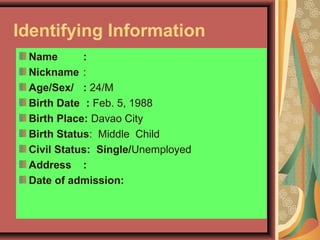
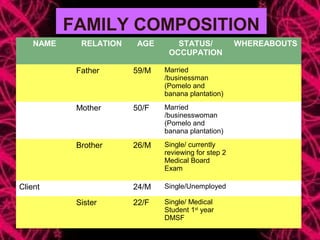
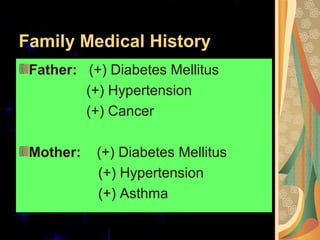
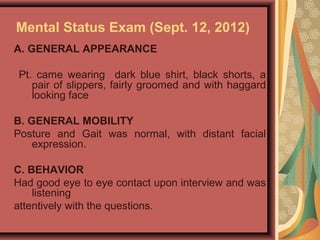
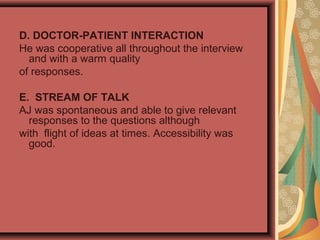
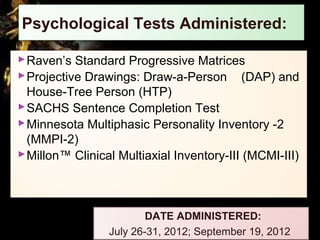
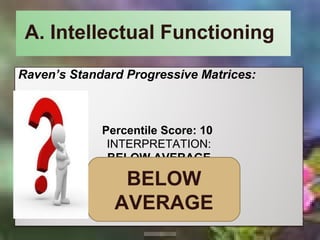
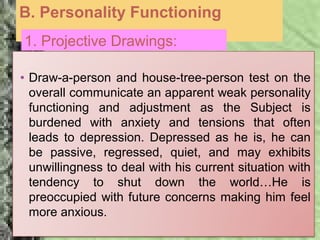
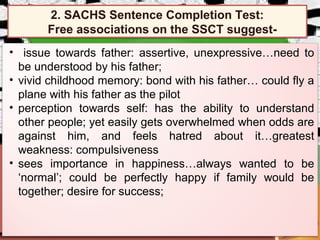
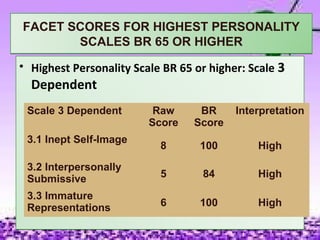
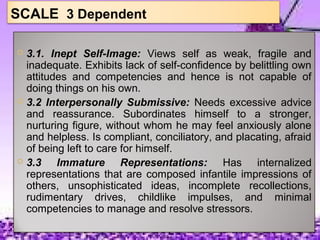
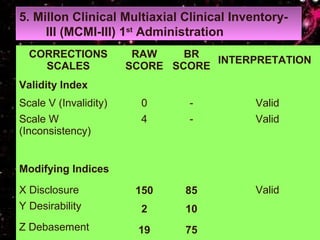
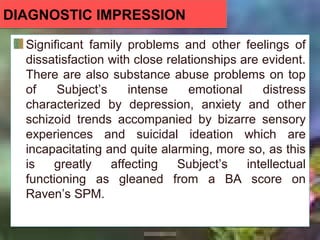
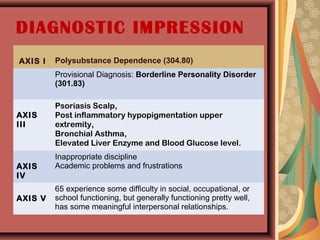
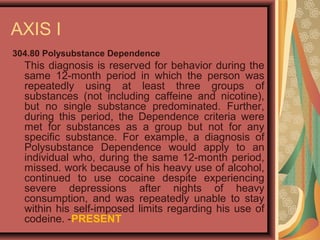
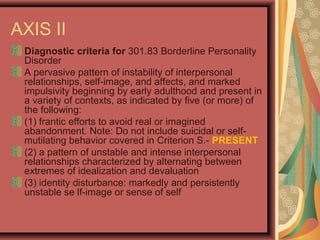
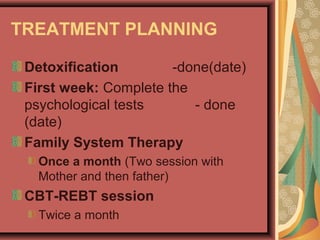
The case presentation summarizes a 24-year-old male client who was readmitted for treatment. Psychological tests revealed below average intellectual functioning and signs of anxiety, depression, and dependence. The client has a history of substance abuse and suicidal ideation. He comes from a family with medical issues and experienced challenges growing up. The diagnostic impression is that the client has intense emotional distress from depression, anxiety, and schizoid tendencies exacerbated by substance abuse that is impairing his functioning.