1. The document discusses intellectual disability and specific learning disorder, outlining their definitions, diagnostic criteria, and assessment process.
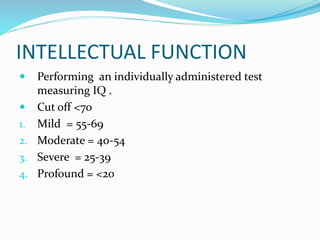
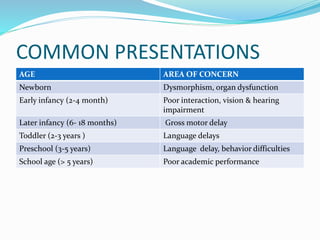
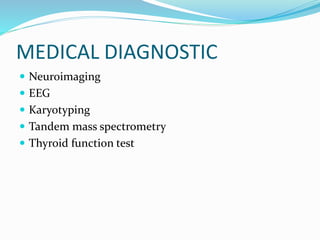
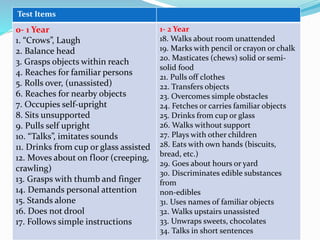
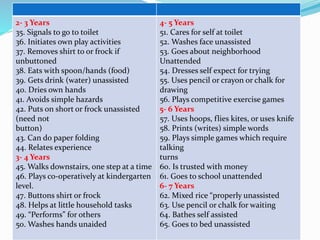
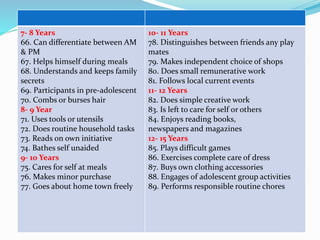
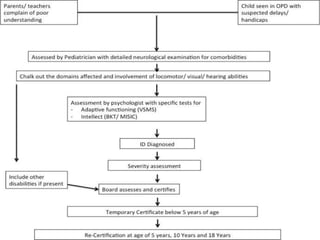
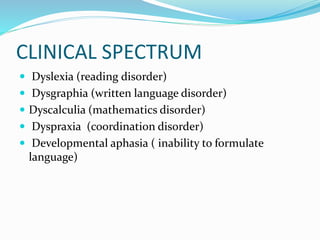
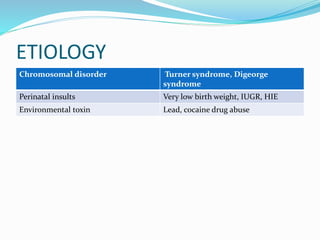
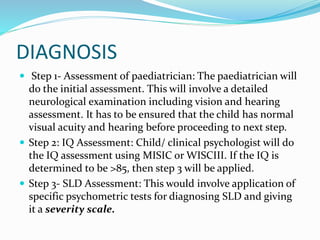
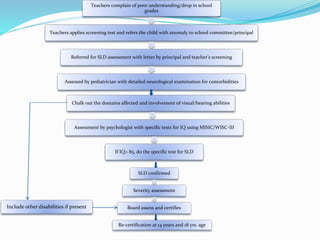
2. It describes assessing adaptive and intellectual functioning to diagnose intellectual disability, and using specific psychometric tests to identify learning deficits for specific learning disorder.
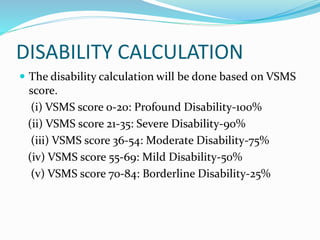
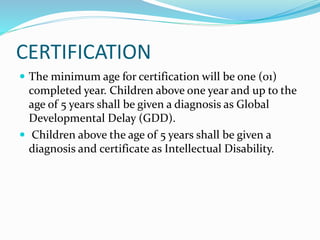
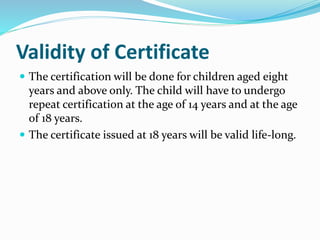
3. The certification process involves evaluations by medical and psychological professionals to determine the diagnosis and issue certificates of disability.