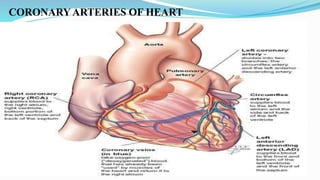
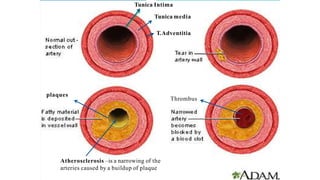
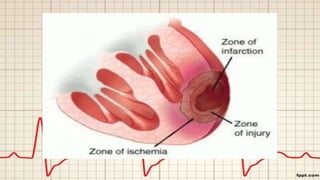
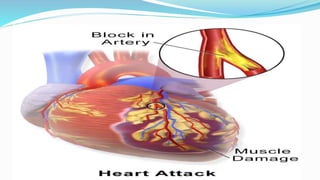
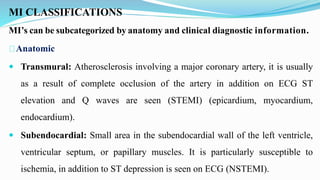
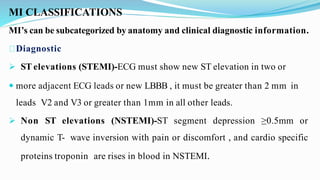
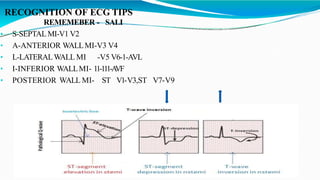
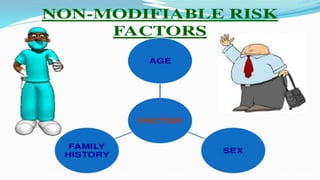
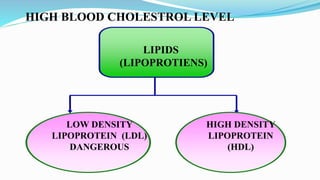
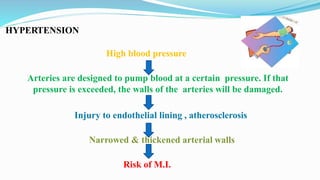
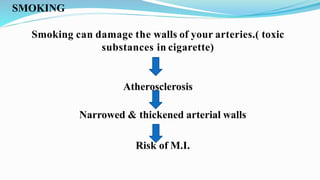
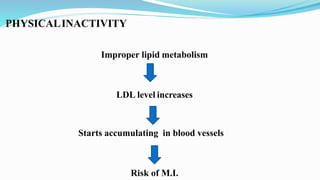
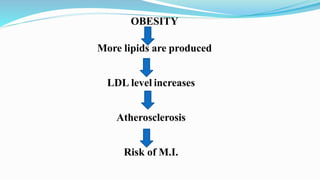
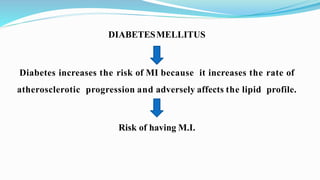
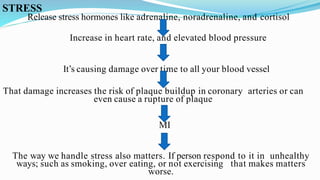
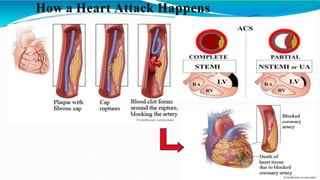
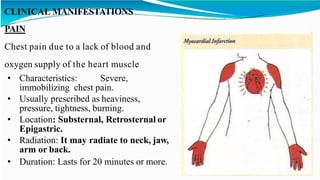
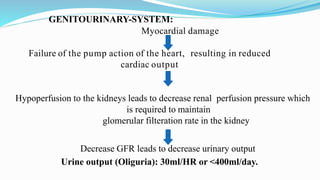
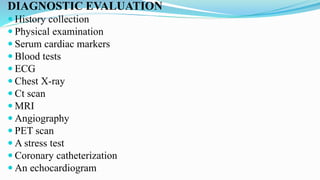
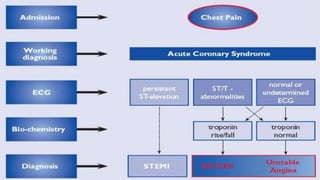
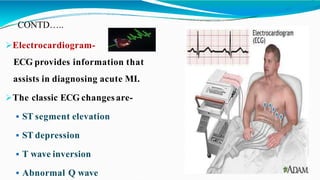
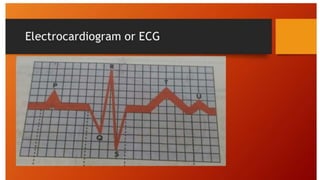
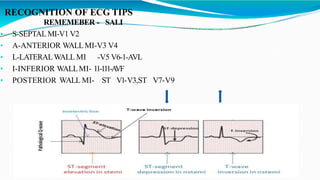
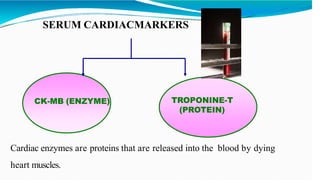
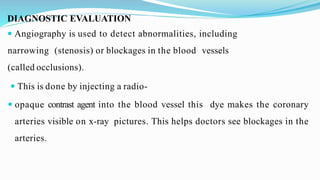
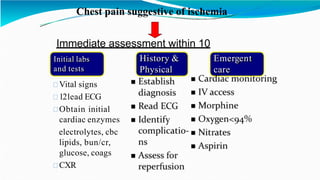
