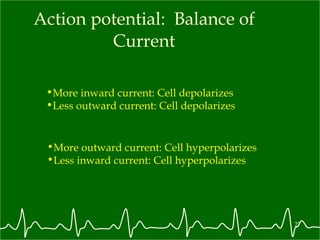
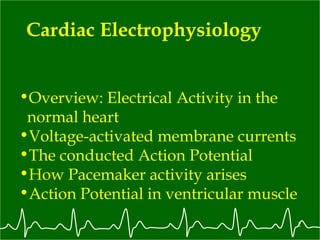
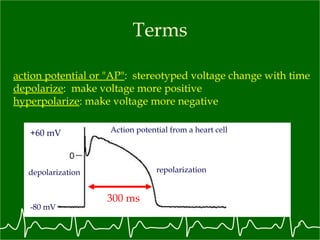
1. Cardiac electrophysiology involves the electrical activity in the heart, including the action potential and ion currents.
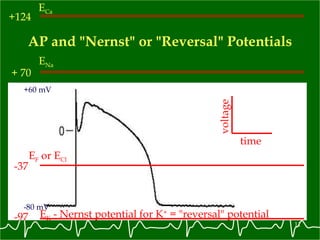
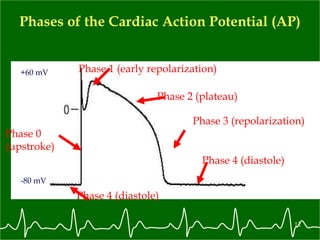
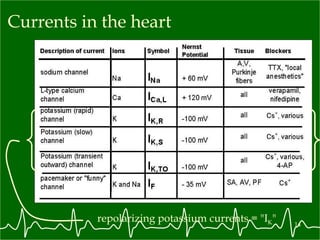
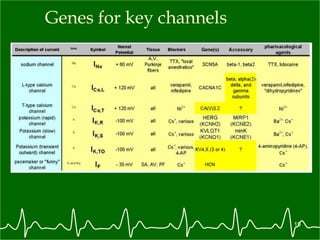
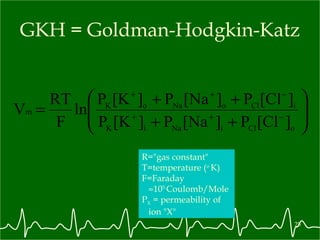
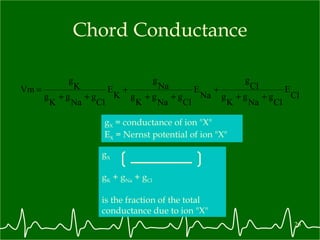
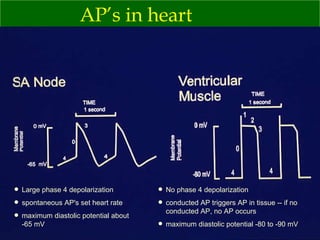
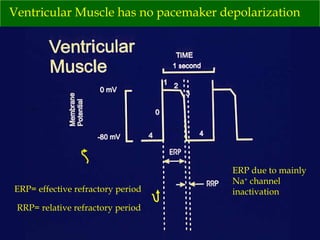
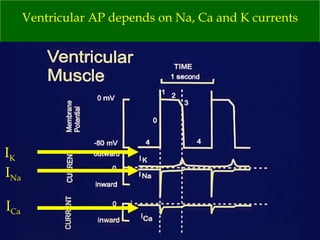
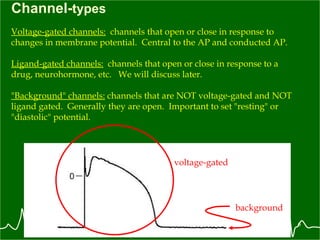
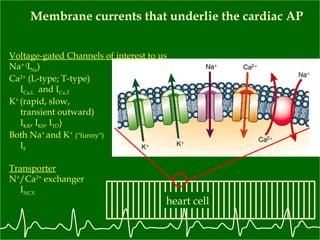
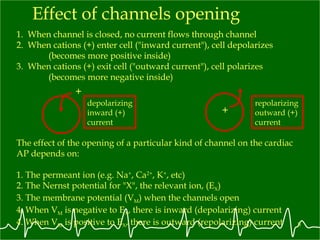
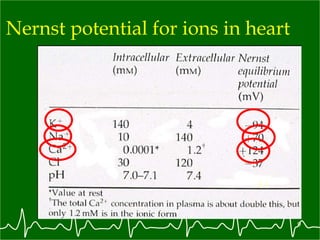
2. The cardiac action potential is initiated by the opening of fast sodium channels, followed by calcium and potassium channels.
