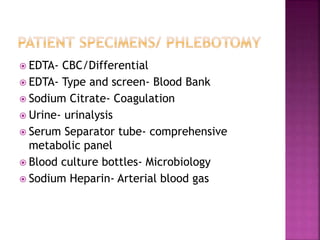
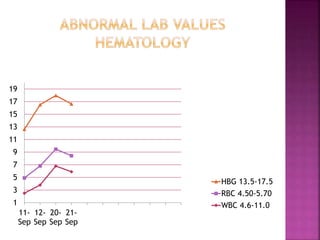
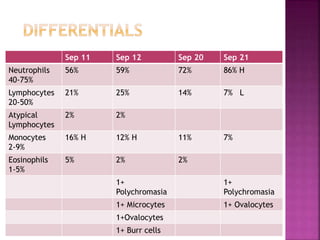
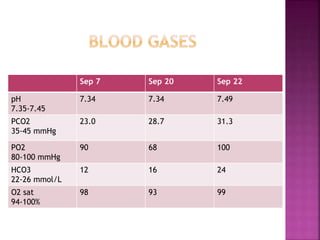
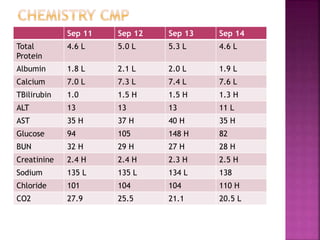
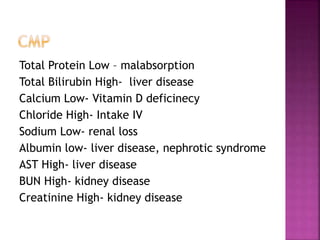
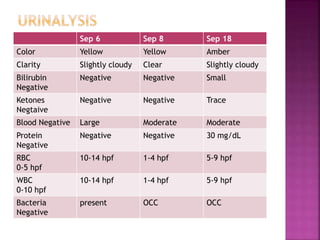
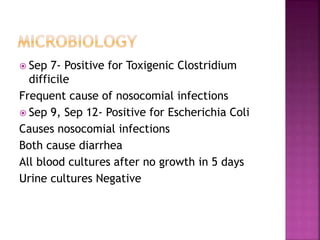
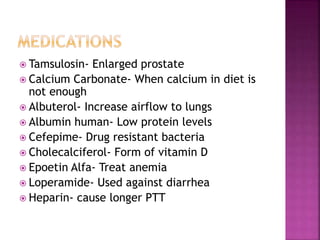
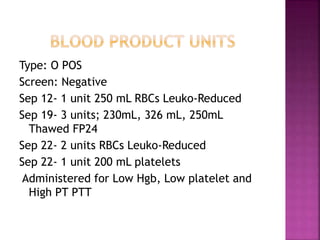
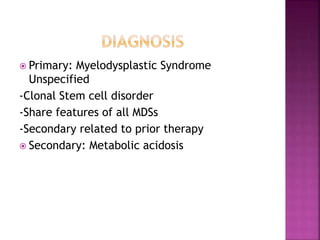
An 86-year-old male presented to the emergency room with dizziness and was admitted to the ICU for dehydration. Medical workup showed malignant neoplasms, hypovolemia, pancytopenia, and a bloodstream infection. Laboratory results indicated anemia, thrombocytopenia, and abnormalities consistent with liver and kidney disease. Stool and blood cultures grew Clostridium difficile and Escherichia coli. The patient was diagnosed with myelodysplastic syndrome and received multiple blood transfusions.