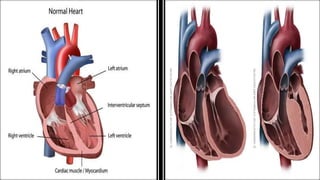
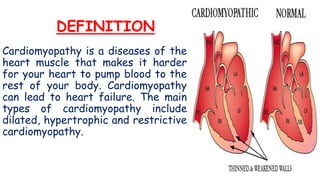
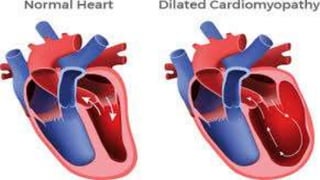
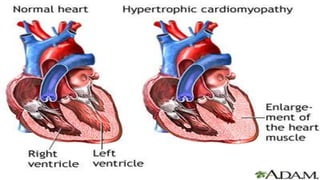
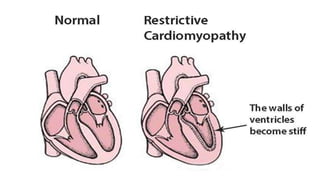
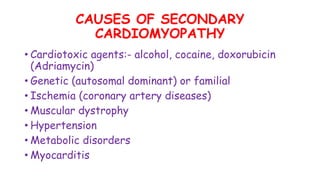
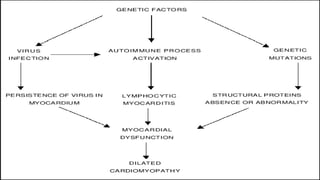
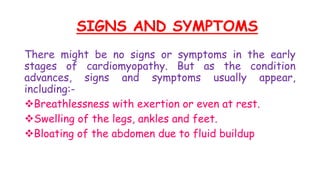
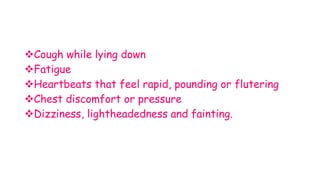
The document provides information about cardiomyopathy including its definition, types (dilated, hypertrophic, restrictive), causes, signs and symptoms, risk factors, complications, diagnostic tests, and medical, nursing, and surgical management. It discusses the pathophysiology and details of each type of cardiomyopathy and emphasizes lifestyle changes that can help prevent cardiomyopathy.