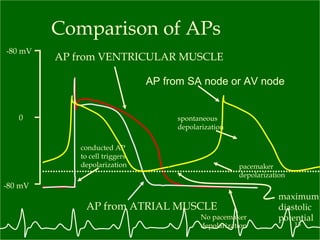
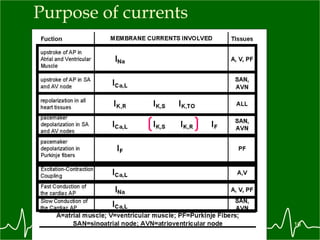
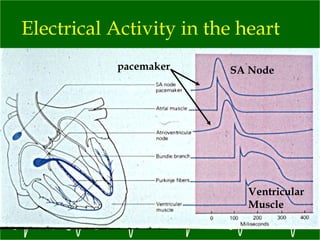
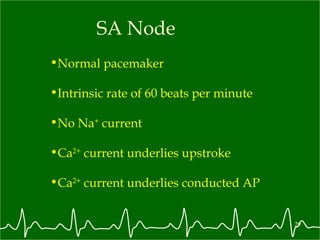
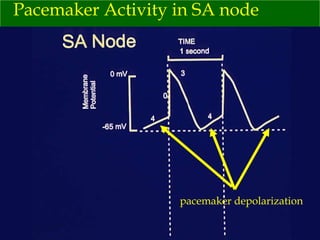
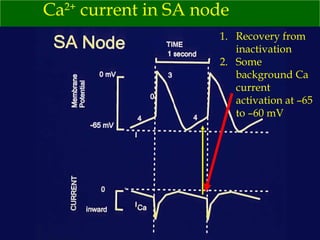
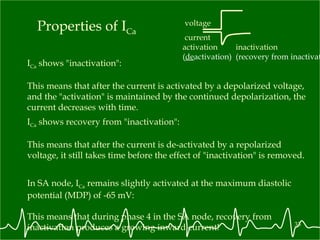
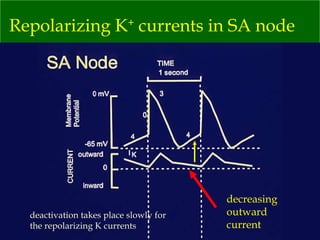
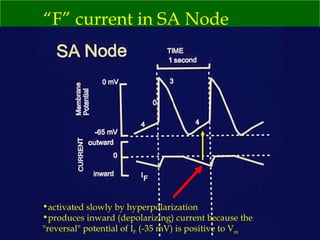
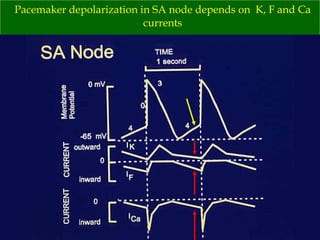
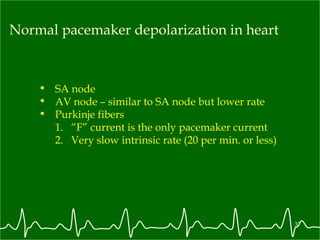
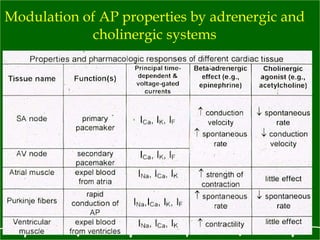
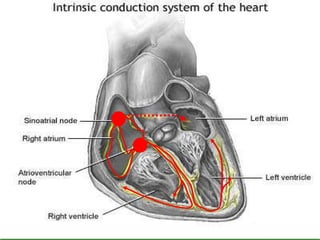
3. Pacemaker cells in the sinoatrial node generate spontaneous action potentials due to a balance of slow inward calcium and funny currents and delayed outward potassium currents.
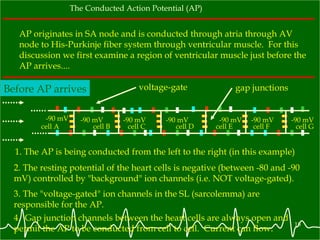
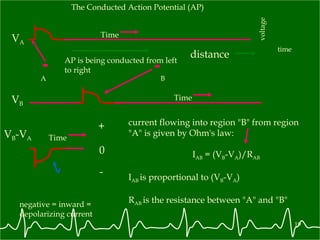
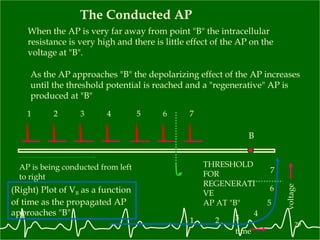
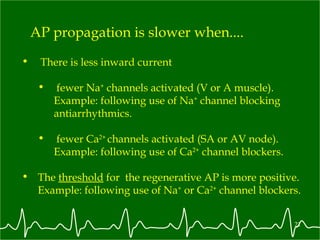
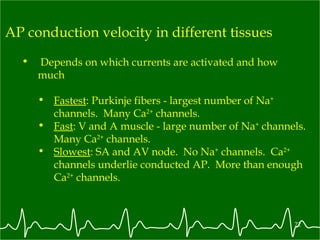
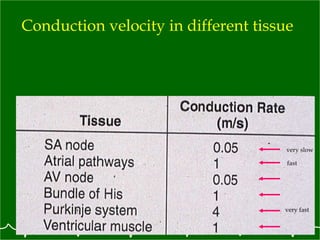
4. Action potentials propagate from pacemaker cells through the heart via gap junctions between cardiomyocytes. Propagation speed depends on the underlying ionic currents.
![Nernst Potential for Ion "X" if K o were 1 mM and K i were 100 mM then E K = -120 mV For a positive monovalent ion R="gas constant" T=temperature ( o K) Z=valence F=Faraday 10 5 Coulomb/Mole E X = 60 mV log ([X + ] o /[X + ] i ) .](https://image.slidesharecdn.com/cardiacelectrophysiology1498/85/Cardiac-Electrophysiology-10-320.jpg)