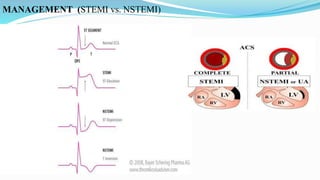
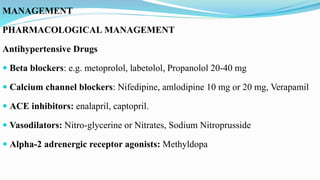
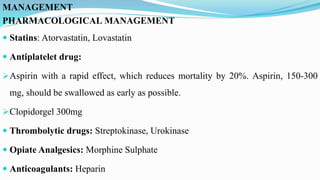
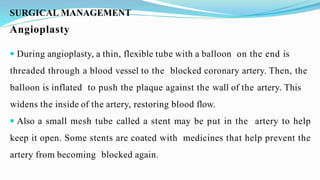
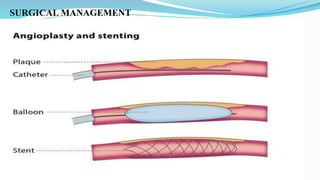
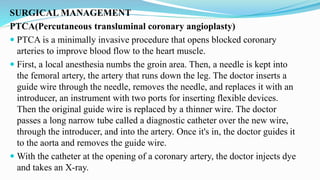
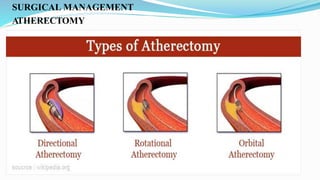
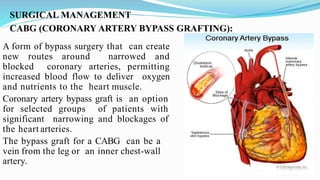
This document provides objectives and content about acute myocardial infarction (AMI) or heart attack. It begins with objectives of explaining AMI and its various aspects. It then defines AMI as reduced blood flow in a coronary artery due to atherosclerosis or thrombus. It discusses the incidence, classifications, risk factors like hypertension and smoking, etiological factors, pathophysiology of plaque buildup and thrombus formation blocking blood flow. It covers clinical features like chest pain, diagnostic evaluation including ECG, cardiac enzymes and angiography. It outlines management including pharmacological treatments, angioplasty, and other surgical procedures to reopen blocked arteries and restore blood flow to the heart.