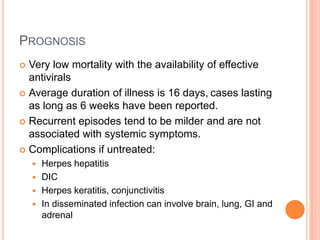
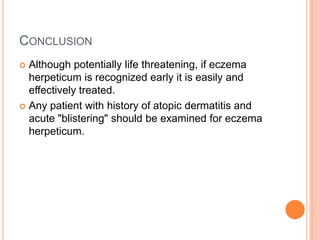
A 11-year-old boy presented with sudden onset tender vesicular lesions on his face and neck, accompanied by redness and discharge from his right eye. He has a history of eczema since age 3. Examination found eczematous rashes with pustular and vesicular eruptions on his face and neck. He was diagnosed with eczema herpeticum with secondary impetigo and conjunctivitis. Treatment included antiviral and antibiotic medications, with referral to dermatology and ophthalmology. Eczema herpeticum is an acute herpes simplex infection in patients with atopic dermatitis that requires prompt treatment to prevent complications.

![REFERENCES
Royal college of paediatrics and child health allergy care
pathways for children eczema
Aronson PL, Yan AC, Mittal MK, Mohamad Z, Shah
SS Delayed acyclovir and outcomes of children hospitalized
with eczema herpeticum. [Journal Article, Multicenter Study,
Research Support, N.I.H., Extramural, Research Support,
Non-U.S. Gov't]
Pediatrics 2011 Dec; 128(6):1161-7.
Brook, I., Frazier, E.H., & Yeager, J.K. (1998). Microbiology of
infected eczema herpeticum. Journal of the Academy of
Dermatology, 38, 627-629.
Sais, G., Jucgla, A., Curco, N., & Peyri, J. (1994). Kaposi's
varicelliform eruption with ocular involvement. Archives of
Dermatology, 130, 1209-1210
CG57 Atopic eczema in children: NICE guideline
Mooney MA, Janniger CK, Schwartz RA. Kaposi's
varicelliform eruption. Cutis. 1994;53:243-245.](https://image.slidesharecdn.com/casepresentationeczemaherpeticum-120215170425-phpapp02/85/Case-presentation-eczema-herpeticum-21-320.jpg)